Abstract
This study sought to determine whether the backward-stepping Push and Release (P&R) Test and the Pull Test, or comprehensive batteries of postural instability (the Mini-BESTest and Brief-BESTest), significantly improve the prediction of future falls beyond knowing a person’s baseline fall history. Complete data were available for 43 of 80 participants with PD. At baseline, participants completed the BESTest (which was scored for all versions and includes the P&R Test), the Unified PD Rating Scale (UPDRS) motor section (which includes the Pull Test), and the participants’ reported falls experienced in the previous 6 months. Participants were classified as recurrent fallers if they reported more than one fall in the 12 months subsequent to baseline. Stepwise logistic regressions determined whether the P&R Test, Pull Test, Brief-BESTest, Mini-BESTest, or UPDRS motor score improved predictions of recurrent fallers independent of baseline fall-group status. Independently, all assessments significantly predicted future recurrent fallers, but only the Mini-BESTest and Brief-BESTest significantly improved predictions of future recurrent fallers independent of baseline fall-group status. The results suggest that, although single tests of reactive postural control do not offer significant predictive benefit, predictions of future recurrent fallers with PD do benefit from a balance examination in addition to knowing whether an individual has a recent history of falls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
People with Parkinson’s disease (PD) are at an increased risk for falls and their sequelae [1]. It is important, therefore, to identify people with PD who are at greatest risk for future falls in order to efficiently prescribe interventions for those who need them. Unfortunately, the best predictor of future falls is a recent history of falls [1], which undermines the potential for targeted preventative interventions. Balance and gait impairment represents one contributing factor to future fall risk [2–4], thus evaluating postural instability could be valuable to improve the prediction of future falls for people with PD. In order for such an evaluation to be useful, though, it must significantly improve predictions of future falls beyond knowledge of a person’s recent fall history, and the evaluation must also be clinically feasible (i.e., fast to perform without requiring significant instrumentation or processing).
The Unified PD Rating Scale (UPDRS) includes a motor section score, and the Pull Test is included within the UPDRS motor exam as a test of postural instability in response to perturbation. The Pull Test, however, exhibits stronger specificity for identifying individuals not at risk for falls with weaker sensitivity for those at risk for falls and, consequently, has not been found sensitive to identifying future fall risk for people with PD [5]. As an alternative, the Push and Release (P&R) Test was found to provide a more reliable perturbation than the Pull Test as well as higher sensitivity for people with PD who report recent falls [6, 7]. The P&R Test, however, still needs to be prospectively evaluated for future fall risk in people with PD [8]. One objective of this study, therefore, is to determine if the P&R Test and Pull Test predict future falls independent of reported fall history.
It has been suggested, however, that fall risk as well as balance and gait impairments are multi-factorial and, thus, require more comprehensive assessment than that provided by a single postural instability test to an external perturbation [8, 9]. The Brief-BESTest [10] and Mini-BESTest [11, 12] each represent clinically feasible balance assessments that were designed to evaluate multiple contexts of postural instability, and each has been found to predict future falls in people with PD [4]. It is not yet determined, though, whether this predictive capacity of the Brief-BESTest and Mini-BESTest improves on predictions based on a person’s fall history. Thus, a second objective of this study is to determine if the Brief-BESTest and Mini-BESTest predict future falls independent of reported fall history. We hypothesized that, independent of baseline fall history, the P&R Test as well as the Brief-BESTest and Mini-BESTest, but not the Pull Test, would provide significant predictors of future falls for people with PD.
Methods
Participants
Participants were recruited from a Movement Disorders center. Individuals were eligible for participation if diagnosed with definite idiopathic PD (Hoehn and Yahr stages I–IV) [13]. Potential participants were excluded if they had: a history or presence of a neurological disorder other than PD or a musculoskeletal injury that limited the ability to walk. Forty-three of the 80 participants tested at baseline completed all assessments at baseline and at the 6-month and 12-month follow-up sessions (Table 1). All participants provided informed consent according to the policies and procedures of the Institutional Human Research Protection Office.
Protocol and explanation of measures
During assessments, participants were on anti-Parkinson’s medication approximately 1.0–1.5 h after administration. Participant characteristics were collected using a custom-designed form. Motor symptom severity was determined using section III of the Movement Disorder Society’s (MDS) version of the UPDRS [14]. A student of physical therapy trained in balance test administration evaluated balance performance using the full, original BESTest [15]. A custom-designed worksheet allowed the examiner to simultaneously record BESTest item scores and Mini-BESTest item scores due to their distinct scoring scales. Brief-BESTest scores were extracted from the relevant items of the original BESTest. Analyses only involve the Brief-BESTest and Mini-BESTest because the length of the original BESTest renders clinical feasibility unlikely. The Pull Test was executed and scored according to the MDS-UPDRS, and the P&R Test was executed and scored according to the original BESTest.
Fall reports and participant classification
Self-reported 6-month fall history was obtained at the baseline, 6-month, and 12-month sessions. Prior to completing the form, each participant was informed that a fall was defined as an unintentional event in which any part of the body comes into contact with the ground. Participants who reported 2 or more falls in the 6 months prior to the baseline assessment were considered recurrent fallers at baseline, and participants who reported 2 or more falls across the follow-up sessions were considered recurrent fallers at follow-up.
P&R Test
The backward-stepping version of the P&R Test involves an examiner standing behind the tested individual with the examiner’s hands on the individual’s scapulae. The individual stands with feet shoulder width apart and their arms down at the sides, then leans into the examiner’s hands, leaning their body backwards through movement about their ankles while maintaining a straight hip angle. The examiner manually supports the individual at a final position such that the hips and shoulders are located just behind the heels. The examiner then releases support and evaluates whether the individual requires multiple steps or assistance in order to recover balance. The response is scored on a 4-point (0–3) ordinal scale, with lower scores representing greater impairment. We note that the 4-point scale of the BESTest’s P&R Test is not the same as the 5-point scale identified in the original description of the P&R Test [6, 15]. Although the BESTest also examines feet-in-place and forward-stepping versions of the P&R Test, only the backward-stepping version was analyzed due to its similarity to the original description of the P&R Test.
Pull Test
The Pull Test involves an examiner standing behind the tested individual, and the individual stands upright with feet comfortably apart and arms down at their sides. Following explanation and a mild practice, the examiner briskly and forcibly pulls on the individual’s shoulders to induce backward stepping and then evaluates the number of steps needed to recover balance or the need for assistance during recovery. The response is scored on a 5-point (0–4) ordinal scale, with higher scores representing greater impairment [14].
MDS-UPDRS motor exam
The MDS-UPDRS motor exam [14] represents an 18-item motor symptom exam that evaluates upper-limb, lower-limb, and speech bradykinesia and hypometria, as well as rigidity, tremor, postural alignment, voluntary postural transitions, reactive postural control to a perturbation (the Pull Test), and gait impairment. Each item is rated on a 5-point (0–4) ordinal scale, with higher scores representing greater impairment, and then a sum score is derived.
Brief-BESTest
The Brief-BESTest [10] is an 8-item balance exam that evaluates hip abductor strength, functional reach, one-leg stance on each leg, lateral P&R tests on each side, stance with eyes closed on a foam surface, and the timed up-and-go test. Each item is rated on a 4-point (0–3) ordinal scale, with lower scores representing greater impairment, and then a sum score is derived.
Mini-BESTest
The Mini-BESTest [11] is a 14-item balance exam that evaluates sit to stand, rise to toes, the most impaired side of one-leg stance, as well as forward, backward, and the most impaired side of lateral P&R tests, stance with eyes open on a firm surface and with eyes closed on a foam surface, stance on an incline with eyes closed, as well as gait with changes in speed, with head turns, with pivot turns, over obstacles, and the dual-task timed up-and-go test. Each item is rated on a 3-point (0–2) ordinal scale, with lower scores representing greater impairment, and then a sum score is derived.
If individuals required an assistive device to complete items in these tests, each version of the BESTest requires that they be scored 1 level lower for each item in which a device is used. If an individual is unable to complete a task with or without a device, they are scored a zero for that item.
Statistical analysis
Total scores of the UPDRS motor exam, Brief-BESTest, and Mini-BESTest were used for statistical analysis, and raw scores were used for the P&R Test and Pull Test. Single-variable logistic regression analyses were conducted to identify fall-group status at follow-up using the baseline fall-group status, Pull Test, P&R Test, Brief-BESTest, Mini-BESTest, and UPDRS motor scores individually as predictors entered into separate models. In order to determine whether the Pull Test or P&R Test could predict future recurrent fallers better than knowledge of baseline fall-group status alone, two forward-stepwise logistic regression models were assessed with baseline fall-group status and either the P&R Test score or the Pull Test score evaluated as potential predictors in the model. In order to determine whether multi-item test batteries, rather than an individual test item, could predict future recurrent fallers better than knowledge of baseline fall-group status alone, three forward-stepwise logistic regressions were also performed with baseline fall-group status and either the UPDRS motor score, Mini-BESTest score, or Brief-BESTest score evaluated as potential predictors in the model. As a preliminary secondary analysis pending further establishment of the measurement properties of individual items, in order to determine if the complete Mini-BESTest or Brief-BESTest is required, multiple-variable stepwise models were generated that included baseline fall status, as well as the total score and individual item scores of either the Mini-BESTest or Brief-BESTest. Receiver operating characteristic (ROC) curves were then generated from the models’ predicted probabilities against fall-group status at follow-up to generate the area under the curve (AUC) for each model.
Results
At baseline, 8 of the 43 participants (19 %) were classified as recurrent fallers, whereas 17 of the 43 participants (40 %) were classified as recurrent fallers by the 12-month follow-up session. Single-variable analysis demonstrates that baseline fall-group status, the Pull Test, the P&R Test, the UPDRS motor exam, the Brief-BESTest, and the Mini-BESTest each individually provide significant predictions of fall-group status at follow-up (Table 2).
The 2-variable stepwise regression models that evaluated baseline fall-group status and either the Pull Test or the P&R Test as potential predictors identified baseline fall-group status as the only significant predictor of fall-group status at the 12-month follow-up. Thus, the statistics identified in Table 2 for the single-variable analysis of baseline fall-group status remain the same for the two-variable analyses (the step increase in χ 2 provided by the Pull Test = 0.98, P = 0.32; the step increase in χ 2 provided by the P&R Test = 2.66, P = 0.10).
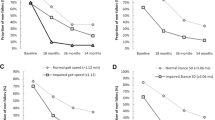
The two-variable stepwise regression models that evaluated baseline fall-group status with either the UPDRS motor scores, Mini-BESTest scores or Brief-BESTest scores identified baseline fall-group status and either the Mini-BESTest or the Brief-BESTest, but not UPDRS motor scores, as significant predictors of fall-group status at the 12-month follow-up (Fig. 1): (1) with the Mini-BESTest, final model χ 2 = 22.54 (P < 0.0001), step increase in χ 2 with addition of the Mini-BESTest = 4.733 (P = 0.030); (2) with the Brief-BESTest, final model χ 2 = 22.02 (P < 0.0001), step increase in χ 2 with addition of the Brief-BESTest = 4.209 (P = 0.040); (3) with the UPDRS motor score, final model χ 2 = 17.81 (P < 0.0001) and did not include the UPDRS motor exam because the step increase in χ 2 with addition of UPDRS motor scores = 2.90 (P = 0.089).
Receiver operating characteristic (ROC) curves identifying the area under the curve (AUC) with 95 % confidence intervals for baseline fall-group status by itself as well as when adding scores from either the Brief-BESTest or the Mini-BESTest, which significantly improved model predictions of fall-group status at the 12-month follow-up
When item scores from the Mini-BESTest or Brief-BESTest were added to these two-variable stepwise regression models, for the Mini-BESTest, baseline fall-group status as well as the items of standing on an incline and walking with pivot turns were identified as significant predictors of fall-group status at the 12-month follow-up: final model χ 2 = 28.87 (P < 0.0001), AUC = 0.898 (0.79–1.0), step increase in χ 2 with addition of incline stance = 5.84 (P = 0.016), further step increase in χ 2 with addition of walk with pivot turn = 5.22 (P = 0.022). For the Brief-BESTest, baseline fall-group status and the item of functional reach were identified as significant predictors of fall-group status at the 12-month follow-up: final model χ 2 = 22.83 (P < 0.0001), step increase in χ 2 with addition of functional reach = 5.02 (P = 0.025), AUC = 0.851 (0.73–0.97).
Discussion
Our hypothesis that, independent of fall history, the P&R Test as well as the Brief-BESTest and Mini-BESTest, but not the Pull Test, would provide significant predictors of future falls for people with PD was only partially supported. Although all assessments could individually predict fall-group status at the 12-month follow-up, the P&R Test, the Pull Test, and the UPDRS motor exam did not significantly improve predictions beyond knowledge of fall-group status at baseline. The Brief-BESTest or Mini-BESTest (or specific item scores of incline stance, walking with pivot turns, and functional reach) did significantly improve predictions of fall-group status at the 12-month follow-up when coupled with fall-group status at baseline.
The lack of improved predictive power of the P&R Test or Pull Test to identify future recurrent fallers beyond predictions from baseline fall history suggests single tasks of reactive postural control are insufficient to identify people without a recent history of falls who are still at risk for future falls. Because item scores in other domains of postural control could independently improve predictions of future falls, this finding likely reflects that reactive postural control to extrinsic perturbation is not a sensitive precursor to falls for people with PD compared to other domains of control. Multiple-item balance and mobility exams have been previously suggested for predicting falls in people with PD [8, 9, 16, 17]. This study corroborates this suggestion due to the improved prediction of recurrent fallers at follow-up when baseline fall history was combined with either the Brief-BESTest, the Mini-BESTest, or items derived from these exams. The lack of significant benefit from the UPDRS motor exam further suggests that any supplemental physical exam is optimized if it specifically focuses on balance and mobility impairment.
Although this study suggests that predicting future recurrent fallers with PD benefits from a balance exam in addition to knowing fall history, the purpose of this study was not to identify an optimal set of balance tests specifically for this purpose. Others have suggested various combinations of test items for future fall prediction in people with PD [9, 16, 18], and this study identified that incline stance, walking with pivot turns, and functional reach (as scored by the Mini-BESTest or Brief-BESTest) provide similar predictive capacity as the complete Mini-BESTest or Brief-BESTest exams. We cannot yet recommend use of the stand-alone items over the complete exams, though, because the measurement properties of the stand-alone items are not yet well established. Thus, this analysis should be viewed as a preliminary validation of the stand-alone items for this purpose of identifying fall risk within our sample’s characteristics. We, therefore, suggest using a standard balance assessment such as the Mini-BESTest or Brief-BESTest until further studies can confirm the measurement properties of a more efficient sub-set of items. Until proven unnecessary with future study, using a complete standardized exam further ensures evaluation of multiple contexts of balance and mobility impairment in order to address the theoretical supposition that the multi-factorial nature of balance and mobility must be considered in order to adequately evaluate fall risk [8].
Other methodological considerations include the use of the BESTest’s version of the P&R Test and scoring, which differs from the test’s original publication [6]. It has yet to be determined which scoring method provides superior assessment. In addition, a large portion of the initial study sample did not complete follow-up assessments. The primary causes for this loss to follow-up were an inability to contact the subject at follow-up or a decline in health condition (details reported in [4]), and these subjects were more severely affected by PD than those who were included for analysis. Therefore, further study will need to evaluate the generalizability of these findings to people who are more severely affected by symptoms of PD. Lastly, although the study is prospective regarding the use of baseline assessments with subsequent fall reports, the reporting, even in follow-up, still represented a retrospective report of the previous 6 months rather than making use of a formal fall diary or another method of immediate fall reporting. Thus, fall reports may not be accurate due to mis-remembering. Unlike a true retrospective report, however, the participants were aware of their participation in the study and need of future fall reports, which likely rendered them more attentive to the experience of any fall events. This attentiveness was further supplemented with advance knowledge of how to define fall events.
In summary, this study demonstrates that several clinical tests of balance and mobility impairments are capable of predicting future falls, but we confirm that the experience of recent falls remains the strongest predictor of future falls for individuals with PD [1]. We also demonstrate, however, that the Mini-BESTest and Brief-BESTest, as well as some specific items within these exams, can improve predictions of future recurrent fallers when paired with fall history reports. Our results, therefore, strengthen previous analyses that demonstrated these tests’ ability to predict future falls [4], but which did not assess their capacity to improve predictions of future falls despite knowledge of recent fall history. This study is also the first to evaluate the P&R Test for prospective fall prediction. As single tests of reactive postural instability, however, the P&R Test and Pull Test were less impactful to improve these predictions of future recurrent fallers with PD. Likewise, the more generalized motor-symptom exam of the UPDRS was less impactful in improving predictions of future recurrent fallers than specific balance and mobility tests. Clinicians, therefore, may benefit from specifically evaluating balance and mobility impairment in addition to asking patients about recent fall history. Although not tested in this study, a multi-item balance exam may have the additional benefit of directing preventative interventions against identified impairments for those individuals who are classified to be at risk for future falls. Whereas some studies of gait, balance, or exercise training have reported decreased incidence of falls after treatment (e.g., [19–21]), meta-analyses demonstrate that not all exercise training ubiquitously protects against falls for people with PD [22, 23]. Thus, further research is necessary to identify optimal interventions that clinicians can prescribe to mitigate the risk they identify by knowing a person’s fall history and performance on balance exams. The ability to identify fall risk independent of fall history, though, at least presents a path for targeted preventative interventions.
References
Pickering RM, Grimbergen YA, Rigney U, Ashburn A, Mazibrada G, Wood B, Gray P, Kerr G, Bloem BR (2007) A meta-analysis of six prospective studies of falling in Parkinson’s disease. Mov Disord 22(13):1892–1900. doi:10.1002/mds.21598
Latt MD, Lord SR, Morris JG, Fung VS (2009) Clinical and physiological assessments for elucidating falls risk in Parkinson’s disease. Mov Disord 24(9):1280–1289. doi:10.1002/mds.22561
Kerr GK, Worringham CJ, Cole MH, Lacherez PF, Wood JM, Silburn PA (2010) Predictors of future falls in Parkinson disease. Neurology 75(2):116–124. doi:10.1212/WNL.0b013e3181e7b688
Duncan RP, Leddy AL, Cavanaugh JT, Dibble LE, Ellis TD, Ford MP, Foreman KB, Earhart GM (2013) Comparative utility of the BESTest, mini-BESTest, and brief-BESTest for predicting falls in individuals with Parkinson disease: a cohort study. Phys Ther 93(4):542–550. doi:10.2522/ptj.20120302
Bloem BR, Grimbergen YA, Cramer M, Willemsen M, Zwinderman AH (2001) Prospective assessment of falls in Parkinson’s disease. J Neurol 248(11):950–958
Jacobs JV, Horak FB, Tran VK, Nutt JG (2006) An alternative clinical postural stability test for patients with Parkinson’s disease. J Neurol 253(11):1404–1413. doi:10.1007/s00415-006-0224-x
Valkovic P, Brozova H, Botzel K, Ruzicka E, Benetin J (2008) Push-and-release test predicts Parkinson fallers and nonfallers better than the pull test: comparison in OFF and ON medication states. Mov Disord 23(10):1453–1457. doi:10.1002/mds.22131
Nonnekes J, Goselink R, Weerdesteyn V, Bloem BR (2015) The retropulsion test: a good evaluation of postural instability in Parkinson’s disease? J Parkinson’s Dis 5(1):43–47. doi:10.3233/JPD-140514
Jacobs JV, Horak FB, Tran VK, Nutt JG (2006) Multiple balance tests improve the assessment of postural stability in subjects with Parkinson’s disease. J Neurol Neurosurg Psychiatry 77 (3):322–326. doi:10.1136/jnnp.2005.068742
Padgett PK, Jacobs JV, Kasser SL (2012) Is the BESTest at its best? A suggested brief version based on interrater reliability, validity, internal consistency, and theoretical construct. Phys Ther 92(9):1197–1207. doi:10.2522/ptj.20120056
Franchignoni F, Horak F, Godi M, Nardone A, Giordano A (2010) Using psychometric techniques to improve the Balance Evaluation Systems Test: the mini-BESTest. J Rehabil Med 42(4):323–331. doi:10.2340/16501977-0537
Franchignoni F, Godi M, Guglielmetti S, Nardone A, Giordano A (2015) Enhancing the usefulness of the Mini-BESTest for measuring dynamic balance: a Rasch validation study. Eur J Phys Rehabil Med 51(4):429–437
Racette BA, Rundle M, Parsian A, Perlmutter JS (1999) Evaluation of a screening questionnaire for genetic studies of Parkinson’s disease. Am J Med Genet 88(5):539–543
Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, Poewe W, Sampaio C, Stern MB, Dodel R, Dubois B, Holloway R, Jankovic J, Kulisevsky J, Lang AE, Lees A, Leurgans S, LeWitt PA, Nyenhuis D, Olanow CW, Rascol O, Schrag A, Teresi JA, van Hilten JJ, LaPelle N, Movement Disorder Society URTF (2008) Movement disorder society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 23(15):2129–2170. doi:10.1002/mds.22340
Horak FB, Wrisley DM, Frank J (2009) The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys Ther 89(5):484–498. doi:10.2522/ptj.20080071
Canning CG, Paul SS, Nieuwboer A (2014) Prevention of falls in Parkinson’s disease: a review of fall risk factors and the role of physical interventions. Neurodegener Dis Manag 4(3):203–221. doi:10.2217/nmt.14.22
Paul SS, Canning CG, Sherrington C, Lord SR, Close JC, Fung VS (2013) Three simple clinical tests to accurately predict falls in people with Parkinson’s disease. Mov Disord 28(5):655–662. doi:10.1002/mds.25404
Duncan RP, Cavanaugh JT, Earhart GM, Ellis TD, Ford MP, Foreman KB, Leddy AL, Paul SS, Canning CG, Thackeray A, Dibble LE (2015) External validation of a simple clinical tool used to predict falls in people with Parkinson disease. Parkinsonism Relat Disord. doi:10.1016/j.parkreldis.2015.05.008
Shen X, Mak MK (2015) Technology-assisted balance and gait training reduces falls in patients with Parkinson’s disease: a randomized controlled trial with 12-month follow-up. Neurorehabil Neural Repair 29(2):103–111. doi:10.1177/1545968314537559
Goodwin VA, Richards SH, Henley W, Ewings P, Taylor AH, Campbell JL (2011) An exercise intervention to prevent falls in people with Parkinson’s disease: a pragmatic randomised controlled trial. J Neurol Neurosurg Psychiatry 82(11):1232–1238. doi:10.1136/jnnp-2011-300919
Protas EJ, Mitchell K, Williams A, Qureshy H, Caroline K, Lai EC (2005) Gait and step training to reduce falls in Parkinson’s disease. NeuroRehabilitation 20(3):183–190
Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, Shah L, Sackley CM, Deane KH, Wheatley K, Ives N (2013) Physiotherapy versus placebo or no intervention in Parkinson’s disease. Cochrane Database Syst Rev 9:CD002817. doi:10.1002/14651858.CD002817.pub4
Allen NE, Sherrington C, Paul SS, Canning CG (2011) Balance and falls in Parkinson’s disease: a meta-analysis of the effect of exercise and motor training. Mov Disord 26(9):1605–1615. doi:10.1002/mds.23790
Acknowledgments
This work was supported by the Davis Phinney Foundation, American Parkinson Disease Association (APDA), Greater St. Louis APDA and the APDA Center for Advanced Research at Washington University in St. Louis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest.
Ethical standard
The study was approved by the institutional review board and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Rights and permissions
About this article
Cite this article
Jacobs, J.V., Earhart, G.M. & McNeely, M.E. Can postural instability tests improve the prediction of future falls in people with Parkinson’s disease beyond knowing existing fall history?. J Neurol 263, 133–139 (2016). https://doi.org/10.1007/s00415-015-7950-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7950-x