Abstract
To investigate the frequency and pattern of orthostatic hypotension (OH) associated with acute isolated cerebellar infarction, and to identify the cerebellar structure(s) potentially responsible for OH, 29 patients (mean age 60.0) with acute isolated cerebellar infarction performed a standard battery of autonomic function tests including the head up tilt test using Finapres for recording of the beat-to-beat BP response during the acute period. Cerebellar infarction related OH was defined as fall in BP (>20 mmHg systolic BP) on tilting in patients without any disease(s) that could potentially cause autonomic dysfunction, or in patients who had a potential cause of autonomic dysfunction, but showed the absence of OH during a follow-up test. The severity and distribution of autonomic dysfunction were measured by the composite autonomic severity score (CASS). Nine patients (31 %) had OH (range 24–53 mmHg) on tilting during the acute period. Most patients (7/9) had a remarkable decrement in systolic BP immediately upon tilting, but OH rapidly normalized. Mean of maximal decrease in systolic BP during head up tilt test was 37.0 mmHg. The OH group showed mild autonomic dysfunctions (CASS, 3.7) with adrenergic sympathetic dysfunction appearing as the most common abnormality. Lesion subtraction analyses revealed that damage to the medial part of the superior semilunar lobule (Crus I) and tonsil was more frequent in OH group compared to non-OH group. Cerebellar infarction may cause a brief episode of OH. The medial part of the superior semilunar lobule and tonsil may participate in regulating the early BP response during orthostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orthostatic hypotension (OH), the most incapacitating sign of an autonomic failure, is defined as a decrease in systolic BP (SBP) of greater than 20 mmHg or a decrease in diastolic BP (DBP) of greater than 10 mmHg on standing or head-up tilt [1]. The most easily recognized symptom of OH is orthostatic dizziness, which is characterized by non-vertiginous light-headedness when patients rise to a standing position from a sitting or supine position. Impaired sympathetic vasoconstriction reflex in muscles and splanchnic vessels in response to orthostatic stress can cause OH. OH has been reported in patients with focal central nervous system lesions involving the brainstem, hypothalamus, or spinal cord [2, 3].
The cerebellum has also been reported to participate in regulating BP, presumably by modulating vestibulo-sympathetic responses. However, studies on the role of the cerebellum in regulating BP have been mostly based on the results of experimental animal studies [4–8]. Until now, few studies [9, 10] have described OH associated with isolated cerebellar lesion in humans. The cardiovascular response during orthostasis after a cerebellar lesion still remains uncertain in humans.
Recently, we reported a patient [10] who had OH on tilt test during the acute period of cerebellar infarction and felt orthostatic dizziness after the initial spontaneous dizziness subsided. To the best of our knowledge, no consecutive clinical series has focused on the autonomic dysfunction with OH from an acute isolated cerebellar infarction. The aims of this study were to investigate the frequency and pattern of OH, and to identify the structure(s) within the cerebellum responsible for OH.
Methods
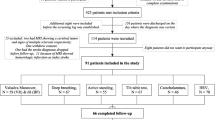
From April 2011 to November 2013, we identified 96 consecutive patients from the acute stroke registry at the Keimyung University Dongsan Medical Center who had an isolated cerebellar infarction diagnosed by brain MRIs including diffusion view. Because the principal purpose of our study was to determine whether the cerebellar infarction itself could cause OH, we excluded (1) patients with anterior inferior cerebellar artery (AICA) territory cerebellar infarction who had an accompanying inner ear infarction with audiovestibular loss (n = 4), (2) patients with additional brainstem or supratentorial lesions including stroke and microangiopathy (n = 23), and (3) patients with a recent history of acute infection, brain edema, or dehydration that could potentially lead to a transient deterioration of autonomic dysfunction (n = 10). According to the above exclusion criteria, 37 patients with acute cerebellar infarction were excluded. Twenty-five patients did not agree to sign on the patient consent form. Thus, 34 patients performed autonomic function tests. We also excluded the patients (n = 5) with medical disease(s) such as diabetes or cardiac disease that could potentially affect the autonomic function who showed OH at both the initial and follow-up tilt tests because OH might result from the medical disease itself (for example, diabetic autonomic neuropathy) rather than the cerebellar lesion itself in these patients. Overall, 67 patients were excluded. Finally, 29 consecutive patients (22 men, age range 41–79 years, mean age 60.0 ± 11.5 years) with unilateral isolated cerebellar infarction who underwent a standardized battery of autonomic function tests during the acute period were included for this study. All had vertigo/dizziness as an accompanying symptom. Limb dysmetria, gait ataxia, truncal instability, and/or nystagmus were common accompanying signs. Patients taking medications known to cause OH or otherwise affect autonomic testing were asked to discontinue use of the drug for 5 half-lives. In all patients, MRIs were performed shortly after the onset of symptoms (mean interval: 3.9 h, range 1–168 h). The territories of the three major cerebellar arteries, including the posterior inferior cerebellar artery (PICA), AICA, and superior inferior cerebellar artery (SCA), were determined according to MR-anatomic templates, a previously validated MR-anatomic template for the delineation of the arterial territory [11]. The vascular territory was determined by consensus between two neurologists (HL, H-AK) who independently reviewed the MRIs. A neuroradiologist (H-WJ) who was blinded to each patient’s clinical status reviewed MRIs in each patient. Complete agreement was achieved between the two neurologists’ estimation of an involved vascular territory and a neuroradiologist’s adjudication.
A standardized battery of autonomic tests, including the head-up tilt test (HUT), Valsalva maneuver, Valsalva ratio, heart rate response to deep breathing using Finometer devices (FMS, Amsterdam, The Netherlands) for recording the beat-to-beat BP and heart rate (HR) responses, and the quantitative sudomotor axon reflex test, was performed during the acute period (3–18 days; mean interval, 8.0 days) in all patients according to a previously validated method for diagnosing autonomic dysfunction [12]. All patients (n = 4) with medical condition(s) that might have caused OH on the first HUT test during the acute period underwent a follow-up HUT test (mean follow-up interval from the initial test: 36.7 days). The tilt protocol included 10 min in the supine position and 20 min of tilt at 70°. OH was defined as a decrease in SBP of at least 20 mmHg or a decrease in DBP of at least 10 mmHg between supine rest for 10 min and an upright posture for 20 min. Classic OH was defined as a decrease in SBP > 20 mmHg or in DBP > 10 mmHg within 3 min of tilting. Delayed OH was defined as a decrease in SBP that occurred after 3 min of tilting. Early OH was characterized as a decrease in SBP of at least 30 mmHg, immediately (usually within 30 s) after tilting with rapid normalization of the BP response after few minutes. Early pattern of OH has been previously verified in patients with orthostatic dizziness [13]. The pattern and severity of autonomic dysfunctions in patients with cerebellar infarction were determined based on the composite autonomic severity score (CASS, range 0–10) that consisted of each subscore evaluating the sympathetic adrenergic and cholinergic, and parasympathetic cardiovagal autonomic functions [14].
Cerebellar OH group was defined as follows: (1) HUT test documented OH during the acute period, and at least one of the following two conditions was satisfied: (2) patients had no medical disease(s) that could potentially cause OH, or (3) patients had medical disease(s) that could possibly have caused OH during an initial HUT test but showed no OH on a follow-up HUT test. The patients with acute isolated cerebellar infarction who showed no OH during an initial HUT test were assigned to no cerebellar OH group, irrespective of medical disease.
To identify the structures involved in the generation of OH, the overlapping lesions of the cerebellar OH group were subtracted from those of the no cerebellar OH group and vice versa, revealing a percentage overlay plot. We used DWIs obtained within the first 48 h after stroke onset and fluid-attenuated inversion recovery sequences when imaging was conducted 48 h or later for the overlay technique and volume measurement. We combined the MRI images of the cerebellar OH group and no cerebellar OH group by flipping the image of the lesions of the right brain-damaged subjects to the left side. Thus, all MRI images were viewed anatomically the left side of the figure, which corresponded to the left side of the brain. The extent of the cerebellar infarctions were drawn directly onto the patient’s individual digitized MRI using MRIcro software (http://www.cabiatl.com/mricro/mricron/index.html) and saved as a region of interest (ROI). Spatial normalization to a spatially unbiased infratentorial (SUIT) template was performed according to the technique described by Diedrichsen [15, 16].
One patient [10] was previously reported, but new information is included in this report. All of the experiments complied with the tenets of the Declaration of Helsinki and the study protocol was reviewed and approved by our institutional review board. Written informed consent was obtained from patients with acute cerebellar infarction after the nature and possible consequences of the study had been explained to the participants.
Results
Among the 29 patients with acute isolated cerebellar infarction who were finally enrolled for this study according to above inclusion and exclusion criteria, 14 patients had PICA territory infarction and 7 had SCA territory infarction. Others (n = 8) had infarction in the combined territories of PICA and SCA. Four patients had lesion including to the posterior vermis, but none of patients had lesion to the fastigial nuclei. Among four patients with lesion to the posterior vermis, two were assigned to the cerebellar OH group.
A total of 9 patients (31 %) had OH during the first HUT test. All patients with OH showed a normal level of blood urea nitrogen (range 8–18 mg/dl; mean, 12 mg/dl) and had no dehydration signs such as an absence of the jugular venous distention. Most (7/9, 78 %) patients showed an initial decrease in SBP of 30 mmHg or more within 30 s after tilting, but OH rapidly normalized (i.e., early OH). Classic OH occurred in 1 patient during the first 3 min of tilting and continued until tilt back. Another patient had delayed OH, which occurred approximately 20 min after tilting. Illustrative case with a typical early pattern of OH during tilting is shown in Fig. 1. During the HUT test, three patients (one early, one classic, and one delayed pattern) with OH felt postural lightheadedness and nausea, which occurred at the time of OH occurrence. A total of eight (28 %) reported a new type of dizziness during hospitalization after the initial spontaneous vertigo/dizziness subsided that was characterized by short-lasting postural lightheadedness, triggered by a standing position from a sitting or supine position (i.e., orthostatic dizziness). None of the patients had symptoms of orthostatic intolerance such as orthostatic dizziness prior to the infarction.
MRI and head-up tilt test (HUT) in a patient with orthostatic hypotension. a Brain MRI scans performed 24 h after the onset of symptoms show hyperintense lesions involving the caudal cerebellum in the territory of the posterior inferior cerebellar artery on the left side. b A HUT test performed 3 days after symptom onset shows a decrease in systolic blood pressure (BP) of up to 60 mmHg immediately after tilting, and the BP then spontaneously and rapidly returns to normal, producing a short period of hypotension (<1 min). Note the increase in heart rate, suggesting an intact compensatory cardiovagal response. c A follow-up HUT test 2 weeks after symptom onset shows normal BP responses
Nine (31 %) patients with OH during the first HUT were classified as the cerebellar OH group, in whom 4 patients had medical diseases including hypertension (n = 4) and diabetes (n = 1), but a follow-up HUT test showed no OH in these patients. Other (n = 20, 69 %) with no OH during tilting were assigned to no cerebellar OH group. There were no differences between the cerebellar OH and no cerebellar OH groups in terms of age, sex, interval from symptom onset to test, involved vascular territory, or frequency of orthostatic dizziness. The mean of maximal decrease in SBP during tilt was 37 mmHg in cerebellar OH group. The total and adrenergic CASS scores were significantly higher in the cerebellar OH group than in the no cerebellar OH group. The patients in the cerebellar OH group showed mild autonomic dysfunction (mean CASS score, 3.7), among which the adrenergic dysfunction was the most common abnormality (Table 1). Lesion subtraction analyses revealed that damage to the medial part of the superior semilunar lobule (Crus I) and the tonsil was more frequent in the cerebellar OH group than in the no cerebellar OH group (Fig. 2).
Overlapping MRI lesions in patients with (A) or without (B) OH. Right-sided lesions are flipped to the left side. The number of overlapping lesions is illustrated by different colors that code for increasing frequencies, which range from violet (n = 1) to red (n = 9 for A, n = 20 for B). Overlay plot of the subtracted superimposed lesions of patients with OH minus no cerebellar OH group. c The percentage of overlapping lesions of the group with OH after subtraction of the no cerebellar OH group is illustrated by five different colors, where dark red represents a difference of 1–20 % and white- yellow represents a difference of 81–100 %. Each color represents increments of 20 %. The regions are colored from dark blue (difference of 1–20 %) to light blue (difference of 81–100 %), indicating regions that were damaged more frequently in patients without OH. The Talairach z coordinates of each transverse slice are given. This figure demonstrates that the medial part of the superior semilunar lobule and tonsil are the anatomical areas related to OH. d The areas including the superior semilunar lobule and tonsil are selectively shown
Discussion
To the best of our knowledge, this is the first study to investigate the frequency and pattern of OH due to acute unilateral cerebellar infarction, and the region(s) within the cerebellum responsible for OH. In our series, OH was found in 31 % of the patients and the most common pattern of OH was early OH, which was observed in approximately 80 % (7/9) of the patients with OH. The medial part of the superior semilunar lobule and tonsil were more commonly damaged in the cerebellar OH group than in no cerebellar OH group.
It was surprising that approximately 30 % of the patients with isolated cerebellar infarction showed OH during tilting. Because of the beat-to-beat BP recording, we could identify brief episodes of transient OH, such as early OH, which constituted approximately 80 % of the total OH observed in our study.
Interestingly, none of our patients with OH showed damage to the caudal vermis including the uvula-nodulus (lobules IX–X) and the fastigial nucleus, which are the structures within the cerebellum thought to participate in cardiovascular control from the results of animal studies [4, 5, 7]. Instead, the medial portion of the superior semilunar lobule and tonsil were more commonly damaged in patients with OH than in those without OH. However, the results from lesion studies in patients do not always correspond to the results from experimental animal studies. For example, in a study [17] on structures responsible for unidirectional gaze-evoked nystagmus in patients with acute cerebellar infarction, none of the patients with unidirectional gaze-evoked nystagmus had a lesion in the flocculus, which is known to play a primary role in the gaze-holding neural integrator network [18]. Furthermore, our result is in agreement with a previously reported patient [9] who showed OH due to a cerebellar tumor confined to the cerebellar hemisphere, supporting the concept that the cerebellar hemispheres might also play a role in the cardiovascular regulation mechanism in addition to the uvula-nodulus (lobules IX–X) and fastigial nucleus. Although the cerebellar hemisphere has no direct effect on the baroreceptor reflex arch, the medial portions of the cerebellar hemispheres are known to project to the globose and emboliform nuclei [19]. These structures have direct connections with the hypothalamus, which is important in the basal and reflex control of sympathetic outflow [20]. Indeed, various parts of the cerebellum, such as the caudal vermis including the uvula-nodulus (lobules IX–X), fastigial nucleus, and anterior vermis (lobules I–III), have been known to participate in cardiovascular control via the baroreflex or the vestibulo-sympathetic reflex. We speculate that the medial portions of the cerebellar hemispheric areas and tonsil may also participate in regulating the BP response during postural changes.
Most (7/9, 78 %) of the cerebellar OH group showed early OH during tilting, which was characterized by a decrease in SBP of 30 mmHg or more within 30 s after tilting with OH rapidly normalizing after few minutes. Early pattern of OH has been previously verified in our study in patients with orthostatic dizziness [13]. Early OH observed in our patients resembles an initial OH, a frequent but underestimated cause of orthostatic intolerance [21]. Similar to an initial OH, this early OH is also accompanied by a remarkable decrement of SBP during the initial period of tilting, followed by a rapid and spontaneous normalization of BP [13]. Thus, the period of hypotension is short. Unlike an initial OH that is exclusively associated with active standing up [21], early OH may occur in a condition of passive tilting, as observed in our patients [13]. Our result is in agreement with previous experimental animal studies [22, 23] that examined the effect of the labyrinth or vestibular nucleus lesions on cardiovascular dysregulation and showed that a decrease in BP after orthostatic stress (i.e., tilting) following a vestibular lesion is prominent only during the early period (within 30 s) after orthostatic stress, and BP then rapidly normalizes. Thus, cerebellar lesions may also cause an early pattern of OH similar to the effects of vestibular lesions observed in experimental animal studies [22, 23].
Because of the complete absence of OH at a follow-up HUT test, four patients who had both medical disease and OH during the first HUT test were included in the cerebellar OH group. Indeed, OH might result from the cerebellar lesion itself rather than from medical disease in these patients. We believe that the possibility of OH associated with one or more underlying medical disease, such as diabetes or cardiac disease, is extremely low in these patients.
Because approximately 30 % (8/29) of patients experienced postural lightheadedness after the initial spontaneous vertigo/dizziness subsided, OH should be considered in the differential diagnosis of dizziness in patients with cerebellar infarction if the patients complain of a new type of dizziness that is typically triggered by a standing position from a sitting or supine position after the initial spontaneous dizziness subsides. In this condition, autonomic function testing rather than diffusion-weighted MRI may be a more effective tool in diagnosing this new type of dizziness.
Our study has some limitations. First, the number of patients was relatively small, and in particular, the small number of patients with cerebellar OH might have lessened the significance of the extracted lesion in these patients. Thus, the possible contribution of the cerebellar hemisphere and/or tonsil related to OH should be investigated again with a large sample size. Second, since OH on HUT test is variably reproducible [24], lack of OH on a second tilt test may not guarantee that the medical conditions were not responsible for OH on the first tilt test. However, frequency of hypertension and diabetes were not significantly different in both cerebellar OH and no cerebellar OH groups. Thus, we believe that the possibility of no OH due to limitation (i.e., low reproducibility) of HUT test was extremely low in these patients (n = 4). Third, because we did not perform a follow-up HUT test in the patients with no medical condition potentially affecting autonomic function who had OH on first HUT test during the acute period, the possibility of idiopathic autonomic failure, such as pure autonomic failure, could not be excluded completely in these patients. Finally, a further study using a standardized dizziness questionnaire, including the onset (i.e., interval from the disappearance of initial dizziness to the onset of new dizziness), frequency, and duration of orthostatic dizziness is needed to clarify the characteristics of this new type of dizziness that occurs after the spontaneous persistent dizziness subsides.
References
(1996) Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurology 46:1470
Claydon VE, Steeves JD, Krassioukov A (2006) Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord 44:341–351
Hsu CY, Hogan EL, Wingfield W Jr et al (1984) Orthostatic hypotension with brainstem tumors. Neurology 34:1137–1143
Bradley DJ, Pascoe JP, Paton JF, Spyer KM (1987) Cardiovascular and respiratory responses evoked from the posterior cerebellar cortex and fastigial nucleus in the cat. J Physiol 393:107–121
Chen CH, Williams JL, Lutherer LO (1994) Cerebellar lesions alter autonomic responses to transient isovolaemic changes in arterial pressure in anaesthetized cats. Clin Auton Res 4:263–272
Yates BJ, Miller DM (2009) Integration of nonlabyrinthine inputs by the vestibular system: role in compensation following bilateral damage to the inner ear. J Vestib Res 19(183–18):9
Holmes MJ, Cotter LA, Arendt HE, Cass SP, Yates BJ (2002) Effects of lesions of the caudal cerebellar vermis on cardiovascular regulation in awake cats. Brain Res 938:62–72
Miller DM, Cotter LA, Gandhi NJ et al (2008) Responses of rostral fastigial nucleus neurons of conscious cats to rotations in vertical planes. Neuroscience 155(317–3):25
Ruchoux MM, Gray F, Gherardi R, Schaeffer A, Comoy J, Poirier J (1986) Orthostatic hypotension from a cerebellar gangliocytoma (Lhermitte-Duclos disease). Case report. J Neurosurg 65:245–248
Lee H, Kim HA (2014) Reversible orthostatic hypotension in PICA territory cerebellar infarction. J Neurol Sci 341:187–188
Tatu L, Moulin T, Bogousslavsky J, Duvernoy H (1996) Arterial territories of human brain: brainstem and cerebellum. Neurology 47:1125–1135
Low PA, Benarroch EE (2008) Clinical autonomic disorders, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Kim HA, Yi HA, Lee H (2014) Spectrum of autonomic dysfunction in orthostatic dizziness. Clin Neurophysiol 125:1248–1254
Low PA (1993) Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc 68:748–752
Diedrichsen J (2006) A spatially unbiased atlas template of the human cerebellum. Neuroimage 33:127–138
Diedrichsen J, Balsters JH, Flavell J, Cussans E, Ramnani N (2009) A probabilistic MR atlas of the human cerebellum. Neuroimage 46:39–46
Baier B, Dieterich M (2011) Incidence and anatomy of gaze-evoked nystagmus in patients with cerebellar lesions. Neurology 76:361–365
Zee DS, Yamazaki A, Butler PH, Gucer G (1981) Effects of ablation of flocculus and paraflocculus of eye movements in primate. J Neurophysiol 46:878–899
Press GA, Murakami J, Courchesne E et al (1989) The cerebellum in sagittal plane-anatomic-MR correlation: 2. The cerebellar hemispheres. AJR Am J Roentgenol 153:837–846
Zhu JN, Yung WH, Kwok-Chong Chow B, Chan YS, Wang JJ (2006) The cerebellar-hypothalamic circuits: potential pathways underlying cerebellar involvement in somatic-visceral integration. Brain Res Rev 52:93–106
Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME (2007) Initial orthostatic hypotension: review of a forgotten condition. Clin Sci (Lond) 112:157–165
Jian BJ, Cotter LA, Emanuel BA, Cass SP (1985) Yates BJ (1999) Effects of bilateral vestibular lesions on orthostatic tolerance in awake cats. J Appl Physiol 86:1552–1560
Mori RL, Cotter LA, Arendt HE, Olsheski CJ, Yates BJ (1985) Effects of bilateral vestibular nucleus lesions on cardiovascular regulation in conscious cats. J Appl Physiol 98:526–533
Ward C, Kenny RA (1996) Reproducibility of orthostatic hypotension in symptomatic elderly. Am J Med 100:418–422
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standard
All of the experiments complied with the tenets of the Declaration of Helsinki and the study protocol was reviewed and approved by our institutional review board. Written informed consent was obtained from patients with acute cerebellar infarction after the nature and possible consequences of the study had been explained to the participants.
Conflicts of interest
None.
Source of funding
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea Government (MSIP) (No. 2014R1A5A2010008).
Rights and permissions
About this article
Cite this article
Kim, HA., Lee, H. Orthostatic hypotension in acute cerebellar infarction. J Neurol 263, 120–126 (2016). https://doi.org/10.1007/s00415-015-7945-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-015-7945-7