Abstract
Regular lifestyle behaviors (RLBs) of sleep, exercise, mealtime pattern and hydration status independently affect migraine occurrence. We aimed herein to evaluate the differences in migraine occurrence among participants who do and do not maintain the RLB triumvirate. Cases of chronic migraine (CM) and referents of episodic migraine (EM) ≥aged 15 years with charts regularly documenting RLB notes were continuously enrolled from a retrospective case–referent cohort study performed on electronic chart review from January 1, 2014 to January 1, 2015 at the Stanford Headache and Facial Pain Program. Association between RLB prevalence and migraine occurrence was studied. 175 CM and 175 EM patients were enrolled (mean age 44.4 years, 22 % males). Migraine was diagnosed according to the ICHD-3 beta criteria, and was confirmed by a Headache Specialist attending the Clinic. The CM cohort (22 %) exhibited less RLB than the EM cohort (69 %), with crude odds ratio of 0.13 (95 % confidence interval or CI 0.08–0.21). The adjusted odds ratio and adjusted relative risk between RLB+, Meds+ (those taking medication) and CM were 0.67 (95 % CI 0.32–1.40) and 0.74 (95 % CI 0.43–1.28), indicating no significant effect modification. Engaging in regular lifestyle behavior helps quell chronic migraine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lifestyle factors play an essential role in promoting wellness and managing disease [1]. The field of lifestyle medicine has become part of evidence-based daily practice in treating and managing disease. Maintenance of biological rhythms is important in maintaining health, i.e., ultradian (e.g., feeding cycles) [2], circadian (e.g., cycles of sleep, digestive secretions, bowel movements) [3], infradian (e.g., menstrual cycles) [3], and diurnal rhythms (circadian rhythms synchronized with day–night cycle) [4]. Lifestyle behaviors of sleep [5], exercise [6–8], mealtime pattern [9] and hydration status [10] are known to independently affect migraine occurrence. Individual-customized daily aerobic exercise, daily scheduled stress management and relaxation techniques, and mindfulness-based stress reduction prevent migraine [5], while inadequate sleep hygiene, non-restorative sleep, skipping meals, and dehydration can trigger migraine [11–14]. The ever-increasing demands of modern life can be challenging and stressful making the individual overlook cardinal self-care behaviors. Synchronized chronobiology and hormonal patterns facilitate self-awareness of well-being and adaptation to milieu of internal and external changes, ultimately coping with migraine triggers [12, 15, 16]. Non-pharmacologic treatments have been shown to be effective in controlling migraines [1, 17].
Given the significance of these individual lifestyle factors, it is important to study the relationship between the RLB triumvirate (regular lifestyle behavior of sleep, mealtime, and daily exercise) and migraine. Our review of the medical literature did not identify studies investigating the combined effects of these three domains of RLB. Previous studies have investigated one domain alone, i.e., either sleep [5, 18], exercise [6, 11], or mealtime [15]. The purpose of the present study is to address this by investigating the connection between the RLB triumvirate and migraine.
Materials and methods
Study question stem
We are examining the association between chronic migraine and regular lifestyle behavior (RLB) with consistency of daily aerobic exercise, scheduled sleep pattern, and regular mealtime. To address this, we designed a clinical study comparing the prevalence of RLB among a cohort of episodic migraine referents and chronic migraine cases. Based on the results obtained, we will deduce the impact of RLB on migraine frequency.
Study setting
The study setting was Stanford Headache and Facial Pain Clinic, at the Stanford Hospitals and Clinics in Stanford, California. The Clinic is a quaternary referral clinical center providing care for more than 3000 patients annually, and manages referrals from catchment areas in California and beyond. Most patients present after having been seen and investigated by various neurologists, primary care physicians and pain specialists (anesthesiology); thus, the clinic often addresses the challenges of misdiagnosis, underdiagnosis, undermanagement, and mismanagement. Through the clinic’s multidisciplinary program involving headache medicine, pain medicine, pain psychology, physical therapy, psychophysiological therapy, and integrative medicine, patients are provided a wide range of personalized management options.
Cases and referents
We conducted a prevalence case–referent study, sex-matched, examining RLB and frequency of headache days among 175 episodic (referents) and 175 chronic migraine (cases) patients. Enrollment was conducted from a cohort population identified using the Stanford Translational Research Integrated Database Environment (STRIDE) [19] Clinical Data Review Tool based on electronic medical records seen and followed at the Stanford Headache and Facial Pain Clinic. STRIDE [19] is a clinical informatics research and development project at Stanford University to create a standards-based informatics platform supporting clinical and translational research. Ethical clearance from the Stanford University IRB (Institutional Review Board) was sought and full approval was obtained (Protocol 30921).
Inclusion and exclusion criteria, data extraction
Clinical documents of any type containing the keywords ‘episodic migraine’ and ‘chronic migraine’ from January 1, 2014 until January 1, 2015 were screened for possible inclusion and exclusion. Inclusion criteria were age 15 years and older, and charts documenting notes on RLB for a minimum duration of 6 months. Exclusion criteria were age younger than 15 years, patients with primary insomnia, shift workers, and charts not documenting notes on RLB. RLB was phenotyped in the chart documentation, and this included clear account on the following three self-report domains: maintaining regular sleep hours with consistent sleep–wake time both in weekdays and weekends, maintaining regular daily mealtime and adequate hydration status, and maintaining daily aerobic exercise of any form for a minimum 20 min duration that raises heart rate. Regular mealtime consisted of keeping consistent meal hours; number of meals was personalized according to the preference of each patient since our study focused on the regularity of mealtimes rather than mealtime frequency. Adequate hydration status similarly consisted of keeping regular amounts of daily water intake; this was also personalized to patient preference. Those patients maintaining all three domains were designated as RLB+; those patients not maintaining all three domains were designated as RLB−.
Depression and anxiety disorders were tallied in both cohorts of episodic and chronic migraineurs to examine their potential confounding effect within the final analysis.
Sample size: matched case–referent power analysis
Sample size was powered to be adequate aposteriorally as post hoc results revealed both statistical and clinical significance. In this sex-matched case-referent study power analysis, assuming the probability of exposure among sampled participants to be 20 %, a sample of 175 cases and 175 referents were obtained based on the pool size of the clinic’s patient annual population size. This total sample size of 350 patients achieves 85 % power to detect a minimum relative risk ratio of 0.005 [20]. PASS v.13 software was utilized for power analysis and sample size computation.
Diagnosis of migraine was made according to the ICHD-3 beta version (International Classification of Headache Disorders) [21] criteria, and every diagnosis was confirmed by a Headache Specialist attending the Clinic. That our diagnosis and headache phenotyping were founded on highly accurate methods with negligible diagnostic errors boosted the statistical power of our sample size, i.e., reducing the false-negative rate. Methods and design of the study were in accordance with STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) [22] checklist.
Statistical analyses and computational notes
Both cohorts were stratified by age group to study their age distribution. Parametric distribution was tested among age and monthly migraine frequency for which Shapiro–Wilk [23] and D’Agostino–Pearson [23] omnibus normality tests were applied. The mean and SD were selected for inter-group comparison of parametric distribution, while the median and interquartile ratios were selected for non-parametric distribution. Means of parametric distributions were analyzed using unpaired t test with Welch’s correction (unequal variance t test) [24], while the Mann–Whitney test was employed to analyze medians of non-parametric distributions. The crude odds ratio (OR), its standard error and 95 % confidence interval were calculated employing standard techniques. The OR was generated by computing the prevalence rate of chronic migraine among those exposed to RLB out of those not exposed to RLB divided by rate of episodic migraine among those exposed to RLB to those not exposed to RLB. The crude relative risk (RR), its standard error and 95 % confidence interval were calculated using standard techniques. The RR was generated by computing the risk of chronic migraine among patients exposed to RLB divided to risk of chronic migraine among patients not exposed to RLB. Relative risk of <1 meant the risk of bad outcome (i.e., chronic migraine) was less likely to occur among the RLB+ cohort than among the RLB− cohort, indicating that the exposure to RLB was beneficial. Analysis of RR was included since crude prevalence of migraine among the general population is known to be marginally higher than 10 % [25]; OR is the preferred method for rare diseases with lower prevalence of under 10 % while RR is generally safer method for diseases with higher prevalence of above 10 %. Moreover, RR analysis enabled us to ascertain RLB exposure and determine the outcome of either chronic/episodic migraine—thereby enabling a retrospective cohort design.
To enhance decision-making for clinical practice and recommendations, absolute risk reduction (ARR) was computed by subtracting risk of chronic migraine among patients exposed to RLB from risk of chronic migraine among patients not exposed to RLB. Numbers needed to treat (NNT) was calculated by dividing 1 to the ARR value, i.e., as the inverse of the ARR. Relative risk reduction (RRR) was calculated by dividing the difference between the two relative risks to the relative risk among of chronic migraine among patients not exposed to RLB.
To study the potential for effect modification by medication use (abortive and/or preventive), our line of inquiry followed the question: What is the association between RLB exposure and chronic migraine given presence or absence of medication use? Adjusted odds ratio (AOR) and adjusted relative risk (AdRR) was then computed among patients stratified into those exposed to RLB (RLB+) given baseline medication use compared to no baseline medication use. Similarly, RLB+ cohort were stratified into those suffering or not suffering depression and/or anxiety and AdRR computed to address the following question: What is the association between RLB exposure and chronic migraine given presence or absence of depression and/or anxiety? Statistical software employed included Analyse-it v.3.80, GraphPad Prism v.5, NCSS v.9, and PASS v.13 [20]. Two-tailed p values were calculated and the level of statistical significance was set to p < 0.05.
Additionally, to analyze the potential for confounding effect by medication use, depression, and anxiety, the Cochran–Mantel–Haenszel (CMH) method was employed to generate a single, summary measure of association between RLB exposure and chronic migraine after adjusting for or taking into account potential confounding by medication use and depression and/or anxiety. The method was used with a dichotomous outcome of either chronic or episodic migraine, and an additional dichotomous risk factor of either presence or absence of RLB exposure. We stratified the data into two levels (i.e., medication use, depression and/or anxiety) of the confounding factors. In essence, we computed a series of two-by-two strata showing the association between the RLB exposure and outcome of chronic migraine at three levels of the confounding factors, and we then computed a weighted average of the relative risk ratios or odds ratios across the strata (i.e., across levels of the confounders).
Results
175 referents of episodic migraine with a combined total of 1016 mean monthly headache days and 175 cases of chronic migraineurs with a combined total of 3786 mean monthly headache days were continuously enrolled. There was no missing data with regards to variables of interest. Twenty-two percent of the patients were males in both cohorts. Age distribution was found to have parametric distribution among both episodic and chronic migraine cohorts (Fig. 1). Mean age was 41 years (26, 59) among the episodic migraine cohort, and 40 years (26, 55) among the chronic migraine cohort (p = 0.86, Student t test; Fig. 1). Monthly migraine frequency distribution was found to have non-parametric distribution among both episodic and chronic migraine cohorts (Fig. 2). By virtue of featuring a more robust method to outlier data, median and interquartile range (IQR) of the monthly migraine frequency distribution was computed to amalgamate the non-parametric nature of migraine frequency data. Median monthly migraine frequency was 5 (IQR 2, 10) among the episodic migraine patients, and 25 (IQR 20, 30; p < 0.001 Mann–Whitney test, Fig. 2).
Scatter plot for age distribution [mean and standard deviation (SD)] among the two cohorts of episodic and chronic migraine patients. Both age distribution cohorts passed normality tests of Shapiro–Wilk normality test and D’Agostino and Pearson omnibus normality test; hence means and parametric t tests were selected for further inter-cohort comparison. Mean age was 41 years (SD 26, 59) among the episodic migraine cohort, and 40 years (26, 55) among the chronic migraine cohort (p = 0.86; Student t test)
Scatter plot for mean monthly migraine frequency [median and interquartile range (IQR)] among the two cohorts of episodic and chronic migraine patients. Both monthly migraine frequency cohorts did not pass normality tests of Shapiro–Wilk normality test and D’Agostino and Pearson omnibus normality test; hence medians and non-parametric t tests were selected for further inter-cohort comparison. Median monthly migraine frequency was 5 (IQR 2, 10) among the episodic migraine patients, and 25 (IQR 20, 30; p < 0.001; Mann–Whitney test)
The CM cohort (22 %) exhibited less RLB than the EM cohort (69 %), with crude odds ratio of 0.13 (95 % CI 0.08–0.21; p < 0.001; Fig. 3). Similarly, the RLB+ cohort (patients with RLB) exhibited less CM (24.5 %) than the RLB− cohort (71.2 %) (patients without RLB), with RR of 0.34 (95 % CI 0.26–0.46; p < 0.0001). The absolute risk reduction (ARR) of chronic migraine among patients exposed to RLB deducted from risk of chronic migraine among patients not exposed to RLB was 46.7 %, while the relative risk reduction (RRR) was 65.6 %. The numbers needed to treat (NNT) was found to be 2.14.
Difference in prevalence of regular lifestyle behavior (RLB) among the chronic and episodic migraine cohorts. There was lower prevalence of patients having RLB (RLB+) among the chronic migraine cohort (22 %) (A). The prevalence of patients having RLB (RLB+) was higher among the episodic migraine cohort (69 %)
Stratifying the triumvirate RLB into its three components showed that while all three components were seen in lower frequency among the chronic migraine cohort, the trend was similar in both cohorts in that it followed a decreasing pattern from regular mealtime, regular sleep, to daily exercise. Regular mealtime was the behavior most commonly adopted by both cohorts, while daily exercise was the least (Fig. 4). When comparing the impact from the triumvirate RLB to the impact from any of its three components, regular sleep had identical impact to that of the triumvirate RLB (i.e. 50 % difference between the cohorts of episodic and chronic migraine) while the impacts from daily exercise (45 % difference) and regular mealtime (46 %) alone were marginally lower than the triumvirate RLB (50 % difference; Fig. 4). Average sleep duration was 6.4 h (range 5–8.3 h).
Dissecting the RLB triumvirate (B) among the chronic and episodic migraine cohorts. Stratifying the triumvirate RLB into its three components showed that while all three components were seen in lower frequency among the chronic migraine cohort, the trend was similar in both cohorts in that it followed a decreasing pattern from regular mealtime, regular sleep, to daily exercise. Regular mealtime was the behavior most commonly adopted by both cohorts, while daily exercise was the least. When comparing the impact from the triumvirate RLB to the impact from any of its three components, regular sleep had identical impact to that of the triumvirate RLB (i.e., 50 % difference between the cohorts of episodic and chronic migraine) while the impact from daily exercise (45 % difference) and regular mealtime (46 %) alone was marginally lower than the triumvirate RLB (50 % difference)
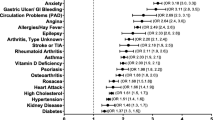
Effect modification from medication use assessed the potential effect modification of the third variable, i.e., medication use. Those patients having RLB (RLB+) were stratified into those taking medication (Meds+) and those not taking medication (Meds−) revealing adjusted odds ratio (AOR) of 0.67 (95 % CI 0.32–1.40; p = 0.29); this AOR value did not show significant implication. The Meds+ cohort exhibited comparable CM (21.6 %) to the Meds− cohort (29 %), with adjusted relative risk (AdRR) of 0.74 (95 % CI 0.43–1.28; p = 0.28); again indicating a non-significant implication, thus implying the absence of effect modification by medications. CMH for RR between lack of RLB exposure and chronic migraine controlled for medication use was 1.24; this supports the above result that chronic migraine is associated with lack of RLB exposure even when controlling for medication use. Stratifying RLB+ cohort into those suffering or not suffering depression and/or anxiety revealed AdRR of 0.72 (95 % CI 0.32–1.61; p = 0.43); indicating a non-significant implication, thus implying the absence of effect modification by the presence of depression and/or anxiety. Similarly, CMH for RR between lack of RLB exposure and chronic migraine controlled for depression and/or anxiety was 7.5. Medication use was heterogeneous, and thus, we chose not to stratify as it reflects a representation of the real-world practice of varying provider and patient preference and profiles. The migraine preventive medications that were taken include tricyclic antidepressants (e.g., nortriptyline), calcium channel blockers (e.g., verapamil), antiepileptics (e.g., topiramate), beta blockers (e.g., metoprolol), onabotulinumtoxinA, magnesium and riboflavin. Most medications were taken for a minimum of 3 months.
Among the cohort of chronic migraineurs who were following the RLB, they were progressively month after month converting into episodic migraineurs, while the episodic migraineurs who were not following the RLB were converting into chronic migraine, month after month (based on 1-year observation). This bidirectional relationship was also found to have a continuous relationship with the degree of RLB compliance, i.e., the more complete the RLB triumvirate compliance, the better outcomes for chronic to episodic migraine reversion. The less complete the RLB triumvirate compliance (e.g., only mealtime regularity) were, the less were the chances for chronic to episodic reversion.
Discussion
The age and migraine frequency distribution of our study patients were representative of episodic and chronic migraine patients in the general population aged 15 years and older. That patients without RLB were more likely to have chronic migraine as compared to the chances of having episodic migraine underscores the importance of maintaining regular behavior in controlling the occurrence of migraine headache. The OR as an effect size measuring the strength of association between RLB prevalence and chronic migraine revealed that RLB prevalence was significantly associated with lower odds of having chronic migraine. Similarly, the RR for the association between RLB prevalence and chronic migraine showed that the risk of having chronic migraine was significantly reduced for patients with RLB. Both the ARR of 47 % and RRR of 66 % distinctly indicated that higher RLB prevalence was protective from developing chronic migraine. These positive results were further strengthened by the fact that the benefit of RLB effectiveness was observed at least at every 2nd patient treated—as per the NNT of 2. Adjusting these results to the possible effect modifier of medication use and depression and/or anxiety did not reveal significant implications. Evidence suggestive of cause and effect with regard to RLB was found based on our progressive observation of the chronic and episodic migraineurs; episodic migraineurs not following RLB were progressively converting to become chronic migraineurs, while chronic migraineurs who were following RLB were converting to become episodic migraineurs. The power of this study was strengthened by virtue of being performed in a quaternary tier setting with precise diagnostic accuracy and clinical phenotypes.
That this study tested the combined effects of the three domains of RLB (i.e., sleep, exercise, mealtime pattern) supports results from other previous studies which have independently tested and shown the efficacy of each three domains [5, 8, 9]. This study provides evidence that the triumvirate RLB has more favorable impact than regular exercise and regular mealtime alone while regular sleep was found to have identical impact to the RLB triumvirate—hence proving the prominent importance of sleep regulation in headache management. This study will be relevant in employing non-pharmacological evidence-based migraine therapeutic protocols for individualized lifestyle behavior modifications that are applicable in daily clinical practice and beyond. Empowering and reinforcing self-management skills and desirable behaviors of lifestyle modifications will be valuable tool for long-term migraine management and prevention. Behavior modification treatment works through recognized conditioning techniques; reverting and unlearning the very same learning strategies that led to the formation of undesirable and inappropriate behaviors besides teaching new, appropriate and favorable behaviors is central to this type of treatment [26, 27]. Reduction of migraine will be a rewarding experience that will further motivate patients to adopt lifestyle modifications. Results from this study can be directly applied in clinic and community for practice guidance; as the cases and referents in this study are representative of the general population with respect to exposure to RLB. Implementing this will be feasible as it does not require resources other than willingness to learn and adapt. Regularizing daily exercise, consistency in sleep schedule, maintaining adequate sleep hygiene, and consistency in mealtime and hydration pattern is designed to emulate regular therapeutic dosing that are similar to daily medications. Therapeutic tools using evidence-based approaches of lifestyle medicine are practical and achievable both in high- and low-resource settings. Efficacy of lifestyle medicine has been demonstrated for treatment of chronic diseases; while being equipotent to daily medications, lifestyle medicine has the added value of obviating medication risks and unwanted side effects common among chronic migraine sufferers. Self-help manuals, daily journals, and where possible, health application software on mobile phones can strengthen the formation and maintenance of RLB. Lifestyle medicine has the capacity to embrace a system-wide and patient-oriented approach to address the migraineur’s disabling pain beyond focusing on the problem of migraine itself; this allows addressing the limitations of reductionism in realizing best clinical practice. The chronic migraineur is having more than a disease; physical, psychological, social symptoms, and impaired functional status are all essential aspects and determinants of patient outcome satisfaction in the context of biopsychosocial medicine. Synchronized biorhythmicity can be maintained by regular lifestyle behaviors, and this can make the individual migraineur become eventually capable of coping with headache triggers and controlling migraine. The positive results from this case–referent study indicates the need to conduct a full prospective randomized controlled clinical trial to further investigate and validate the role and impact of RLB in migraine management. Our 1-year observation showed the possible causality link between lack of RLB and chronic migraine. The bidirectional and continuous relationship between RLB exposure and reversion of chronic to episodic migraine, and the temporal precedence are evidences for the possible causality link.
Limitations
The limitations of this study were inherent to its design of being cross-sectional. Although this provides an accurate picture of patients attending the clinic currently, we relied on patient data recorded in their medical files to examine the connection between RLB and migraine, rather than collecting data prospectively and monitoring for incident cases, or conducting a controlled randomized trial. Prospective studies will allow deeper probing into the effect of degree of flexibility in maintaining RLB. Prospective studies will further validate causality between lack of RLB and chronic migraine, or whether there is another undetermined factor causing both e.g. high stress level. This study underscores the high priority for developing psychometrically sound measures or wearable devices to track lifestyle behaviors as they relate to migraine—such efforts will avoid the limitations of self-report and improve accuracy of data accrual including real-time datastreaming which can collect actual behavior data rather than self-report data. Data arising from self-report are vulnerable to be underreported or exaggerated.
Conclusion
Engaging in regular lifestyle behavior (RLB) of regular and optimum sleep schedule, daily aerobic exercise, and mealtime and hydration pattern is a moderating factor in migraine; it is protective against developing chronic migraine. Learning this self-regulated behavior can enable the migraineur develop and form a favorable habit which can ultimately help control migraine. Therapeutic tools employing lifestyle behavior changes are practical in both high- and low-resource settings, since they do not require resources other than learning and motivation.
Clinical implications
-
What is already known: Lifestyle behaviors of sleep, exercise, mealtime pattern and hydration status independently affect migraine occurrence
-
What this study adds: Migraine patients who follow all three domains of regular lifestyle behavior with regard to combined regular mealtimes, bedtimes, and daily aerobic exercise are more likely to have episodic than chronic migraine.
References
Buse DC, Andrasik F (2009) Behavioral medicine for migraine. Neurol Clin 27(2):445–465
Sarabdjitsingh RA et al (2010) Recovery from disrupted ultradian glucocorticoid rhythmicity reveals a dissociation between hormonal and behavioural stress responsiveness. J Neuroendocrinol 22(8):862–871
Munch M, Bromundt V (2012) Light and chronobiology: implications for health and disease. Dialogues Clin Neurosci 14(4):448–453
Hashimoto S, Honma S, Honma K (2007) Sleep and biological rhythms. Nihon Yakurigaku Zasshi 129(6):400–403
Kelman L, Rains JC (2005) Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache 45(7):904–910
Hindiyeh NA, Krusz JC, Cowan RP (2013) Does exercise make migraines worse and tension type headaches better? Curr Pain Headache Rep 17(12):380
Darabaneanu S et al (2011) Aerobic exercise as a therapy option for migraine: a pilot study. Int J Sports Med 32(6):455–460
Gil-Martinez A et al (2013) Therapeutic exercise as treatment for migraine and tension-type headaches: a systematic review of randomised clinical trials. Rev Neurol 57(10):433–443
Molarius A, Tegelberg A, Ohrvik J (2008) Socio-economic factors, lifestyle, and headache disorders—a population-based study in Sweden. Headache 48(10):1426–1437
Spigt M et al (2012) A randomized trial on the effects of regular water intake in patients with recurrent headaches. Fam Pract 29(4):370–375
Varkey E et al (2011) Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia 31(14):1428–1438
Martin PR, MacLeod C (2009) Behavioral management of headache triggers: avoidance of triggers is an inadequate strategy. Clin Psychol Rev 29(6):483–495
Wells RE et al (2014) Meditation for migraines: a pilot randomized controlled trial. Headache 54(9):1484–1495
Houle TT et al (2012) Stress and sleep duration predict headache severity in chronic headache sufferers. Pain 153(12):2432–2440
Hufnagl KN, Peroutka SJ (2002) Glucose regulation in headache: implications for dietary management. Expert Rev Neurother 2(3):311–317
Graham JR (1952) The natural history of migraine: some observations and a hypothesis. Trans Am Clin Climatol Assoc 64:61–73 (discussion 73–74)
Andrasik F, Buse DC, Grazzi L (2009) Behavioral medicine for migraine and medication overuse headache. Curr Pain Headache Rep 13(3):241–248
Calhoun AH, Ford S (2007) Behavioral sleep modification may revert transformed migraine to episodic migraine. Headache 47(8):1178–1183
Lowe HJ et al (2009) STRIDE—an integrated standards-based translational research informatics platform. AMIA Annu Symp Proc 2009:391–395
Dupont WD (1988) Power calculations for matched case–control studies. Biometrics 44(4):1157–1168
Headache Classification Committee of the International Headache (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33(9):629–808
von Elm E et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 85(11):867–872
D’Agostino RB (1986) Tests for normal distribution. In: D’Agostino RB, Stephens MA (eds) Goodness-of-fit techniques. Marcel Dekker, New York
Welch BL (1947) The generalisation of student’s problems when several different population variances are involved. Biometrika 34(1–2):28–35
Woldeamanuel YW, Cowan RP (2016) Global migraine epidemiology: systematic review and meta-analysis of 302 community-based studies involving 6,216,995 participants. Headache
Armitage CJ, Norman P, Conner M (2002) Can the theory of planned behaviour mediate the effects of age, gender and multidimensional health locus of control? Br J Health Psychol 7:299–316
Norman P et al (1998) Health locus of control and health behaviour. J Health Psychol 3(2):171–180
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Woldeamanuel, Y.W., Cowan, R.P. The impact of regular lifestyle behavior in migraine: a prevalence case–referent study. J Neurol 263, 669–676 (2016). https://doi.org/10.1007/s00415-016-8031-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8031-5