Abstract
Monitoring disease burden is an unmeet need in multiple sclerosis (MS). Identifying patients at high risk of disability progression will be useful for improving clinical-therapeutic decisions in clinical routine. To evaluate the role of visual field testing in non-optic neuritis eyes (non-ON eyes) as a biomarker of disability progression in MS. In 109 patients of the MS-VisualPath cohort, we evaluated the association between visual field abnormalities and global and cognitive disability markers and brain and retinal imaging markers of neuroaxonal injury using linear regression models adjusted for sex, age, disease duration and use of disease-modifying therapies. We evaluated the risk of disability progression associated to have baseline impaired visual field after 3 years of follow-up. Sixty-two percent of patients showed visual field defects in non-ON eyes. Visual field mean deviation was statistically associated with global disability; brain (normalized brain parenchymal, gray matter volume and lesion load) and retinal (peripapillary retinal nerve fiber layer thickness and macular ganglion cell complex thickness) markers of neuroaxonal damage. Patients with impaired visual field had statistically significative greater disability, lower normalized brain parenchymal volume and higher lesion volume than patients with normal visual field testing. MS patients with baseline impaired VF tripled the risk of disability progression during follow-up [OR = 3.35; 95 % CI (1.10–10.19); p = 0.033]. The association of visual field impairment with greater disability and neuroaxonal injury and higher risk of disability progression suggest that VF could be used to monitor MS disease burden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The afferent visual pathway has been proposed as a structural–functional paradigm for understanding brain damage in multiple sclerosis (MS) [1]. The visual pathway is frequently affected in patients with MS [2, 3] and visual dysfunction is highly relevant from the patients´ perspective [4]. Low-contrast visual dysfunction correlates with health-related quality of life [5] and global disability in MS [6]. Additionally, we found that color visual dysfunction in eyes without prior history of optic neuritis (non-ON eyes) was associated with greater disability progression and gray mater atrophy after 1 year of follow-up [7].
The field of vision is the portion of space in which objects are visible at the same moment during steady fixation of gaze in one direction. Standard automated perimetry such as the Humphrey visual field has been used to identify visual field (VF) defects in MS patients [8]. VF defects due to Optic Neuritis (ON) have been well described in MS patients [9, 10]. However, VF abnormalities have also been described in non-ON eyes [11]. VF defects in non-ON eyes may represent diffuse damage in the afferent visual pathway or local lesions in optic radiations or visual cortex.
Our goal was to investigate VF abnormalities in non-ON eyes in a cohort of MS patients, specifically addressing the relationship between VF impairment and other clinical and imaging parameters of neuroaxonal injury to evaluate its role as biomarker of central nervous system damage in MS in a longitudinal cohort study with three years of follow-up.
Materials and methods
Study design
The MS-VisualPath cohort is an ongoing prospective cohort study of patients with MS conducted at the Hospital Clinic of Barcelona—IDIBAPS (Spain). The design and methods of the MS-VisualPath cohort have been described in detail elsewhere [12]. Briefly, we recruited MS patients according to McDonalds Criteria [13, 14] without any psychiatric, neurological or ocular disorders that may interfere the aims of the study. The first consecutive prospective 115 patients of the cohort were included in this analysis. At baseline and yearly thereafter, patients underwent a complete examination including neurological evaluation, visual function test, optical coherence tomography and magnetic resonance imaging. Hospital Clinic of Barcelona Institutional Review Board approvals were obtained and all participants provided written informed consent.
Clinical evaluation
We collected demographic and MS-related variables (type of onset, diagnosis date, disease type, disease duration since first symptom onset, history of previous ON, disease-modifying therapies and clinical disability). The presence of prior ON was assessed in the electronic medical records as previously described [15] considering classical clinical presentation semiology and standard examinations previously described [16]. Subclinical episodes of ON were also checked by identifying an abnormal (a mean plus one standard deviation of the interocular asymmetry of registered ON clinical cases) asymmetry in the peripapillary retinal nerve fiber layer thickness measured by optical coherence tomography as previously described [3].
We assessed global neurological disability using the expanded disability status scale (EDSS) and multiple sclerosis functional composite (MSFC) at baseline and yearly thereafter. Disability progression was defined as showing at least one-point increase sustained for ≥3 months in the EDSS score (or at least half-point for if baseline EDSS ≥5.5) as has been used in recent MS clinical trials [17]. MSFC progression was defined as worsening on at least 1 MSFC component score by 20 % from baseline (MSFC progression-20), sustained for ≥3 months [18]. Cognitive functionality was evaluated at baseline with the brief repeatable battery-neuropsychology test including separate scores for verbal memory, visual memory, executive function and verbal fluency functions.
Visual field analysis
Best-corrected visual fields were evaluated with Humphrey field analyzer 750 (Carl Zeiss Meditec. Inc) using Swedish Interactive Threshold Algorithm—standard central 24–2 protocol, white stimulus Goldman size III (0.43°) with a background luminance of 31.5 Apostlibs [12]. All patients underwent an ophthalmological evaluation including wide-field fundus imaging, slit lamp examination and eye pressure measurement. Visual field testing was performed at baseline and after 1 year of follow-up.
We defined the reliability criteria following the Humphrey Instruments. Inc (San Leandro, CA) recommendations with <20 % fixation loss, <33 % of false positives and <33 % of false negative [19]. Any result not matching these criteria was repeated and excluded after two failed repetitions.
We evaluated visual field abnormalities quantitatively using visual field mean deviation. 54 individual points were tested in the case of the Humphrey 24-2 testing algorithm. Each individual location has a calculated deviation from the expected threshold value for a person of the same age and ethnicity. Visual field mean deviation is the average of the deviations across all test locations. We also evaluated visual field defects qualitatively using a modified version of the classification described in the Optic Neuritis Treatment Trial [9] and the Ocular Hypertension Treatment Study [20]. This classification included both quantitative and qualitative parameters to establish the differences between normal and impaired VF as well as the type of defect, including diffuse, focal and mix (focal + diffuse) abnormalities. We simplified the previously referred classifications by merging all types of local defects in a single category of focal defects for simplicity and because our main goal was to evaluate the role of a pathological (any type) VF as a marker of neuroaxonal damage and risk of disability progression in MS:
-
1.
Normal VF
-
(a)
The Glaucoma hemifield test VF index is normal and
-
(b)
Mean deviation (MD) and pattern standard deviation (PSD) does not show abnormality (p < 5 %) and
-
(c)
There are no abnormality criteria considering abnormal clustered points
-
(a)
-
2.
Abnormal VF
-
(a)
Glaucoma hemifield test index is abnormal and/or
-
(b)
MD and/or PSD show abnormality with p < 5 % and/or
-
(c)
A single point is worse than the 0.5 % probability level on the total and/or pattern deviation plot; and/or
-
(d)
Two clustered points are beyond the reference range (p < 5 %). and at least 1 point worse than the p < 1 % on the total and/or pattern deviation plot (a cluster is defined as 2 or more horizontally or vertically, not diagonally, contiguous abnormal points with p < 5 %); and/or
-
(e)
Three or more clustered points worse than p < 5 % on the total and/or pattern deviation plot and the pattern of loss is consistent with ocular abnormalities.
-
(a)
-
3.
Type of defects
-
(a)
Diffuse (also called widespread)
-
(i)
The Glaucoma hemifield test may show a general reduction of sensitivity or the MD must show a p value of less than 5 % and
-
(ii)
The corrected PSD must not show a p value of less than 5 % and
-
(iii)
Most abnormal points on the total deviation plot are not abnormal on the pattern deviation plot
-
(i)
-
(b)
Non-diffuse (focal)
-
(i)
The glaucoma hemifield test may show abnormality (different to general reduction of sensitivity) or the MD shows abnormality with p < 5 % and
-
(ii)
PSD shows a p value of less than <5 % or
-
(iii)
Most abnormal points on the total deviation plot are abnormal on the pattern deviation plot
-
(i)
-
(c)
Mix
-
(i)
VF result overlapping criteria mentioned in (a) and (b)
-
(ii)
Total loss: severe widespread VF loss (MD ≤ −20.00 dB)
-
(i)
-
(a)
We used only the visual field data of the non-ON eye in patients with previous history of unilateral ON. In patients without two non-ON eyes, we estimated visual field mean deviation as the mean of MD values of both non-ON eyes and considered a patient as having VF impairment if she/he had abnormal VF in either of the two non-ON eyes.
Imaging assessment
A trained optometrist performed a spectral domain optical coherence tomography (Spectralis®; Heidelberg Engineering) acquisition for each eye as previously described [12]. We used the 6.0c version of the Spectralis® segmentation algorithm version to quantify macular ganglion cell complex thickness as the sum of macular retinal nerve fiber layer, ganglion cell layer and inner plexiform layer. Peripapillary retinal nerve fiber layer and macular ganglion cell complex thicknesses were estimated as the mean value of both non-ON eyes except for patients with an ON eye for whom only the fellow non-ON eye’s value was considered.
Magnetic resonance imaging brain images were acquired using a Siemens Trim Trio® 3 T with a 32-channel phased array coil. The complete protocol has been described in detail [12]. Here, we used 3D structural T1-MPRAGE and FLAIR images to perform volumetric analyses using the same approach described to evaluate color vision abnormalities in MS [7]. First, T1-lesion masks were manually created from T1-MPRAGE using ITK-SNAP software [21]. Then, normalized brain parenchymal volume and normalized gray matter volume were evaluated with SIENAX (FMRIB, Oxford, UK) once the T1 lesion mask had been used to avoid pixel misclassification [22]. We calculated lesion load in the T1-MPRAGEs by counting the number of lesion voxels within the brain.
Statistical analysis
First, we performed descriptive statistics to characterize the sample using absolute numbers and proportions for qualitative variables and means and standard deviations for quantitative variables. Second, we performed bivariate analyses using the Fisher test for qualitative variables and independent 2-sample t tests for quantitative variables to compare demographic and MS-related variables in patients with and without VF impairment. Then, we ran multivariate linear regression models adjusted for sex, age, disease duration and the use of MS disease-modifying therapies to evaluate the association between visual field mean deviation in non-ON eyes at baseline and clinical, brain and retinal parameters of neuroaxonal damage. We also estimated the multivariable-adjusted means of these parameters between patients with and without VF abnormalities using general linear models, adjusting for the same covariates. Finally, we performed logistic regression analyses to evaluate the role of VF abnormalities in non-ON eyes at baseline as predictor of disability progression in MS adjusted for sex, age, disease duration, the use of disease-modifying therapies and also baseline disability. Two-tailed p values <0.05 were considered statistically significant. All analyses were performed with the Statistical Package IBM-SPSS software version 20.0 (SPSS Inc. Chicago. IL. USA).
Results
Visual field impairment in non-ON eyes in MS patients at baseline
First, we analyzed the VF impairment in non-ON eyes in MS patients. Out of the 115 MS patients, 65 had no prior history of ON in either eye while 44 patients had history of unilateral ON (and 6 patients had bilateral ON and for this reason were excluded from the analysis). Thus, 174 non-ON eyes were available for the analyses. The mean of visual field mean deviation in non-ON eyes was −2.75 (SD 2.04). We found that 75 non-ON eyes (43.1 %) had normal patterns in the perimetry; 41 non-eyes (23.5 %) displayed focal defects; 38 non-ON eyes (21.9 %) showed diffuse abnormalities; and 20 non-ON eyes (11.5 %) had a mix patterns in the perimetry.
Demographic and MS-related variables among patients
Next, we compared the demographics and MS-related features in patients with and without VF impairment in non-ON eyes. Out of the 109 MS patients analyzed, 68 (62.4 %) had an abnormal VF pattern, while 41 (37.6 %) had a normal VF pattern. Patients with impaired VF had a trend to longer disease duration compared to those with normal VF. We did not find any significant difference in other variables (Table 1).
Visual field impairment is associated with higher disability and CNS atrophy at baseline
Visual field mean deviation was statistically associated with global disability (MSFC, p = 0.001); brain markers of neuroaxonal damage (normalized brain parenchymal volume, p = 0.003; normalized gray matter volume, p = 0.05; lesion load; p < 0.001) and retinal parameters of neuroaxonal injury (peripapillary retinal nerve fiber layer thickness; p = 0.035; macular ganglion cell complex thickness, p = 0.026) (Table 2). MS patients with impaired VF suffered greater global disability and cognitive decline than those with normal VF, as reflected by the significantly higher EDSS and lower cognitive performance (Table 3). These patients also showed significantly lower normalized brain parenchymal volume and higher lesion volume as well as a trend towards lower normalized gray matter volume and macular ganglion cell complex thickness (Table 3).
Visual field impairment at baseline is associated with a higher risk of disability progression after 3 years of follow-up
Visual field mean deviation at baseline was associated with disability progression using EDSS and/or MSFC (Table 4). Our model predicts that a MS patient with a visual field mean deviation in non-ON eye 1 dB higher has 47 % [(1 − 0.53) × 100 = 47] lower risk of disability progression as measured by EDSS or/and MSFC compared with a MS patient with a 1 dB lower visual field mean deviation. Therefore, a patient with a visual field mean deviation in non-ON eye 1 dB lower has a 87 % [OR = e−(b.coef) = e−(−0.627) = 1.87] greater risk of disability progression. MS patients with impaired VF at baseline tripled the risk of disability progression after 3 years of follow-up (Table 4).
Longitudinal changes in the VF after 1-year follow-up
Finally, we performed longitudinal analyses of the VF changes after 1 year of follow-up, but not subsequently during the follow-up because VF testing was only performed at baseline and after 1-year follow-up. 97 out of 109 had longitudinal information of the VF at 1-year follow-up. The VF changes were analyzed from quantitative and qualitative points of view. For the quantitative analysis, we compared the data of visual field mean deviation between baseline and the first-year follow-up visit. The visual field mean deviation was significantly lower (p = 0.023), suggesting more severe impairment after 1 year (−3.11 ± 2.66) than at baseline (−2.77 ± 2.09). Moreover, we found that 11 patients (32 %) with a VF classified as normal at baseline were classified as pathological after 1 year of follow-up. On the other hand, seven patients (10 %) that were classified as abnormal VF initially, changed to normal VF after 1-year follow-up. We did not find any statistical differences in disability progression (EDSS, MSFC) and brain and retinal imaging markers of neuroaxonal loss between those who developed incident impaired VF (11 patients) and those who remained with normal VF outcomes (23 patients) (data not shown).
Discussion
The most important results coming from this study are that MS patients with visual field abnormalities in non-ON eyes showed greater disability and neuroaxonal damage and threefold increased risk of disability progression after 3 years of follow-up. These differences were adjusted by possible confounding factors such as sex, age, disease duration and the use of disease-modifying treatments and baseline disability for longitudinal analyses.
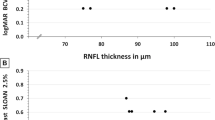
Brain volume loss measured by magnetic resonance imaging is likely the most widely accepted measure of neuroaxonal damage in MS [23]. In our cohort, visual field mean deviation was positively associated with normalized brain parenchymal volume and patients with visual field abnormalities displayed lower brain parenchymal volume compared with those with normal visual field testing. Retinal atrophy has recently been associated with brain atrophy [24]. In our study, both peripapillary retinal nerve fiber layer and macular ganglion cell complex thicknesses were positively associated with visual field mean deviation. However, even both retinal layer thicknesses were lower for those with pathological VF compared with patients with normal VF testing, differences did not reach statistical significance. So far, it has been reported moderate to strong associations between these retinal imaging markers and both low-contrast visual acuity [25] and color vision scores [26] in non-ON eyes of MS patients. Regarding visual field testing, associations between optical coherence tomography parameters and VF were identified for ON-eyes [27], but these associations were absent for non-ON eyes in some studies using standard white-on-white perimetry [8, 28]. One explanation may be that visual field abnormalities might appear due to damage along the entire visual pathway [11] while retinal ganglion cell damage has been identified as the main contributor leading to low-contrast visual acuity abnormalities [29] and dyschromatopsia [30].
The associations between visual field mean deviation and brain parenchymal volume and retinal thickness suggest that neuroaxonal damage is a relevant histopathological mechanism responsible of visual field impairment. However, diffuse demyelination should be also considered as an important factor leading to visual pathway dysfunction. Diffuse demyelination during central nervous system inflammation in MS contribute to the dysfunction and maldistribution of ion channels leading to excitotoxicity, mitochondrial dysfunction and energy failure. All of these mechanisms culminate in neuroaxonal damage [31]. The role of demyelination, as a common antecedent to axonal injury, in the VF testing dysfunction has been evaluated using multifocal visual evoked potentials (mfVEPs). The latency of mfVEPs is a relatively novel approach for assessing the extent of demyelination in MS. Laron M and colleagues compared the role of mfVEPs, VF testing and optical coherence tomography for assessing visual pathway integrity in a cohort of MS patients. These authors found that 38 % of non-ON eyes were found to be abnormal based on VF testing while 25 and 8 % of non-ON eyes were abnormal based on mfVEPs (latency) and optical coherence tomography (RNFL), respectively. The authors evaluated retinal thickness using a time-domain optical coherence tomography that may have limited their results. Nevertheless, these results suggested that VF abnormalities could be found even in the absence of significant neuroaxonal damage [32].
We found that patients with visual field abnormities had greater disability than those with normal visual field testing. It has been reported good correlations between disability and other visual function tests such as low-contrast vision acuity [33, 34] or color vision [7]. These tests are technically easier and shorter to be administered in the clinical care. However, there is not enough evidence that they can predict risk of disability progression in the medium- or large follow-up. The novelty and the strength of this study are that we found that visual field impairment at baseline was associated with an increased risk of disability progression after 3 years of follow-up in our cohort. These results suggest that VF impairment captures the damage in the central nervous system of MS patients, expanding upon the widely described role of the VF testing as a measurement of visual outcomes due to the acute inflammatory events affecting the optic nerve such as ON.
We also found significant changes in the VF between baseline and the first year of follow-up when considering the mean deviation values. However, when we compared patients who developed impaired VF after the first follow-up with patients who still displayed normal VF, we did not find statistical differences in any of the clinical or imaging markers of MS burden. However, the small sample size of this comparison (n: 44) and the short follow-up may partially explain these results. There were seven patients classified as normal VF in the first-year follow-up with abnormal VF at baseline. None of these seven patients had abnormal results during the ophthalmological examination during the first follow-up visit. These findings could be explained by several different reasons. First, it could be related to the fluctuations in the clinical state of the disease that could affect the result of the perimetry as a subjective test (e.g., pseudoexacerbations). Second, the well-known learning effect when performing standard automated perimetry could explain why certain cases originally classified as abnormal transitioned to normal at the first-year follow-up [35]. Finally, in our study, 3 out of these 7 cases obtained reliability indices close to the limits; this fact could have caused certain cases to be wrongly classified as abnormal at baseline.
The identification of markers of neuroaxonal damage is critical for developing neuro-protective drugs. Our study shows that the VF test is a useful tool to evaluate central nervous system damage in MS independently of the prior history of ON and to predict risk of disability progression in MS.
References
Martínez-Lapiscina E, Sanchez-Dalmau B, Fraga-Pumar E et al (2014) The visual pathway as a model to understand brain damage in multiple sclerosis. Multiple Scler 20:1678–1685
Castro SMC, Damasceno A, Damasceno BP et al (2013) Visual pathway abnormalities were found in most multiple sclerosis patients despite history of previous optic neuritis. Arq Neuropsiquiatr 71:437–441
Gabilondo I, Martínez-Lapiscina EH, Martínez-Heras E et al (2014) Trans-synaptic axonal degeneration in the visual pathway in multiple sclerosis. Ann Neurol 75:98–107
Heesen C, Böhm J, Reich C et al (2008) Patient perception of bodily functions in multiple sclerosis: gait and visual function are the most valuable. Multiple Scler 14:988–991
Mowry EM, Loguidice MJ, Daniels AB et al (2009) Vision related quality of life in multiple sclerosis: correlation with new measures of low and high contrast letter acuity. J Neurol Neurosurg Psychiatry 80:767–772
Balcer LJ, Baier ML, Cohen JA et al (2003) Contrast letter acuity as a visual component for the multiple sclerosis functional composite. Neurology 61:1367–1373
Martínez-Lapiscina EH, Ortiz-Pérez S, Fraga-Pumar E et al (2014) Colour vision impairment is associated with disease severity in multiple sclerosis. Multiple Scler 20:1207–1216
Cheng H, Laron M, Schiffman JS et al (2007) The relationship between visual field and retinal nerve fiber layer measurements in patients with multiple sclerosis. Invest Ophthalmol Vis Sci 48:5798–5805
Keltner JL, Johnson CA, Cello KE, Dontchev M (2014) Visual field profile of optic neuritis (a final follow-up report from the optic neuritis treatment trial from baseline through 15 years). Arch Ophthalmol 128:330–337
Nevalainen J, Krapp E, Paetzold J et al (2008) Visual field defects in acute optic neuritis–distribution of different types of defect pattern, assessed with threshold-related supraliminal perimetry, ensuring high spatial resolution. Graefes Arch Clin Exp Ophthalmol 246:599–607
Chorazy M, Drozdowski W, Sherkawey N, Mariak Z (2007) Asymptomatic visual field disturbances in multiple sclerosis patients without a history of optic neuritis. Neurol Neurochir Pol 41:223–228
Martínez-Lapiscina EH, Fraga-Pumar E, Gabilondo I et al (2014) The multiple sclerosis visual pathway cohort: understanding neurodegeneration in MS. BMC Res Notes. doi:10.1186/1756-0500-7-910
Polman CH, Reingold SC, Edan G et al (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol 58:840–846
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Martínez-Lapiscina EH, Fraga-Pumar E, Pastor X et al (2014) Is the incidence of optic neuritis rising? Evidence from an epidemiological study in Barcelona (Spain), 2008–2012. J Neurol 261:759–767
Petzold A, Wattjes MP, Costello F et al (2014) The investigation of acute optic neuritis: a review and proposed protocol. Nat Rev Neurol 10:447–458
Cohen JA, Barkhof F, Comi G et al (2010) Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med 362:402–415
Rudick RA, Polman CH, Cohen JA et al (2009) Assessing disability progression with the multiple sclerosis functional composite. Multiple Scler 15:984–997
Birt CM, Shin DH, Samudrala V et al (1997) Analysis of reliability indices from humphrey visual field tests in an urban glaucoma population. Ophthalmology 104:1126–1130
Keltner JL, Johnson CA, Cello KE et al (2003) Classification of visual field abnormalities in the ocular hypertension treatment study. Arch Ophthalmol 121:643–650
Yushkevich PA, Piven J, Hazlett HC et al (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31:1116–1128
Sdika M, Pelletier D (2009) Nonrigid registration of multiple sclerosis brain images using lesion inpainting for morphometry or lesion mapping. Hum Brain Mapp 30:1060–1067
De Stefano N, Airas L, Grigoriadis N et al (2014) Clinical relevance of brain volume measures in multiple sclerosis. CNS Drugs 28:147–156
Saidha S, Al-Louzi O, Ratchford JN et al (2015) Optical coherence tomography reflects brain atrophy in multiple sclerosis: a four-year study. Ann Neurol 78:801–813
Sriram P, Wang C, Yiannikas C et al (2014) Relationship between optical coherence tomography and electrophysiology of the visual pathway in non-optic neuritis eyes of multiple sclerosis patients. PLoS One 9:e102546. doi:10.1371/journal.pone.0102546
Villoslada P, Cuneo A, Gelfand J et al (2012) Color vision is strongly associated with retinal thinning in multiple sclerosis. Multiple Scler 18:991–999
Trip SA, Schlottmann PG, Jones SJ et al (2005) Retinal nerve fiber layer axonal loss and visual dysfunction in optic neuritis. Ann Neurol 58:383–391
Kitsos G, Detorakis ET, Papakonstantinou S et al (2011) Perimetric and peri-papillary nerve fibre layer thickness findings in multiple sclerosis. Eur J Neurol 18:719–725
Walter SD, Ishikawa H, Galetta KM et al (2012) Ganglion cell loss in relation to visual disability in multiple sclerosis. Ophthalmology 119:1250–1257
Lampert EJ, Andorra M, Torres-Torres R et al (2015) Color vision impairment in multiple sclerosis points to retinal ganglion cell damage. J Neurol 262:2491–2497
Friese MA, Schattling B, Fugger L (2014) Mechanisms of neurodegeneration and axonal dysfunction in multiple sclerosis. Nat Rev Neurol 10:225–238
Laron M, Cheng H, Zhang B et al (2010) Comparison of multifocal visual evoked potential, standard automated perimetry and optical coherence tomography in assessing visual pathway in multiple sclerosis patients. Multiple Scler 16:412–426
Schinzel J, Zimmermann H, Paul F et al (2014) Relations of low contrast visual acuity, quality of life and multiple sclerosis functional composite: a cross-sectional analysis. BMC Neurol 14:31
Baier ML, Cutter GR, Rudick RA et al (2005) Low-contrast letter acuity testing captures visual dysfunction in patients with multiple sclerosis. Neurology 64:992–995
Castro DPE, Kawase J, Melo LAS (2008) Learning effect of standard automated perimetry in healthy individuals. Arq Bras Oftalmol 71:523–528
Acknowledgments
We are extremely grateful to the MS-VisualPath participants and fieldworkers without whose contribution, this study would not be possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data
Elena H. Martínez-Lapiscina had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
This study was supported by Instituto de Salud Carlos III, Spain: PS09/00259 and RD07/0060/01 to PV and RD12/0032/0002 to AS. EHML was supported by a fellowship from the Instituto de Salud Carlos III, Spain (Rio Hortega Program: CM13/00150). The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of interest
AS has received compensation for consulting services and speaking from Bayer-Schering, Merck-Serono, Biogen-Idec, Sanofi-Aventis, Teva Pharmaceutical Industries Ltd and Novartis. PV has received consultancy fees from Heidelberg Engineering regarding the clinical applications of optical coherence tomography. Elena H Martinez-Lapiscina has received for speaking honoraria from Biogen Idec and Genzyme and travel reimbursement from TEVA for The European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) and Sociedad Española de Neurología (SEN) and from Bayer Healthcare for American Academy of Neurology (AAN) over the last 3 years. All other authors have no conflicts of interest to declare.
Ethical standard
This means that the study has compliance with ethical standars which is a key requirement to obtain the approval by the mentioned committee.
Informed consent
It is stated in methods that Hospital Clinic of Barcelona Institutional Review Board approvals were obtained and all participants provided written informed consent.
Rights and permissions
About this article
Cite this article
Ortiz-Perez, S., Andorra, M., Sanchez-Dalmau, B. et al. Visual field impairment captures disease burden in multiple sclerosis. J Neurol 263, 695–702 (2016). https://doi.org/10.1007/s00415-016-8034-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8034-2