Abstract
Background
Neuromyelitis optica spectrum disorder (NMOSD) is a B-cell-mediated disease with autoimmunity towards the astrocyte water channel aquaporin-4 (AQP-4) in the central nervous system.
Objective
To assess the long-term safety and efficacy in NMOSD patients receiving maintenance therapy with B-cell-depleting agent rituximab for more than 2 years.
Method
NMOSD patients were included prospectively from 2014 to 2018 and received continuous cycles of rituximab infusions biannually. Incidence of adverse events (AE), serious AEs (SAE), and infusion-related AEs were evaluated through monthly phone calls and neurological examination every 4 months.
Results
A total of 44 NMOSD patients were included, of those 30 were treatment naive (68%). The mean age was 37.2 years with 79.5% females. With overall observation period of 31.6 ± 7.3 months (24–48 months), tolerability was assessed as satisfactory in most cases. We observed infusion reactions (mostly mild) in 31.8% of patients and 31.8% never experienced any AEs after a mean 5.1 cycles of rituximab therapy. Rituximab was also beneficial in terms of improvement in relapse rate (from 0.26 ± 0.54 to 0, P = 0.003) and Expanded Disability Status Scale (from 4.1 ± 1.8 to 3.1 ± 1.8, P < 0.001). Stratification according to AQP4-IgG serostatus showed no difference between groups.
Conclusion
Rituximab treatment is well tolerated, safe, and efficacious with a minor risk of mild infusion reactions for NMOSD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuromyelitis optica spectrum disorder (NMOSD) is an autoimmune disease of the central nervous system (CNS) that mainly affects the optic nerve and spinal cord [1]. The majority of patients experience a relapsing course and frequent attacks lead to increasing disability [2]. Several studies indicate a crucial role for B cells in NMOSD pathogenesis [3]. An immunoglobulin G (IgG) autoantibody specific for the astrocyte water channel aquaporin-4 (AQP4) is detected in most NMOSD patients [3]. Depletion of B cells is, therefore, a valid treatment approach for the disease [1, 4, 5].
Rituximab, a chimeric anti-CD20 monoclonal antibody, is a maintenance treatment option for NMOSD patients [6]. During the maturation process, B cells express CD20 antigen, the production of which ceases in mature plasma cells [7, 8]. Rituximab primarily targets naïve and memory B cells through (a) antibody-dependent cytotoxicity, (b) complement-associated cytotoxicity, and (c) inducing apoptosis in the targeted cells [9]. Rituximab has through suppression of the B-cell population an effect on neurological autoimmune disorders driven by B-cell dysregulation [10] such as myasthenia gravis [11]. For treatment of other diseases, the most frequently reported side effects included fever, chills, bronchitis, headache, nausea, vomiting, hypotension, thrombocytopenia and neutropenia [12].
There is no curative treatment for NMOSD and rituximab as an immunosuppressive agent offers an option; however, there is presently insufficient evidence on long-term safety and efficacy of rituximab treatment. In this prospective study, we registered long-term tolerability, safety and efficacy of rituximab therapy in NMOSD patients.
Materials and methods
Study population
In a prospective study from 2014 to 2018, NMOSD patients referred to the multiple sclerosis (MS) and related disorders clinic at Kashani University Hospital in Isfahan, Iran, were evaluated for inclusion in the study. Around 2% of the patients referred to this center are usually diagnosed with NMOSD. The NMOSD diagnosis was based on the international consensus diagnostic criteria defined by Wingerchuk et al. [13]. NMOSD patients that received rituximab treatment during the study period were enrolled consecutively in the study. Patients with prior or concomitant diseases that prompted the use of rituximab were excluded from the study. Upon enrollment, written informed consent was provided from all participants; the study was approved by the research ethics committee of the Isfahan University of Medical Sciences (Approval Code: IR.MUI.RSEARCH.REC.1397.171).
Study protocol
Immunosuppressive therapies such as rituximab may contribute to the increased risk of infection. Therefore, patient’s vaccination status was evaluated and confirmed prior to treatment to prevent certain infections. AQP4-IgG was determined for each patient prior to study enrollment using a commercially available indirect immunofluorescence kit (Euroimmun, Lübeck, Germany) [14].
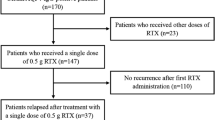
The rituximab treatment sessions were performed in compliance with established standard protocols; briefly, in the first session the patient received 500 mg rituximab (Zytux, AryoGen Pharmed Company, Iran) delivered in 500 cc of 0.9 sodium chloride via intravenous line for 1 h, each week for 4 weeks (2 g in total) followed by 1 g of rituximab received divided for two consecutive weeks (500 mg/week) every 6 months. Before each infusion, patients received 4 mg of oral chlorpheniramine and 100 mg of intravenous hydrocortisone to minimize hypersensitivity reactions.
Patients were seen in the clinic for neurological examination and safety evaluation every 4 months as well as prior to rituximab injection sessions. They were also followed up monthly via phone calls throughout the entirety of their treatment period especially for evaluation of safety and unwanted outcomes/events. A previously determined checklist of unwanted reactions and side effects was collected on each follow-up session (Supplementary File 1). This check list was designed based on previous reports on the side effects of rituximab [15, 16]. The occurrence of infections, malignancies, or any unexpected side effects was documented. All infections were noted as adverse event (AE) or serious AE (SAE), if they required hospitalization. Data from routine physical examinations, as well as annualized relapse rate (ARR) and extended disability status scale (EDSS), performed by a neurologist, were also registered for each patient.
Statistical analysis
Descriptive statistical methods were used to report frequencies and distribution of the results as well as means ± standard deviation (SD). Categorical data were analyzed using a cross-tabulation and chi-square; Simple T test and paired T test or their non-parametric equals were used for analysis of means among numerical data. Pearson analysis was used to assess correlations between numerical data. P values less than 0.05 were considered statistically significant. All statistical analysis was performed using the IBM SPSS software version 23.
Results
Baseline demographics and disease characteristics
A total of 46 patients were included in the study initially. 44 patients were followed up successfully. A 64-year-old male, seronegative, with previous chronic obstructive pulmonary disease expired due to a case of complicated pneumonia 1 month after initiation of the treatment. This patient was hospitalized with complaint of respiratory distress and died after 10 days because of hospital-acquired pneumonia with influenza superinfection in spite of checked vaccination before initiation of treatment. Also, a 33-year-old female, seronegative, presented severe anaphylactic reaction during the first infusion session and was switched to other medications.
The patients had an overall observation period of 31.6 ± 7.3 months (ranging from 24 to 48 months). The mean age was 37.2 ± 10.4 years with 35 female patients out of 44 subjects (79.5%). The mean disease duration was 6.3 ± 4.1 years and the mean number of rituximab treatment cycles was 5.1 ± 1.2. Table 1 presents baseline demographic and disease data in the study population.
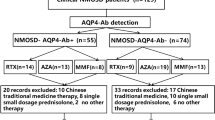
Serostatus and adverse events
The patients were stratified according to AQP4-IgG serostatus, and 14 patients (31.8%) were AQP4-IgG seropositive and were predominantly female (13 out of 14 cases). Seropositive and seronegative patients did not differ significantly with regard to gender, duration of therapy, baseline annualized relapse rates, baseline EDSS, and neurological presentation of disease (P = 0.135, P = 0.293, P = 0.809, P = 0.857, and P = 0.618, respectively). Seronegative patients found to be younger (34.9 ± 8.5 compared to 42.7 ± 12.6 years; P = 0.031) and had shorter duration of disease (5.3 ± 3.7 compared to 8.6 ± 4.2 years; P = 0.011) compared to seronegative subjects (Table 1).
Comparing the occurrence of reported AEs in each separated category resulted in no statistically significant difference between seropositive and seronegative patients (Table 2). Twenty seronegative patients (66.7%) and ten seropositive patients (71.4%) had reported experiencing at least one AE (P = 0.752). Moreover, comparing the mean total number of reported AEs in seropositive (14 ± 1.6) and seronegative (30 ± 2) patients revealed no difference (P = 0.907).
Tolerability and safety
After initiation of treatment, tolerability was satisfactory in almost all cases. Altogether, 82 episodes of AE were documented in 44 patients who were followed up during the study. As stated earlier, one of our cases died because of previous pulmonary disease and complicated respiratory infections 1 month after the first cycle of rituximab therapy. Among the 44 cases who were followed at least 24 months, none of the reported AE were found to be serious or life threatening.
In general, 31.8% of the patients never experienced any side effects or reactions and in 25% of the cases there was only one account of AE reported throughout the study. Particularly, minor uncomplicated infections were reported in 31.8% of the patients none of which required hospitalization. These infections mostly involved urinary tract and respiratory tract in a few cases (Table 2). There were no reported accounts of SAE such as thrombocytopenia, hemolytic anemia, encephalitis, Guillain–Barre syndrome, hepatitis, primary varicella-related infections, malignancies or neutropenia in any of the patients during the follow-up period.
Minor infusion-related reactions were reported in 31.8% of the cases. These reactions were all self-limited and were minimized by administration of chlorpheniramine and hydrocortisone. There was only one account of severe hypersensitivity reaction as mentioned above and she was switched to another therapy at the first rituximab cycle.
There was no significant correlation between the mean treatment duration and the mean total number of AEs (r = − 0.01, P > 0.05). Table 3 shows the frequency and distribution of AEs based on the treatment longevity. Figure 1 presents the frequency of AE episodes for each patient in the context of treatment duration.
Efficacy outcomes
Regarding treatment efficacy, the mean of EDSS decreased from 4.1 ± 1.8 to 3.1 ± 1.8 after 2–4 years of rituximab therapy (P < 0.001). At baseline, 34 patients were relapse free (77.3%) while at the last follow-up, they had all been relapse free in the past year (P < 0.001). The mean ARR decreased from 0.26 ± 0.54 to 0 after 2–4 years of rituximab therapy (P = 0.003). As presented in Table 1, no difference was found in the mean EDSS and ARR between seropositive and seronegative patients at the end of study (P = 0.070 and P = 1, respectively) (Table 1). Moreover, comparing the mean reduction ratio in EDSS (EDSS difference divided by baseline EDSS) showed no statistically significant difference (0.070 ± 0.28 in seropositive patients and 0.264 ± 0.25 in seronegative patients, P = 0.091).
Discussion
This prospective study describes the tolerability, safety and efficacy of rituximab as maintenance therapy among NMOSD patients, independent of AQP4-IgG serostatus, throughout a long-term follow-up beyond 24 months. Rituximab was well tolerated in most cases with satisfactory safety and proven effect of treatment via reduced relapses (ARR) and disability (EDSS). The safety of rituximab in NMOSD has not been widely investigated and most available data come from small studies or limited follow-up periods [4]. In the current study, about one-third of our patients experienced minor infections of urinary and respiratory tract and non-serious infusion-related reactions were also observed in one-third of cases. A total of 31.8% did not report of any AEs following rituximab therapy.
A recent metanalysis of 438 NMOSD patients, mostly seropositive, with a mean follow-up of 27.5 months (range 3–272 months) reported AEs in 114 patients (26%) [17]. Among the reported AEs, infusion-related AEs and infections were the most common (10.3% and 9.1%, respectively) [17]. However, of a total of 46 studies that were included in this metanalysis only a few were focused on AEs. A closer analysis of the studies with more focus on AEs disclosed the following results. Smaller studies only reported infusion-related AEs [18, 19]. With respect to larger studies, Kim et al. evaluated a group of 30 NMOSD (6 treatment naive) cases during 2 years of rituximab therapy and reported transient non-serious infusion-related reactions in 40% during the first infusion, mostly hypotension and flu-like symptoms (febrile sense, headache, rash) [20]. Also, they reported at least one non-serious infection in 40% of cases, including nasopharyngitis, upper and lower respiratory tract infection, and urinary tract infection [20]. A total of 27 of these patients were reported as a retrospective case series followed for 5 years to assess long-term efficacy of safety of rituximab [21]. No serious AEs were observed and the most commonly reported AEs were infections of respiratory tract, urinary tract, and a single case of Herpes zoster infection [21]. Bedi et al. found non-serious AEs in 30% of a group of 23 NMOSD patients (8 treatment-naive cases) [22]. Annovazzi et al. retrospectively studied 73 NMOSD cases (16 treatment-naive cases) from 13 MS centers in Italy and reported AEs in 19 cases (26%). Infections were the most frequent adverse events seen in 12 (16.4%) cases (6 urinary tract and 4 respiratory infections). Also, seven patients experienced infusion reactions, which led to drug interruption in two of them. One patient reported breast cancer and two died during the follow-up period; however, none as a result of treatment complications [15]. On contrary, a study on 21 NMOSD cases which received at least one course of rituximab therapy reported serious infections in five patients (24%) that lead to medication discontinuation in a single case with recurrent pneumonia and persistent leukopenia. All these patients had leukopenia and/or hypogammaglobulinemia and mostly presented with severe disability (median EDSS of 7.5). Notably, they were leukopenic before entering the study, and had a history of receiving immunosuppressive drugs [23]. In 11 cases (52%), the authors reported persistent IgG hypogammaglobulinemia after the first rituximab course. Moreover, they observed three non-infectious complications: one case of severe arterial hypotension followed by atrial fibrillation, one case of breast cancer (who was previously treated with cyclophosphamide), and one case with worsening of pre-existing monoclonal IgG gammopathy and persistent leukopenia, leading to discontinuation of therapy [23].
While most of these studies focused on rituximab efficacy and did not utilize a systematic approach to investigate safety, their findings are comparable to our results regarding the favorable tolerability of rituximab. The observed discrepancies could be justified with respect to patients’ demographic as well as medical history and previous immunomodulatory therapies. As perceived from Table 1, our sample population was relatively young and not severely disabled. This is an important determinant in treatment safety studies. Younger age and less disability are key factors that prevent a minor post-treatment insult from evolving into a full-blown infection or major complication [24]. In terms of age, the most similar study to ours was recently conducted by Memon et al. on 21 NMOSD with the mean age of 35 years and mild severity of disability [25]. Like our findings, they reported well tolerability of repeated rituximab infusions over time without serious infusion reactions, as well as UTI and URI as the most frequent complications [25]. Unlike our findings, 13% of their cases (4 out of 21 patients) required IV antibiotics or hospitalization for serious infections (pneumonia, UTI, sinusitis) [25]. Patients receiving rituximab are more prone to infections, especially of urinary and respiratory tract origin. These mucosal surfaces mainly rely on B-cell-produced IgA antibody molecules for their defense against pathogens [26].
Our study population included 30 treatment-naive cases (68%), considerably more than other studies. History of immunosuppressants could increase vulnerability to infections and other AEs due to long-term suppression of the immune system. The high rate of leukopenia in Radaelli et al. [23] study is not compatible with other reports as well as our findings and is probably due to the history of leukopenia in most of their subjects. Long-term rituximab therapy may increase the risk of hypogammaglobulinemia [23, 27]. As a limitation, we did not evaluate serum immunoglobulin levels in the current study.
None of the previous studies on NMOSD patients have reported any case of progressive multifocal leukoencephalopathy [17] as has been reported previously in rheumatoid arthritis [28], lymphoma [29], and lupus [30]. Regarding the other SAEs, we had one account of death, in a case with a complicated medical history, and severe hypersensitivity reaction in another case. Overall, deaths are reported in 1.6% of cases receiving rituximab [17]. Other reported SAEs include persistent leukopenia (4.6%) and reversible posterior encephalopathy (0.5%) [17] as well as those mentioned earlier. Malignancies have been rarely reported as a possible SAE of rituximab in very small number of studies as addressed earlier.
In the current study, we observed no difference regarding the reported AEs between seropositive and seronegative cases. This issue has not been investigated previously and serostatus does not seem to be a determinant for AEs. Moreover, no correlation was found between treatment duration and overall number of AEs. Similarly, Memon et al. claimed that rituximab adverse events are not related to the dosage, duration of treatment, and the number of treatment cycles [25]. Based on previously published data from large studies on other diseases (such as rheumatoid arthritis), there is no known correlation between the duration of treatment and AEs [31].
Regarding rituximab efficacy, we found a favorable outcome in our study group in response to rituximab as has been reported previously [17, 21, 32, 33]. Both EDSS and ARR of our patients significantly decreased following therapy. Notably, we found no difference regarding the efficacy between seropositive and seronegative patients as summarized by Damato et al. [17].
To conclude, the main side effects of rituximab therapy include infusion reactions, and opportunistic and non-opportunistic infections. Injection reactions are very common mostly controlled by antihistamines, IV steroids, or slow up-titration of rituximab. Our results showed that treatment with rituximab is well tolerated and safe in most cases; complications that concomitantly arise are self-limited. Rituximab favorably reduces disability and relapses, which renders rituximab as a safe and efficacious treatment option for NMOSD patients.
References
Hinson S, Pittock SJ, Lucchinetti CF, Roemer S, Fryer J, Kryzer T, Lennon VA (2007) Pathogenic potential of IgG binding to water channel extracellular domain in neuromyelitis optica. Neurology 69:2221–2231
Kim S-H, Mealy MA, Levy M, Schmidt F, Ruprecht K, Paul F, Ringelstein M, Aktas O, Hartung H-P, Asgari N (2018) Racial differences in neuromyelitis optica spectrum disorder. Neurology. https://doi.org/10.1212/WNL.0000000000006574
Melamed E, Levy M, Waters PJ, Sato DK, Bennett JL, John GR, Hooper DC, Saiz A, Bar-Or A, Kim HJ (2015) Update on biomarkers in neuromyelitis optica. Neurol Neuroimmunol Neuroinflamm 2:e134
Sand IK (2016) Neuromyelitis optica spectrum disorders. Continuum 22:864–896
Lucchinetti CF, Mandler RN, McGavern D, Bruck W, Gleich G, Ransohoff RM, Trebst C, Weinshenker B, Wingerchuk D, Parisi JE (2002) A role for humoral mechanisms in the pathogenesis of Devic’s neuromyelitis optica. Brain 125:1450–1461
Collongues N, de Seze J (2016) An update on the evidence for the efficacy and safety of rituximab in the management of neuromyelitis optica. Ther Adv Neurol Disord 9:180–188
Hauser SL, Bar-Or A, Comi G, Giovannoni G, Hartung HP, Hemmer B, Lublin F, Montalban X, Rammohan KW, Selmaj K, Traboulsee A, Wolinsky JS, Arnold DL, Klingelschmitt G, Masterman D, Fontoura P, Belachew S, Chin P, Mairon N, Garren H, Kappos L, Opera I, Investigators OIC (2017) Ocrelizumab versus interferon beta-1a in relapsing multiple sclerosis. N Engl J Med 376:221–234
Vale AM, Schroeder HW Jr (2010) Clinical consequences of defects in B-cell development. J Allergy Clin Immunol 125:778–787
Edwards JC, Szczepański L, Szechiński J, Filipowicz-Sosnowska A, Emery P, Close DR, Stevens RM, Shaw T (2004) Efficacy of B-cell—targeted therapy with rituximab in patients with rheumatoid arthritis. N Engl J Med 350:2572–2581
Wang Q, Racine JJ, Ratiu JJ, Wang S, Ettinger R, Wasserfall C, Atkinson MA, Serreze DV (2017) Transient BAFF blockade inhibits type 1 diabetes development in nonobese diabetic mice by enriching immunoregulatory B lymphocytes sensitive to deletion by anti-CD20 cotherapy. J Immunol 199:3757–3770
Etemadifar M, Salari M, Mirmosayyeb O, Serati M, Nikkhah R, Askari M, Fayyazi E (2017) Efficacy and safety of rituximab in neuromyelitis optica: review of evidence. J Res Med Sci 22:18
Maloney DG, Grillo-López AJ, White CA, Bodkin D, Schilder RJ, Neidhart JA, Janakiraman N, Foon KA, Liles T-M, Dallaire BK (1997) IDEC-C2B8 (rituximab) anti-CD20 monoclonal antibody therapy in patients with relapsed low-grade non-Hodgkin’s lymphoma. Blood 90:2188–2195
Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, de Seze J, Fujihara K, Greenberg B, Jacob A, Jarius S, Lana-Peixoto M, Levy M, Simon JH, Tenembaum S, Traboulsee AL, Waters P, Wellik KE, Weinshenker BG, International Panel for NMOD (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85:177–189
Waters P, Jarius S, Littleton E, Leite MI, Jacob S, Gray B, Geraldes R, Vale T, Jacob A, Palace J, Maxwell S (2008) Aquaporin-4 antibodies in neuromyelitis optica and longitudinally extensive transverse myelitis. Arch Neurol 65(7):913–919
Annovazzi P, Capobianco M, Moiola L, Patti F, Frau J, Uccelli A, Centonze D, Perini P, Tortorella C, Prosperini L, Lus G, Fuiani A, Falcini M, Martinelli V, Comi G, Ghezzi A (2016) Rituximab in the treatment of neuromyelitis optica: a multicentre Italian observational study. J Neurol 263:1727–1735
Pellkofer HL, Krumbholz M, Berthele A, Hemmer B, Gerdes LA, Havla J, Bittner R, Canis M, Meinl E, Hohlfeld R, Kuempfel T (2011) Long-term follow-up of patients with neuromyelitis optica after repeated therapy with rituximab. Neurology 76:1310–1315
Damato V, Evoli A, Iorio R (2016) Efficacy and safety of rituximab therapy in neuromyelitis optica spectrum disorders: a systematic review and meta-analysis. JAMA Neurol 73:1342–1348
Fernandez-Megia MJ, Casanova-Estruch B, Perez-Miralles F, Ruiz-Ramos J, Alcala-Vicente C, Poveda-Andres JL (2015) Clinical evaluation of rituximab treatment for neuromyelitis optica. Neurologia 30:461–464
Ip VH, Lau AY, Au LW, Fan FS, Chan AY, Mok VC, Wong KS (2013) Rituximab reduces attacks in Chinese patients with neuromyelitis optica spectrum disorders. J Neurol Sci 324:38–39
Kim SH, Kim W, Li XF, Jung IJ, Kim HJ (2011) Repeated treatment with rituximab based on the assessment of peripheral circulating memory B cells in patients with relapsing neuromyelitis optica over 2 years. Arch Neurol 68:1412–1420
Kim SH, Huh SY, Lee SJ, Joung A, Kim HJ (2013) A 5-year follow-up of rituximab treatment in patients with neuromyelitis optica spectrum disorder. JAMA Neurol 70:1110–1117
Bedi GS, Brown AD, Delgado SR, Usmani N, Lam BL, Sheremata WA (2011) Impact of rituximab on relapse rate and disability in neuromyelitis optica. Mult Scler 17:1225–1230
Radaelli M, Moiola L, Sangalli F, Esposito F, Barcella V, Ferre L, Rodegher M, Colombo B, Fazio R, Martinelli V, Comi G (2016) Neuromyelitis optica spectrum disorders: long-term safety and efficacy of rituximab in Caucasian patients. Mult Scler 22:511–519
Kosmidis ML, Dalakas MC (2010) Practical considerations on the use of rituximab in autoimmune neurological disorders. Ther Adv Neurol Disord 3:93–105
Memon AB, Javed A, Caon C, Srivastawa S, Bao F, Bernitsas E, Chorostecki J, Tselis A, Seraji-Bozorgzad N, Khan O (2018) Long-term safety of rituximab induced peripheral B-cell depletion in autoimmune neurological diseases. PLoS One 13:e0190425
Kantele A, Mottonen T, Ala-Kaila K, Arvilommi HS (2003) P Fimbria-specific B cell responses in patients with urinary tract infection. J Infect Dis 188:1885–1891
Marcinnò A, Marnetto F, Valentino P, Martire S, Balbo A, Drago A, Leto M, Capobianco M, Panzica G, Bertolotto A (2018) Rituximab-induced hypogammaglobulinemia in patients with neuromyelitis optica spectrum disorders. Neurol Neuroimmunol Neuroinflamm 5:e498
Clifford DB, Ances B, Costello C, Rosen-Schmidt S, Andersson M, Parks D, Perry A, Yerra R, Schmidt R, Alvarez E, Tyler KL (2011) Rituximab-associated progressive multifocal leukoencephalopathy in rheumatoid arthritis. Arch Neurol 68:1156–1164
Al-Tawfiq JA, Banda RW, Daabil RA, Dawamneh MF (2015) Progressive multifocal leukoencephalopathy (PML) in a patient with lymphoma treated with rituximab: a case report and literature review. J Infect Public Health 8:493–497
Molloy ES, Calabrese LH (2008) Progressive multifocal leukoencephalopathy in patients with rheumatic diseases: are patients with systemic lupus erythematosus at particular risk? Autoimmun Rev 8:144–146
van Vollenhoven RF, Emery P, Bingham CO 3rd, Keystone EC, Fleischmann RM, Furst DE, Tyson N, Collinson N, Lehane PB (2013) Long-term safety of rituximab in rheumatoid arthritis: 9.5-year follow-up of the global clinical trial programme with a focus on adverse events of interest in RA patients. Ann Rheum Dis 72:1496–1502
Mealy MA, Wingerchuk DM, Palace J, Greenberg BM, Levy M (2014) Comparison of relapse and treatment failure rates among patients with neuromyelitis optica: multicenter study of treatment efficacy. JAMA Neurol 71:324–330
Nikoo Z, Badihian S, Shaygannejad V, Asgari N, Ashtari F (2017) Comparison of the efficacy of azathioprine and rituximab in neuromyelitis optica spectrum disorder: a randomized clinical trial. J Neurol 264:2003–2009
Acknowledgements
The authors wish to thank the patients for their cooperation throughout the follow-up process.
Funding
No funding received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standard
The study was approved by research ethics committee of Isfahan University of Medical Sciences (Approval Code: IR.MUI.RSEARCH.REC.1397.171) and it was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Written informed consents were obtained from all patients upon enrollment.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shaygannejad, V., Fayyazi, E., Badihian, S. et al. Long-term tolerability, safety and efficacy of rituximab in neuromyelitis optica spectrum disorder: a prospective study. J Neurol 266, 642–650 (2019). https://doi.org/10.1007/s00415-019-09180-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09180-9