Abstract
Stroke risk is increased in cancer patients and cancer activity has been claimed to play a role in the development of ischaemic stroke (IS). We wanted to further test these assumptions and to explore the impact of such relation on short-term prognosis. We identified all IS patients that were admitted to the neurological department of our primary and tertiary care university hospital between 2008 and 2014 (n = 4918) and reviewed their medical records for an additional diagnosis of cancer. Cancer patients were categorized into those with “active cancer” (AC: recurrent malignant tumour, metastases, ongoing chemo-/radiotherapy) and “non-active cancer” (NAC). We compared demographic, clinical and neuroimaging features of both patient groups and assessed their association with in-hospital mortality. 300 IS patients with known cancer were identified (AC: n = 73; NAC: n = 227). IS patients with AC were significantly younger (70.3 ± 10.6 vs. 74.9 ± 9.9 years), had more severe strokes at admission (NIHSS: median 5 vs. 3), more frequently cryptogenic strokes (50.7 vs. 32.5 %) and more often infarcts in multiple vascular territories of the brain (26 vs. 5.2 %) compared to IS patients with NAC. In-hospital mortality was significantly higher in AC patients (21.9 vs. 6.2 %). Multivariate analysis identified AC (odds ratio [OR] 3.70, 95 % confidence interval [CI] 1.50–9.30), NIHSS at admission (OR 1.10, CI 1.10–1.20) and C-reactive protein level (OR 1.01, CI 1.00–1.02) as factors significantly and independently associated with in-hospital death. Our findings support a direct role of AC in the pathogenesis and prognosis of acute IS. This needs to be considered in the management and counselling of such patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Malignant cancer and ischaemic stroke (IS) each represent leading causes of death and disability [1]. In addition, previous reports have indicated that stroke risk is increased in cancer patients [2]. It has been suggested that cancer-related coagulation disorders, tumour embolism or adverse effects from oncological treatment could be a trigger for IS [3–6]. Some studies found indirect evidence in this direction such as a lower number of classical stroke risk factors, higher rates of unidentified stroke aetiologies and lesion patterns on magnetic resonance imaging (MRI) suggesting an embolic origin [6–11], while others could not identify clear differences in stroke features between cancer and non-cancer groups [4, 5].
However, the majority of these investigations did not separate between different states and stages of cancer and just focused on stroke patients with active cancer (AC) or were limited by a small size of their study cohort [5–10]. Thus far, only one Korean study has investigated stroke characteristics in cancer patients according to cancer state (active vs. non-active). The authors found an association between AC and higher concentrations of inflammatory markers, a pattern of multiple diffusion weighted imaging (DWI) lesions on MRI and cryptogenic stroke aetiology [11].
We thus aimed to replicate these observations in a European cohort of stroke patients. Furthermore, we particularly focused on post-stroke prognosis of cancer patients, which is also quite controversial and largely unresolved [5, 7, 10]. Whereas AC is clearly associated with a high long-term risk of death among stroke patients, information about the influence of cancer activity on the short-term outcome after stroke is limited [7, 8, 12]. We therefore also investigated the short-term risk of death of IS patients with AC and searched for possible predictors.
Methods
Study design and data collection
We retrospectively identified all IS patients that were admitted to the neurological department of a university hospital between 2008 and 2014 (n = 4918), which also provides primary stroke care for a defined population of the province of Styria. To collect data, the medical and nursing documentation and communication network of Styria (MEDOCS) was used. This hospital information system allows accessing neurological and oncological records as well as neuroimaging and laboratory data acquired in all 21 public hospitals in Styria with more than 1.2 million inhabitants. To be considered for this study, ischaemic cerebral infarction had to be confirmed by brain MRI or computed tomography (CT). All IS patients identified in this manner were reviewed for the presence of an additional diagnosis of cancer and, if positive, included in our investigation. Patients with brain tumours or cerebral metastases were excluded because of the possibility of stroke mechanisms related to local tumour effects.
Considering cancer activity, patients were divided into two cohorts, i.e. those with active (AC) and non-active cancer (NAC). AC was defined as a recurrent malignant tumour, presence of metastases or ongoing chemo- or radiotherapy at hospital admission [13]. Metastases had to be verified by radiological evidence or biopsy. Patients with a diagnosis of cancer who did not meet these criteria were classified as NAC.
Diagnostic stroke workup irrespective of this classification consisted of cerebral MRI or CT, extra- and intracranial duplex sonography, electrocardiography (ECG), 24-h ECG, routine laboratory tests (including coagulation tests, haematology and biochemistry) and transthoracic or transoesophageal echocardiography.
We recorded patient demographics, the presence of cerebrovascular risk factors, previous vascular events, use of drugs affecting blood clotting, clinical symptoms at presentation [using the National Institutes of Health Stroke Scale (NIHSS)] and in-hospital mortality after stroke [6, 14]. In addition, oncological records were carefully reviewed for cancer-specific aspects such as tumour types and cancer therapy.
Stroke aetiology and infarct pattern
Stroke aetiology was defined according to the Trial of ORG 10172 in Acute Stroke Treatment (TOAST)-classification [15]. Furthermore, all available MRI and CT scans were reviewed by a neuroradiological expert for infarct pattern/extension and vessel occlusion, unaware of the patient’s cancer activity. Large vessel disease was considered in the presence of vessel stenosis (≥50 %)/occlusion proximal to ischaemic lesions. Acute subcortical hemispheric or brainstem infarcts with a diameter of less than two centimetres were classified as related to cerebral small vessel disease. Cardioembolism was suspected in the presence of a cardioembolic source without evidence for large or small vessel disease. Finally, cryptogenic stroke was noted if the cause of stroke could not be determined confidently or if at least two possible causes of stroke were present [15]. Cancer was not considered as a distinct aetiology.
Infarct patterns were classified based on cerebral MRI/CT into four groups: (1) single lesion in one vascular territory, (2) scattered lesions in one vascular territory, (3) borderzone infarction and (4) infarcts in multiple vascular territories of the brain [16].
Statistical analysis
All analysis was performed with the IBM Statistical Package of Social Sciences (SPSS)—statistics (version 22.0). For continuous variables, Gaussian distribution was tested with the Kolmogorov–Smirnov test. If Gaussian distribution was identified, we used the Student’s t test to compare the AC and NAC subgroups. Otherwise Mann–Whitney U Test for independent variables was utilized. Categorical variables and frequencies were compared using the Chi-square test. A p value less than 0.05 was considered statistically significant.
A multivariate binary logistic regression model with the occurrence of in-hospital death as the target variable was fitted. In block A, the model was loaded with the variables age and sex. Block B consisted of variables that were significantly associated with the complication of in-hospital death in univariate analysis; thus including AC, infarcts in multiple vascular territories of the brain, NIHSS and C-reactive protein level at hospital admission.
Results
We identified 300 patients [mean age, 73.0 ± 10.5 years; 177 (59.0 %) male] with IS and an additional diagnosis of cancer. Of those, 73 (24.3 %) had active and 227 (75.7 %) non-active concomitant cancer. While 296 patients had a preceding diagnosis of cancer, four individuals had been diagnosed with AC after the index IS.
Among all included patients, arterial hypertension was the most common stroke risk factor (77.6 %), followed by dyslipidemia (38.0 %), atrial fibrillation (33.3 %), nicotine abuse (25.0 %) and diabetes mellitus (20.7 %; for numbers, see Table 1). A previous vascular event (myocardial infarction, stroke, venous thromboembolism) was recorded in 84 (28.0 %) patients. Median NIHSS at hospital admission was 3 (range 0–38) and 30 patients (10.0 %) died during their stay in hospital (median duration of stay: 9, range 2–45 days).
The most frequent cancer types in our IS patients were prostate (20.3 %), breast (15.3 %) and colon carcinoma (12.0 %). Overall, 61.5 % had an adenocarcinoma as the underlying histological cancer subtype (Table 2). Cardioembolism (29.3 %) was the most common stroke aetiology, followed by large vessel disease (21.3 %) and small vessel disease (12.3 %; for numbers see Table 3). 111 (37.1 %) patients were classified as cryptogenic stroke.
Finally, brain imaging [MRI (n = 237; 79 %) and/or CT (n = 279; 93 %)] revealed a total of 187 (62.4 %) IS patients with a single territorial lesion, 64 (21.3 %) with scattered territorial lesions, 31 (10.3 %) with infarcts in multiple vascular territories and 18 (6.0 %) with borderzone infarction (Table 3).
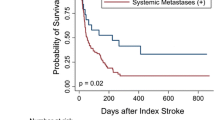
AC versus NAC
IS patients with AC were significantly younger compared to patients with NAC (70.3 ± 10.6 vs. 74.9 ± 9.9, p < 0.001) and suffered from more severe strokes as indicated by a significantly higher NIHSS score (median, 5 vs. 3, p = 0.01). They also had a higher in-hospital mortality, which was 21.9 % in AC compared to 6.2 % in NAC patients (p < 0.001, for numbers see Table 1).
Classical stroke risk factors, including arterial hypertension and dyslipidaemia, were less frequent in AC patients, while the prevalence of previous vascular events did not differ between the subgroups (Table 1). Regarding laboratory markers, AC patients presented with higher CRP levels at stroke onset (28.9 ± 32.5 vs. 11.6 ± 27.9 mg/L, p < 0.001), while routine coagulation tests and leuco-/thrombocyte counts or renal and liver function did not significantly differ between the two subgroups (data not shown).
Stroke aetiology and infarct pattern also differed significantly between the subgroups (Table 3). Thus, cryptogenic stroke was more prevalent in AC patients (50.7 vs. 32.5 %, p = 0.007), while the NAC cohort more often showed cardioembolism and small vessel disease as causes of stroke. Infarcts in multiple vascular territories of the brain were observed significantly more often in AC compared to NAC patients (26 vs. 5.2 %, p < 0.001). Figure 1 shows representative images of the latter infarct pattern.
Representative images of infarcts in multiple cerebrovascular territories. Multiple supra- (a, c) and infratentorial (b, d) acute ischaemic infarcts in a 54-year-old patient with underlying active colon cancer are shown on FLAIR (a, b) and DWI MRI sequences (c, d). MRI magnetic resonance imaging, FLAIR fluid-attenuated inversion recovery, DWI diffusion weighted imaging
Lung, liver and pancreatic carcinoma were especially prevalent in IS patients with AC, who overall also had a higher rate of adenocarcinoma histologically when compared to IS patients with NAC (Table 2).
Multivariate analysis served to identify variables that predicted in-hospital death in ischaemic stroke patients. Variables that remained significantly associated with in-hospital death after adjusting for age and sex were AC [odds ratio (OR) 3.70, 95 % confidence interval (CI) 1.50–9.30], NIHSS at admission (OR 1.10, CI 1.10–1.20) and C-reactive protein level at admission (OR 1.01, CI 1.00–1.02).
Discussion
This analysis in well-characterized central European IS patients with concomitant cancer showed that various characteristics of IS, including age, stroke risk factors, infarct patterns and stroke aetiology differed depending on cancer state (AC vs. NAC). Furthermore, AC was associated with more severe stroke at admission and a higher rate of in-hospital death. These findings support a direct role of AC on IS development and on short-term outcome after stroke.
Although there exists a considerable number of studies that have explored the co-occurrence of stroke and cancer [5–10], reports that have investigated features of stroke according to different cancer state (active vs. non-active) are limited [8, 11]. Only one Korean study associated IS of AC patients with an elevated CRP level, infarcts in multiple vascular territories of the brain and stroke of unidentified aetiology [11]. We here replicate these observations and additionally show a lower mean age at stroke onset with fewer classical stroke risk factors in the AC cohort supporting the assumption of a specific stroke mechanism in patients with an underlying AC [6, 7, 11].
Hypercoagulability is the most likely triggering factor in this cascade. This gains support from the presence of a significant CRP elevation [17, 18] and the type of tumour preferably found in patients with AC. Noteworthy, our AC patients revealed a high proportion of lung, liver and pancreatic cancer and had more often an adenocarcinoma as their underlying cancer histology, which all have been suggested to trigger paraneoplastic thrombosis (Trousseau’s syndrome) [2, 19–21]. The fact that we did not find a higher prevalence of vascular events before the index stroke in our AC patients does not necessarily argue against this explanation as IS may just have been the first sign of cancer-induced endogenous alterations.
Thromboembolism due to hypercoagulability as the cause of IS in AC is also supported by our MRI findings. Analysis of the DWI lesion pattern showed an association between infarcts in multiple vascular territories of the brain and AC. While this infarct pattern has been associated specifically with a proximal and most often cardioembolic source [22], such a stroke aetiology was actually less often diagnosed in patients with AC than NAC.
However, it cannot be excluded that cardioembolic sources may have escaped detection as only few patients underwent transoesophageal echocardiography (12 %). In this context, a prospective echocardiographic study detected valvular vegetations in about 20 % of all cancer patients and suggested a high mortality due to systemic embolism [23]. Also in other studies reporting on the association of IS and cancer, the percentage of transoesophageal echocardiographic workup has been low (10–17 %) and thus have led to underestimation of a cancer-associated cardioembolic source [8, 11].
Another specific scope of the present work was to assess the influence of a cancer activity on stroke severity and short-term outcome after stroke, as data about clinical parameters of stroke patients with concomitant cancer are limited. While the few studies available thus far have reported no major differences, we found that AC patients presented with more severe stroke syndromes at admission (NIHSS: median 5 vs. 3) and had an excessively high in-hospital mortality rate compared to the NAC cohort (21.9 vs. 6.2 %). Based on data from the Austrian Stroke Unit Registry, the short-term mortality after IS with a median NIHSS of 3–4 at admission would be expected to range between 8.6 and 13.9 % [24].
Multivariate regression analysis further revealed that particularly AC, and to a lesser extent NIHSS at admission and CRP elevation were independently associated with in-hospital death. The impact of stroke severity and CRP level at hospital admission, both increased in AC patients in univariate analysis, have been generally related to reduced survival after stroke [17, 24]. Possible reasons why these associations of AC with stroke severity and poor short-term prognosis have not been found in previous studies [5, 7, 8] include relatively small patient groups, patient selection and the absence or differences in the definition of AC.
Our retrospective study has some obvious limitations. First, we did not compare our cancer cohorts to a control group with non-cancer patients. However, previous studies had not revealed substantial differences between NAC and non-cancer patients [8, 11].
Second, the retrospective study design limits our analysis to investigations available from routine workup and does not allow to reliably capturing outcome data after hospital discharge. In view of the likely importance of hypercoagulability, it would have been interesting to also determine the fibrinogen and D-dimer levels in our patients but these are not being obtained on a routine basis. Furthermore, the low autopsy rate of 10.0 % prohibits a reliable analysis of the most plausible cause of death in our patients.
In conclusion, IS in AC shows specific characteristics which support the role of active malignancies in the development of stroke. Pancreatic, lung and liver cancer as well as adenocarcinoma appear particularly prone to cause IS and thromboembolism is the most likely mechanism. In addition, patients with IS and AC have a high rate of in-hospital death.
Clinicians should consider our finding of this poor short-term outcome in the management and counselling of IS patients with an underlying AC.
References
World health organization. Changing history. World health report 2004, pp 120–125
Zöller B, Ji J, Sundquist J, Sundquist K (2012) Risk of haemorrhagic and ischaemic stroke in patients with cancer: a nationwide follow-up study from Sweden. Eur J Cancer 48:1875–1883
Grisold W, Oberndorfer S, Struhal W (2009) Stroke and cancer: a review. Acta Neurol Scand 119:1–16
Cestari DM, Weine DM, Panageas KS, Segal AZ, DeAngelis LM (2004) Stroke in patients with cancer: incidence and aetiology. Neurology 64:2025–2030
Zhang YY, Cordato D, Shen Q, Sheng AZ, Hung WT, Chan DK (2007) Risk factor, pattern, etiology and outcome in ischemic stroke patients with cancer: a nested case-control study. Cerebrovasc Dis 23:181–187
Kim K, Lee JH (2014) Risk factors and biomarkers of ischemic stroke in cancer patients. J Stroke 16:91–96
Schwarzbach CJ, Schaefer A, Ebert A et al (2012) Stroke and cancer: the importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke 43:3029–3034
Karlińska AG, Gromadzka G, Karliński MA, Członkowska A (2015) The activity of malignancy may determine stroke pattern in cancer patients. J Stroke Cerebrovasc Dis 24(2):348–353
Kim SG, Hong JM, Kim HY et al (2010) Ischemic stroke in cancer patients with and without conventional mechanisms: a multicenter study in Korea. Stroke 41:798–801
Navi BB, Singer S, Merkler AE et al (2014) Cryptogenic subtype predicts reduced survival among cancer patients with ischemic stroke. Stroke 45:2292–2297
Lee EJ, Nah HW, Kwon JY, Kang DW, Kwon SU, Kim JS (2014) Ischemic stroke in patients with cancer: is it different from usual stroke. Int J Stroke 9:406–412
Aarnio K, Joensuu H, Haapaniemi E et al (2015) Cancer in young adults with ischemic stroke. Stroke 46:1601–1606. doi:10.1161/STROKEAHA.115.008694
Lee AY, Levine MN, Prins M et al (2003) Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 349(2):146–153
Goldstein L, Samsa G (1997) Reliability of the national institutes of health stroke scale. Stroke 28:307–310
Adams HP, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke 24:35–41
Rolfs A, Fazekas F, Grittner U et al (2013) Acute cerebrovascular disease in the young: the stroke in young fabry patients study. Stroke 44(2):340–349
Rodriguez-Yanez M, Castillo J (2008) Role of inflammatory markers in brain ischemia. Curr Opin Neurol 21:353–357
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Navi BB, Reiner AS, Kamel H et al (2015) Association between incident cancer and subsequent stroke. Ann Neurol 77(2):291–300
Iodice S, Gandini S, Löhr M, Lowenfels AB, Maisonneuve P (2008) Venous thromboembolic events and organ-specific occult cancers: a review and meta-analysis. J Thromb Haemost 6(5):781–788
Wahrenbrock M, Borsig L, Le D, Varki N, Varki A (2003) Selectin-mucin interactions as a probable molecular explanation for the association of Trousseau syndrome with mucinous adenocarcinomas. J Clin Investig 112(6):853–862
Kang DW, Chalela JA, Ezzeddine MA, Warach S (2003) Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol 60:1730–1734
Edoute Y, Haim N, Rinkevich D, Brenner B, Reisner SA (1997) Cardiac valvular vegetations in cancer patients: a prospective echocardiographic study of 200 patients. Am J Med 102(3):252–258
Gattringer T, Ferrari J, Knoflach M et al (2014) Sex-related differences of acute stroke unit care: results from the Austrian stroke unit registry. Stroke 45(6):1632–1638
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest. The authors have nothing to disclose relating to the subject matter of this article.
Funding
This work receives no specific funding.
Ethical Standards
The study was approved by the hospital institutional review board and the ethics committee of the Medical University of Graz.
Rights and permissions
About this article
Cite this article
Kneihsl, M., Enzinger, C., Wünsch, G. et al. Poor short-term outcome in patients with ischaemic stroke and active cancer. J Neurol 263, 150–156 (2016). https://doi.org/10.1007/s00415-015-7954-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7954-6