Abstract
Objective
Unlike most muscular dystrophies that progress symmetrically at a constant rate, facioscapulohumeral muscular dystrophy (FSHD) is characterized by stepwise, asymmetric progression of muscle wasting, and weakness. Muscle tissue is progressively replaced by fat; however, its relation to preceding inflammation is unclear. In this longitudinal study of FSHD, we assessed muscle inflammation and fat replacement and their relation quantitatively. We also investigated whether fat replacement in muscle varies along its length.
Methods
Forty-five patients with FSHD were evaluated twice, 14 months apart. Using MRI sequences with short TI inversion recovery (STIR), we quantified the degree of STIR hyperintensity in muscles (≥ 2 SD above control intensity). STIR hyperintensities (STIR+) suggest edema or inflammation. We used Dixon MRI to quantify fat content.
Results
Of 370 thigh muscles, 83 were STIR+ at baseline and 103 at follow-up. The highest frequency of STIR+ was seen in muscles with inter-mediate fat content (40–60% fat). The progression of fat replacement was higher in STIR+ muscles (5.0 ± 4.0%) vs. STIR− muscles [2.3 ± 3.3% (P < 0.0001)]. In addition, muscles with severe STIR+ at baseline had a higher fat replacement progression than muscles with milder STIR+ (R = 0.39, P = 0.001). The fat content was higher in the distal part vs. proximal part of most muscles (P < 0.05). However, the progression of the fat replacement was uniform along the length of all the muscles.
Conclusion
Muscles with STIR+, indicating inflammation, have a faster progression of fat replacement than STIR− muscles, and the fat replacement progression correlated with the severity of STIR+.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Facioscapulohumeral muscular dystrophy type 1 (FSHD) is an inherited neuromuscular disease caused by contractions of D4Z4 repeats on chromosome 4q35, resulting in lost repression of the myotoxic protein, DUX4 [1]. Unlike most other muscular dystrophies, which are slowly progressive and symmetric, FSHD is characterized by stepwise, asymmetric progression of muscle wasting and weakness of facial and upper girdle muscles [2]. Abdominal, paraspinal, and lower extremity muscles are also involved [3]. There is no curative treatment of the disease and up to one-fourth of patients with FSHD become wheelchair-dependent [2, 3].
In the development of a treatment for FSHD, it is important to understand the pathophysiology of the disease. As in the other muscular dystrophies, muscle tissue is replaced by fat during the course of the disease. However, the rate of fat replacement and its relation to preceding inflammation of the muscles is unknown. In a recent MRI study of 45 patients with FSHD [4], we investigated the disease progression in back and leg muscles over 1 year and detected two modes of progression; one with a slowly progressive decline as found in other muscular dystrophies, but also another with a stepwise disease progression. Most muscles had a slow and widespread progression in fat replacement of 2.2% annually, while some had a faster progression of 9.9% annually [4]. It has been proposed that muscle inflammation contributes to the pathophysiology of FSHD and that it precedes the muscle destruction. Studies that have investigated muscle inflammation and fat replacement in FSHD have suggested that severe muscle inflammation predicts a faster fat replacement of muscle [5,6,7]. However, the link between muscle inflammation and fat replacement was unclear, since some inflamed muscles did not progress in fat content and other muscles progressed in fat content without prior inflammation. Muscle inflammation can be investigated using MRI sequences with short TI inversion recovery (STIR). STIR hyperintensities (STIR+) visualize edema and biopsies of STIR+ muscles have shown inflammatory changes [7, 8]. We hypothesized that muscle inflammation precedes the faster muscle degeneration seen in FSHD. We developed a quantifying method using STIR sequences that allowed us to identify and quantify the edematous changes in muscle that indicate inflammation. Furthermore, we quantified muscle fat content using Dixon MRI sequences, and investigated the relation between muscle inflammation and fat replacement in FSHD over 14 months.
To further shed light on the pathophysiology and disease progression in FSHD, we also investigated whether fat replacement in muscle varies along its length and if it progresses from one part to another.
Methods
Ethical approval
All participants gave their informed consent to participate prior to their inclusion and the study was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. The study was approved by the Danish National Committee on Health Research Ethics (approval number: H-3-2012-163, 41665, 43449) and registered at Clinicaltrials.gov (identifier: NCT02159612).
Study design and subjects
In this study, we present the results of new MRI analyses performed on the MR images of participants of a previous longitudinal MRI study that we performed at Copenhagen Neuromuscular Center, Rigshospitalet, Denmark from March 2013 to March 2015 [3, 4]. Forty-five patients with genetically verified FSHD type 1 were evaluated by MR scan twice, 436.3 ± 43 days apart (range 359–560 days).
MRI
We scanned all participants using a 3.0 T Siemens scanner (MAGNETOM Verio Tim System; Siemens AG, Erlangen, Germany). The MRI protocol for thighs and calves included localizers, T1-weighted images, and two-point Dixon, using parameters described before [4]. We also scanned the thighs with STIR sequences (field of view 400 mm, TE 29 ms, TR 3300 ms, and slice thickness 6.0 mm). The entire protocol was completed within 45 min.
Muscle fat content and STIR intensity
We mapped all thigh muscles manually on the slice corresponding to the middle of the thigh at baseline and follow-up. Muscle fat content was calculated using Dixon images by expressing the fat signal as a percentage of the total water and fat signal as described before [9]. The precision of the manual mapping has previously been established (Pearson product moment correlation: R = 0.976, P < 0.0001, n = 80) [4].
We developed a new method to quantify the degree of muscle edema using STIR images. High-signal intensities on STIR images, or STIR hyperintensities, indicate edema. In our method, we used histograms of the signal intensity of all pixels in a mapped muscle and determined the number of pixels above a defined upper reference limit, referred to as elevated pixels. Muscles with less than 2.5% elevated pixels were defined as being STIR-negative (STIR−). Muscles with more than 2.5% elevated pixels were defined as being STIR-positive (STIR+). The percentage of elevated pixels will also be referred to as the degree or severity of the hyperintensity.
We defined the upper reference limit using 121 unaffected FSHD muscles. These control muscles had no visually detectible STIR hyperintensities and had normal fat content (below 20%). The signal intensities of the control muscles were similar to healthy controls’ and were normally distributed. We, therefore, used control muscles from the patients with FSHD. The upper reference limit of signal intensity was set at 2 SD above the mean of the control muscles. The cut-off value of 2.5%, at which a muscle was considered to be STIR+, was based on the fact that, in a normal distribution, 95% of values lie within 2 SD of the mean, 2.5% in a lower tail, and 2.5% in an upper tail. The signal intensity of all images was normalized to an unaffected muscle.
Three months after analysis of all the scans, 19 random baseline and follow-up scans were re-analyzed showing a high level of reliability (Pearson product moment correlation: R = 0.977, P < 0.0001, n = 171). One trained evaluator (JRD) performed all the analyses using the Horos software.
All muscles were also evaluated visually on the STIR sequences assessing qualitatively the presence or absence of signal hyperintensity in each muscle. The evaluator was blinded to the quantitative determination of fat content and STIR intensity.
Proximal–distal gradient
In addition to the muscle mapping performed at 50% of the length of the right femur, we mapped quadriceps, rectus femoris, sartorius, and semimembranosus at 35 and 60% of the length of femur. In the calf, we mapped the right anterior and posterior tibialis muscles and the medial gastrocnemius muscle at slices corresponding to 25, 35, and 45% of the length of tibia. The images were analyzed by two evaluators using the Horos software (JRD and TK). Intraclass correlation coefficient was 0.998 (95% confidence interval 0.996–1.0).
Sub-groups of muscles
To be able to compare muscles with different fat content, progression of fat content and degree of STIR signal intensity, we grouped the muscles into sub-groups using cut-off values (Table 1). Shifting these values by ± 5% did not change the main results of this study.
Statistical analyses
Statistical analysis was performed using SPSS v25 and values are mean ± standard deviation (SD) unless otherwise stated. A P value of < 0.05 was considered significant.
ANOVA was used for investigating the proximal–distal gradient and the fat content progression from baseline to follow-up. P values were Bonferroni corrected.
Results
Muscle fat content and STIR intensity
Forty-three patients were included in the muscle inflammation and fat content analyses and nine thigh muscles were evaluated in each patient. Seventeen muscles were excluded from the analysis due to missing paired STIR or Dixon data, resulting in a total of 370 analyzed muscles.
Thirty-three patients had at least one STIR+ muscle at baseline and 34 at follow-up. Of all 370 muscles, 83 were STIR+ at baseline and 103 at follow-up. The muscles with the highest number of STIR+ lesions were the adductor magnus (nbaseline = 18; nfollow-up = 18), the long head of biceps femoris (nbaseline = 15; nfollow-up = 22), and semitendinosus (nbaseline = 15; nfollow-up = 18).
Whether a muscle was STIR+ or STIR− was also evaluated qualitatively by visual inspection. In 82% of the 370 muscles, the visual and the quantitative assessments showed agreement. In the majority (84%) of the 18% of muscles where the two methods showed discrepancy, the quantitative method detected STIR+ that was not visually detectible.
When investigating the evolution of the STIR hyperintensities from baseline to follow-up, we found that muscles with new STIR+ lesions and muscles with an increase in the severity of the hyperintensity had lower muscle fat content than the other muscles (Table 2; Fig. 1). The highest fat content was seen in muscles that were STIR+ at baseline and STIR− at follow-up. The majority of the muscles that remained STIR− from baseline to follow-up had muscle fat content below 30% or above 70%.
The distribution of STIR-negative and STIR-positive muscles according to their fat content at baseline in patients with facioscapulohumeral muscular dystrophy. Histograms of the distribution of STIR-negative (STIR–) and STIR-positive (STIR+) muscles according to their fat content at baseline. The ellipses show the distribution of muscles according to their STIR status at follow-up. Also see Table 2. ↑ increase in STIR signal hyperintensity from baseline to follow-up; ↓ decrease in signal hyperintensity from baseline to follow-up
All muscles had a significant increase in fat content from baseline to follow-up of 2.89% annually (P < 0.0001), which is about a 14 times higher rate than the 0.2% annual increase reported in healthy adults [10]. The absolute progression of fat replacement was higher in STIR+ muscles, 5.0 ± 4.0%, than in STIR− muscles, 2.3 ± 3.3% (P < 0.0001). There was a weak correlation between the severity of the hyperintensity at baseline and the progression of fat replacement among STIR+ muscles, i.e., as the severity of the hyperintensity increased, the fat replacement also increased (R = 0.39, P = 0.001; Fig. 2).
The relation between STIR signal intensity and progression of muscle fat replacement in patients with facioscapulohumeral muscular dystrophy. The relation between STIR signal intensity at baseline (percentage of elevated pixels) and progression of muscle fat content over 14 months in 370 muscles in patients with facioscapulohumeral muscular dystrophy
Arranging muscles by their fat content showed an hourglass pattern with a few muscles with inter-mediate fat contents [4]. The inter-mediate phase muscles, with fat contents from 40 to 60% at baseline, had a higher progression of fat replacement vs. muscles with lower or higher fat fractions (P < 0.0001; Fig. 3a). The progression was 6.1 ± 5.3% in the inter-mediate phase muscles compared to 3.1 ± 3.4% in muscles with fat content below 40%, and 1.6 ± 2.8% in muscles with fat content above 60%. Muscles with inter-mediate fat content also had a higher percentage of STIR+ muscles (P < 0.05). Forty-two percent of the inter-mediate phase muscles were STIR+ compared to 22% in muscles with lower fat content and 18% in muscles with higher fat content (Fig. 3b).
Fat replacement progression and percentages of muscles with different degree of STIR signal intensity in facioscapulohumeral muscular dystrophy. a The progression in muscle fat content over 14 months in muscles with low (< 40%), inter-mediate (40–60%) and high (> 60%) fat content at baseline. b The distribution of muscles with different STIR signal intensities in muscles with low (< 40%), inter-mediate (40–60%) and high (> 60%) fat content at baseline. c The distribution of muscles with different STIR signal intensities in muscles with slow (< 5%) vs fast (> 5%) progression of fat replacement over 14 months. The box plot (a) includes the 25th–75th percentiles, the mid line indicates the median, whiskers are the 5th–95th percentiles, and black dots are outliers. The numbers to the right of the columns in b and c indicate the absolute number of muscles. STIR– STIR-negative muscles, STIR+ STIR-positive muscles, STIR+, STIR++ and STIR+++ degree of the STIR hyperintensity (see also Table 1)
We have previously demonstrated two modes of fat replacement progression in FSHD (slow and continuous vs. fast and stepwise) [4]. When dividing muscles in two groups according to the rate of progression, we found that the percentage of STIR+ muscles was 16% in muscles with a fat replacement progression below 5% and 44% in muscles with a progression above 5% (P < 0.0001; Fig. 3c). The hyperintensity was more severe in the STIR+ muscles with the faster progression (13.3 ± 10.7% elevated pixels) compared to STIR+ muscles with the slower progression (6.5 ± 4.6% elevated pixels; P < 0.05).
Proximal–distal gradient
Patients with missing or unusable MRIs on one or more levels at any time point were excluded from the relevant muscle analysis. As a result, 33 patients were included in the quadriceps femoris and sartorius analyses, 34 in the rectus femoris and semitendinosus analyses, 41 in the tibialis anterior analysis, and 42 in the tibialis posterior and gastrocnemius medialis analyses.
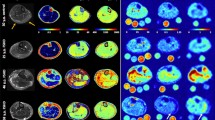
There was an increase in muscle fat content from baseline to follow-up in all the muscles (P < 0.05; Fig. 4). There was also significantly different fat content along the length of all muscles in the thigh and calves, except the tibialis posterior muscle, at both baseline and follow-up (P < 0.05). This difference was most commonly found between the most proximal and distal measuring levels, but differences were also present between the mid-level and the most proximal (semitendinosus and gastrocnemius medialis muscles) or distal level (quadriceps, tibialis anterior, and gastrocnemius medialis muscles). The fat content increased from the proximal part of the muscle to the distal part.
To investigate whether the progression of fat replacement from baseline to follow-up was faster in some parts of the muscles than in other, we tested if there was an interaction between the level of measurement (proximal, middle, and distal) and time point (baseline and follow-up). We found no interaction, neither individually (P = 0.26–0.97) nor when all muscles were grouped (P = 0.32). These results indicate that the rate of fat replacement was uniform along the length of the muscles.
Muscle fat replacement, STIR intensity, and a proximal–distal gradient
Muscles with a faster progression of fat replacement (> 5%) had a steeper proximal–distal gradient than muscles with slower progression (< 5%) (P = 0.001).
The gradient was also steeper in STIR+ muscles compared to STIR– muscles (P = 0.007; Fig. 5). The progression of fat replacement from baseline to follow-up was similar at all the measurement levels in both STIR+ and STIR– muscles (P = 0.33).
Discussion
In this study, we investigated the pathophysiology of FSHD in 45 patients over 14 months. We quantified STIR hyperintensities, indicating inflammation, and fat content in thigh muscles and investigated its relation and progression over 14 months. We also investigated the progression of fat replacement of muscle along the length of the thigh and calf. All muscles had a significant increase in fat content over the 14 months. This progression of fat replacement was more than twice as fast in STIR+ muscles compared to STIR– muscles and increased with the severity of the hyperintensity. The fat content of most thigh and calf muscles was higher in the distal part of the muscle than more proximally. This proximal–distal gradient was steeper in STIR+ muscles compared to STIR– muscles. The progression of the fat replacement, however, was uniform along the length of all the muscles, irrespective of STIR hyperintensity.
Emerging treatment options for FSHD call for accurate and sensitive outcome measures that can capture changes or effects of interventions [2]. MRI has gained a lot of attention in this respect, and MRI with STIR sequences has been proposed as a prognostic outcome measure [5, 11]. STIR hyperintensities (STIR+) visualize edema, which is a marker of inflammation. In accordance with this, biopsies of STIR+ muscles show inflammatory changes [8]. STIR+ appears to precede the replacement of muscle by fat in FSHD, and preliminary results indicate that very bright STIR+ areas evolve more rapidly toward fat [5, 6, 11]. A faster replacement of muscle by fat has also been associated with inter-mediate fat content in muscles [4, 11]. Arranging muscles by their fat content shows an hourglass pattern with a few muscles carrying inter-mediate fat content [4, 11]. These inter-mediate muscles have a faster progression of fat replacement. It has been suggested that, once a muscle reaches an inter-mediate fat fraction, it accelerates towards complete fat replacement and that muscle inflammation might act as a trigger for this process [11].
In our study, we found that the highest percentage of STIR+ muscles were among the inter-mediate muscles, and thus, among the muscles with fat content at baseline between 40 and 60%. Almost half of the inter-mediate muscles were STIR+ compared to approximately one-fifth of the muscles with lower or higher fat content (Fig. 2b). The mean fat fraction of new STIR+ lesions at follow-up was 30%, compared to 66% in resolved lesions (Table 2). The majority of the STIR– muscles had fat fractions below 30% or above 60%, suggesting that they were either relatively unaffected or completely fat replaced. STIR+ muscles had a faster progression of fat replacement of 5.0% compared to 2.3% in STIR– muscles. Furthermore, as the severity of the STIR hyperintensity increased, the fat replacement progression also increased (Fig. 5). All these findings support the notion that muscle inflammation contributes to the pathophysiology of muscle destruction in FSHD and that inflammation may act as a biological trigger for the faster disease progression.
The relationship between inflammation and fat replacement has previously been suggested by three longitudinal studies [6, 11, 12]. In cohorts of 9–15 patients with FSHD followed for 4 months to 2 years, these studies identified a larger progression of fat replacement in STIR+ muscles. However, the link between muscle inflammation and fat replacement was unclear, since some STIR+ muscles did not progress in fat content and other muscles progressed in fat content without prior STIR+ lesion. The lack of conclusive results from these studies might be explained by the small number of patients examined. Furthermore, two of the studies used qualitative scoring to evaluate muscle inflammation and fat content which is subjective and observer-dependent [6, 12]. The study investigated the inflammation and fat content quantitatively, investigated 11 patients twice, 4 months apart, and only identified six muscles with inflammation [11]. In our large study, we developed a quantitative method to evaluate muscle inflammation, reflected by elevated STIR signals, and identified 83 STIR+ muscles (22%) at baseline and 103 (28%) at follow-up. The high number of STIR+ muscles, and the way which STIR was quantified in our study allowed us to better investigate the relation between inflammation and progression of fat replacement in muscle, and could compare sub-groups of muscles with different fat content and progression rates. The higher frequency of STIR+ muscles observed in our study when compared to the previous reports is likely explained by the different methods used [5, 8, 11,12,13,14]. Quantitative methods are generally more sensitive to change than the qualitative methods and are able to detect changes before the changes are visually detectible [15].
Even though the percentage of STIR+ muscles was more than twice as high in muscles with a faster fat replacement progression (> 5%) than muscles with a slower progression (< 5%) in our study, more than half of the muscles with the faster progression were STIR– at baseline. Whether these STIR– muscles with fast muscle destruction were STIR+ at another time before or after the baseline examination, or there are other factors affecting muscle destruction in FSHD is impossible to determine based on two assessments. To be able to identify the true relation between muscle inflammation and fat replacement, and to fully evaluate the potential of STIR as an outcome measure, multiple assessments are necessary.
In line with the previous studies, we found that the fat content increased from proximal to distal in the rectus femoris, quadriceps femoris, sartorius, semitendinosus, tibialis anterior, and gastrocnemius medialis muscles (Fig. 3) [11, 16]. Tibialis posterior, however, had no proximal–distal gradient. While all the muscles with a proximal–distal gradient had mean fat fractions above what is seen in healthy people, tibialis posterior had a mean fat fraction similar to healthy. Tibialis posterior is, thus, a relatively unaffected muscle in patients with FSHD, which may explain the lack of a proximal–distal gradient.
The proximal–distal gradient was steeper in muscles with a faster progression of fat replacement (> 5%) compared to muscles with slower progression (< 5%) and in STIR+ thigh muscles compared to STIR– muscles (Fig. 4). The gradient remained constant over time in all the muscles, also in STIR+ muscles. These results indicate that the muscle degeneration in FSHD initiates in the distal part of the muscle and accelerates evenly throughout the muscle. This is important to keep in mind when designing longitudinal natural history and interventional studies.
A limitation of our study includes the relatively short follow-up time of 14 months. In our study, 39 of 83 STIR+ muscles did not change from baseline to follow-up and a previous study has observed stable STIR+ signal for over 3 years [6]. We investigated thigh muscles in this study even though upper girdle muscles often are more severely involved in patients with FSHD. However, it has previously been shown that the frequency of STIR+ muscles in upper girdle muscles is lower than in the lower limbs [5]. In less than 3% of patients with FSHD, STIR+ muscles occur as a lone phenomenon in the muscles of the upper girdle, compared to 28% in lower limb muscles [5]. The participants in our study were only examined twice, but repeated measures are required to more definitively associate muscle fat replacement with inflammation. Finally, even though STIR+ muscles have been shown to have pathological changes of muscle inflammation accompanied by a significant upregulation of genes involved in the muscle inflammatory disease process, STIR hyperintensity is relatively non-specific [17]. In addition to edema and inflammation, it may also reflect cell necrosis, denervation, sarcoplasmic leakiness, and myocyte swelling [18].
In conclusion, we describe the relation between STIR hyperintensities and fat content in muscle investigated with quantitative MRI. Muscles with STIR hyperintensities had a faster progression of fat replacement than muscles without STIR hyperintensities. Furthermore, the fat replacement progression was faster in muscles with severe STIR hyperintensities compared to the muscles with milder STIR hyperintensities. Since STIR hyperintensities indicate inflammation, these results suggest that muscle inflammation contributes to the faster muscle destruction seen in FSHD and may very well act as a trigger function.
Abbreviations
- ANOVA:
-
Analysis of variance
- FSHD:
-
Facioscapulohumeral muscular dystrophy
- SD:
-
Standard deviation
- STIR:
-
Short TI inversion recovery
- STIR+:
-
STIR hyperintensity
- STIR−:
-
No STIR hyperintensity
References
Tawil R, van der Maarel SM, Tapscott SJ (2014) Facioscapulohumeral dystrophy: the path to consensus on pathophysiology. Skelet Muscle 4:12. https://doi.org/10.1186/2044-5040-4-12
Hamel J, Tawil R (2018) Facioscapulohumeral muscular dystrophy: update on pathogenesis and future treatments. Neurother J Am Soc Exp Neurother. https://doi.org/10.1007/s13311-018-00675-3
Dahlqvist JR, Vissing CR, Thomsen C, Vissing J (2014) Severe paraspinal muscle involvement in facioscapulohumeral muscular dystrophy. Neurology 83:1178–1183. https://doi.org/10.1212/WNL.0000000000000828
Andersen G, Dahlqvist JR, Vissing CR et al (2017) MRI as outcome measure in facioscapulohumeral muscular dystrophy: 1-year follow-up of 45 patients. J Neurol 264:438–447. https://doi.org/10.1007/s00415-016-8361-3
Tasca G, Monforte M, Ottaviani P et al (2016) Magnetic resonance imaging in a large cohort of facioscapulohumeral muscular dystrophy patients: pattern refinement and implications for clinical trials. Ann Neurol. https://doi.org/10.1002/ana.24640
Ferguson MR, Poliachik SL, Budech CB et al (2018) MRI change metrics of facioscapulohumeral muscular dystrophy: stir and T1. Muscle Nerve 57:905–912. https://doi.org/10.1002/mus.26038
Wang LH, Friedman SD, Shaw D et al (2018) MRI-informed muscle biopsies correlate MRI with pathology and DUX4 target gene expression in FSHD. Hum Mol Genet. https://doi.org/10.1093/hmg/ddy364
Frisullo G, Frusciante R, Nociti V et al (2011) CD8(+) T cells in facioscapulohumeral muscular dystrophy patients with inflammatory features at muscle MRI. J Clin Immunol 31:155–166. https://doi.org/10.1007/s10875-010-9474-6
Ma J (2008) Dixon techniques for water and fat imaging. J Magn Reson Imaging JMRI 28:543–558. https://doi.org/10.1002/jmri.21492
Dahlqvist JR, Vissing CR, Hedermann G et al (2017) Fat replacement of paraspinal muscles with aging in healthy adults. Med Sci Sports Exerc 49:595–601. https://doi.org/10.1249/MSS.0000000000001119
Janssen BH, Voet NBM, Nabuurs CI et al (2014) Distinct disease phases in muscles of facioscapulohumeral dystrophy patients identified by MR detected fat infiltration. PloS One 9:e85416. https://doi.org/10.1371/journal.pone.0085416
Friedman SD, Poliachik SL, Otto RK et al (2014) Longitudinal features of STIR bright signal in FSHD. Muscle Nerve 49:257–260. https://doi.org/10.1002/mus.23911
Leung DG, Carrino JA, Wagner KR, Jacobs MA (2015) Whole-body magnetic resonance imaging evaluation of facioscapulohumeral muscular dystrophy. Muscle Nerve 52:512–520. https://doi.org/10.1002/mus.24569
Lareau-Trudel E, Le Troter A, Ghattas B et al (2015) Muscle quantitative MR imaging and clustering analysis in patients with facioscapulohumeral muscular dystrophy type 1. PloS One 10:e0132717. https://doi.org/10.1371/journal.pone.0132717
Willis TA, Hollingsworth KG, Coombs A et al (2013) Quantitative muscle MRI as an assessment tool for monitoring disease progression in LGMD2I: a multicentre longitudinal study. PloS One 8:e70993. https://doi.org/10.1371/journal.pone.0070993
Kan HE, Scheenen TWJ, Wohlgemuth M et al (2009) Quantitative MR imaging of individual muscle involvement in facioscapulohumeral muscular dystrophy. Neuromuscul Disord NMD 19:357–362. https://doi.org/10.1016/j.nmd.2009.02.009
Tasca G, Pescatori M, Monforte M et al (2012) Different molecular signatures in magnetic resonance imaging-staged facioscapulohumeral muscular dystrophy muscles. PloS One 7:e38779. https://doi.org/10.1371/journal.pone.0038779
Carlier PG, Marty B, Scheidegger O et al (2016) Skeletal muscle quantitative nuclear magnetic resonance imaging and spectroscopy as an outcome measure for clinical trials. J Neuromuscul Dis 3:1–28. https://doi.org/10.3233/JND-160145
Acknowledgements
The authors thank Poul Henrik Frandsen, radiologist, Department of Diagnostic Radiology, Rigshospitalet, for his helpful advice in setting up the MRI protocol. This study has been funded by the Augustinus foundation.
Author information
Authors and Affiliations
Contributions
JRD: conception and design of the study, acquisition and analysis of data, drafting the text, and preparing the figures. GA: conception and design of the study, acquisition of data, and analysis of data. TK: acquisition and analysis of data. CV: acquisition and analysis of data. CT: design of the study and analysis of data. JV: conception and design of the study, design of manuscript, and reviewing.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest related to this study.
Rights and permissions
About this article
Cite this article
Dahlqvist, J.R., Andersen, G., Khawajazada, T. et al. Relationship between muscle inflammation and fat replacement assessed by MRI in facioscapulohumeral muscular dystrophy. J Neurol 266, 1127–1135 (2019). https://doi.org/10.1007/s00415-019-09242-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09242-y