Abstract
Fatigue in multiple sclerosis (MS) is a highly disabling symptom. Among the central mechanisms behind it, an involvement of sensorimotor networks is clearly evident from structural and functional studies. We aimed at assessing whether functional/structural balances of homologous sensorimotor regions—known to be crucial for sensorimotor networks effectiveness—decrease with MS fatigue increase. Functional connectivity measures at rest and during a simple motor task (weak handgrip of either the right or left hand) were derived from primary sensorimotor areas electroencephalographic recordings in 27 mildly disabled MS patients. Structural MRI-derived inter-hemispheric asymmetries included the cortical thickness of Rolandic regions and the volume of thalami. Fatigue symptoms increased together with the functional inter-hemispheric imbalance of sensorimotor homologous areas activities at rest and during movement, in absence of any appreciable parenchymal asymmetries. This finding supports the development of compensative interventions that may revert these neuronal activity imbalances to relieve fatigue in MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fatigue is a bothersome symptom shared by a variety of conditions, including Multiple sclerosis (MS), in which up to 90 % of patients may complain of it even early in the disease [1]. It affects social relationships and daily cognitive and physical activities of MS sufferers [2] who report fatigue as exhaustion, lacking energy, increased somnolence or worsening of MS symptoms, with augmented weakness exacerbated by activity and heat [3].
Fatigue may be secondary to MS-related complications (trigeminal neuralgia, spasms, psychiatric comorbidities, etc.), musculoskeletal involvement (pain, posture, gait anomalies, etc.), sleep and drug-related issues [4]. Several findings confirm the existence of peripheral nervous system components of fatigue in MS [5]. However, there are clear indications that a main role is played by dysfunctional central mechanisms [6–9], with the sensorimotor system playing a principal role [6, 8–15].
Rather than on a whole-brain basis, primary MS-fatigue-related alterations emerged from structural studies measuring either the lesion volume or non-conventional metrics derived from magnetic resonance imaging (MRI) in specific brain regions [16, 17]. Indeed, pointing on brain regional specificity, a higher lesion load in fatigued patients has been found in the internal capsule, the periventricular trigone [6], the posterior parietal cortex [18], the right parieto-temporal and left frontal lobes [19].
From a neurophysiological perspective, potential mechanisms of this phenomenon reside in the sensorimotor system functional alterations at cortical [6, 10–13] and subcortical levels [8, 14, 15]. We recently observed that altered functional communication within the sensorimotor system emerges in MS-fatigued patients before that any structural damage in the communicating nodes is appreciated [9].
A recent achievement is the dynamic interplay between homologous cortical areas as a critical element for a proper functioning of the motor system either during task execution or even at rest (in which the behavioral performance associates to the functional connectivity across the nodes of the devoted network) [20–22]. Thus, here we focused on the inter-hemispheric balance between homologous primary sensorimotor cortices. The primary nodes of the sensorimotor network may be early affected by demyelination and/or axonal loss, reflecting functional disconnections even over long distances. Dynamic indices were derived at rest and during movement from electroencephalographic (EEG) recordings.
To assess the potential influence of structural (parenchymal) inter-hemispheric sensorimotor imbalances on MS fatigue, we also investigated the asymmetry indices of thalamic volumes and cortical thickness of rolandic regions, which represent key nodes of this network.
Data were collected from relapsing remitting (RR) MS patients with low-range disability to minimize the effects of the disease upon fatigue.
Methods
Participants
The work was approved by the Ethical Committee of the Fatebenefratelli Hospital and was performed in accordance with the ethical standards noted in the 1964 Declaration of Helsinki. All subjects signed informed consents prior to their inclusion in the study.
According to Lublin’s categories [23], twenty-seven MS patients (13 females; age range 22–47 years; mean = 37 years) were recruited at the MS center of ‘S. Giovanni Calibita’ Fatebenefratelli Hospital (Rome, Italy). Eight healthy subjects (7 females, age range 25–48 years; mean = 37) were enrolled as controls (C).
A detailed clinical history inclusive of ongoing disease-modifying therapy (DMT), disease duration and annual relapse rate was collected. Beck Depression Inventory (BDI) and expanded disability status scale (EDSS) were scored at the time of neurological examination and used in exclusion criteria to eliminate concomitant origin of fatigue in depression (BDI ≥ 13) or excessive disease severity (EDSS > 2). Fatigue levels were assessed using the modified fatigue impact scale (mFIS) that identifies the physical, cognitive, and psychosocial components of fatigue. Inclusion criteria were as follows: absence of clinical relapse or radiological evidence of disease activity over the last 3 months; ability to rule out physical disability or depression as confounding factors; EDSS score ≤3; no drugs against depression. The exclusion criteria included: (a) assumption of symptomatic drugs affecting the fatigue; depression and/or anxiety within the past 3 months; (b) epilepsy or other central/peripheral nervous system comorbidities; (c) any systemic conditions that may cause fatigue (e.g., anemia or pregnancy). We gave care to include people with MS suffering by a wide range of fatigue symptoms. mFIS scores ranged between 5 and 57, and considering a threshold of 36, 12 MS patients suffered low fatigue and 15 high fatigue (Table 1).
Electrophysiological study and inter-hemispheric balance assessment
The functional connectivity was measured during movement through the spectral coherence (inter-hemispheric coherence index, IHCoh) [24] and at rest through the power inter-hemispheric symmetry index (IHSym_Rest) [25], already proven to be a sensitive measure of the functional balance between homologous areas [26, 27].
The digital signals were recorded on computer for off-line processing using a pre-cabled cap (mod. CUEE60 M, Sei EMG s.r.l., Cittadella, Italy) with 23 Ag/AgCl electrodes (the standard 19 channels of the 10–20 International system plus FC4, FC3, CP4, CP3), with sampling rate of 1024 Hz (band pass filter 0.48–256 Hz). In addition, electro-oculogram to check for eye blinking and electrocardiogram (ECG) were acquired as polygraphic traces. EEGs were recorded using a Micromed System Plus equipped with SAM32 headbox (Micromed S.p.A., Mogliano Veneto, Italy), with a mid-frontal reference and an occipital ground. All subjects sat comfortably on a reclining chair, with their arms supported, flexed at the elbow and with the forearm semi-pronated (Fig. 1). Following a block design paradigm, EEG signals were recorded in 24 consecutive blocks, in which 20s of muscular contraction (motor task) were alternated with 10 s of opened eyes rest, to avoid fatigue induced by the task. The motor task consisted in an isometric handgrip against resistance from a semi-compliant air-bulb, connected to a digital board hosting in-house developed electronics that recorded the exerted pressure while giving the subject a visual feedback (Interactive Pressure Sensor, InPresS, Fig. 1). The task was executed once with each hand, in random order between subjects. The EEG recordings lasted about 20 min for each of the two sides. The procedure has been detailed elsewhere [9]. Complete resting EEG data were also collected.
Electrophysiological exam and variable. Left the recording set up with the EEG-cap, surface EMG electrodes and visual feedback is shown on an exemplificative subject. Right from top visual feedback while performing the task, with periods of isometric contractions intermingled with non-contraction; one second windowed a signal of EMG from left to right opponens pollicis muscles (second and fourth rows, EMGOPr and EMGOPl) and with bipolar derivation selected as maximally coherent with contralateral EMG activity (third and fifth rows, EEGSM1l and EEGSM1r) during rest and during right and left isometric handgrips. In the successive rows in one representative patient (Pat_10), power spectral density function (PSD) in the [2–90] Hz frequency range for EEGSM1 and EEGSMr in resting periods and during movement are shown (ordinate scales are fixed across the conditions). It is clear the reactivity with power reduction during movement than rest. The inter-hemispheric coherence function between EEGSM1 and EEGSMr is presented in the last row (dimensionless numbers) considered during movement. Asymmetry in the inter-hemispheric coherence when moving the right and left hands, especially in the alpha range, is evident
Firstly, the EEG bipolar derivations maximally coherent with the contralateral muscular activity during contraction were selected for both left (\({\text{EEG}}_{{{\text{SM}}_{1} }}^{\text{L}}\), typically C3-F3 or C3-FC3) and right (\({\text{EEG}}_{{{\text{SM}}_{1} }}^{\text{R}}\), typically C4-F4 or C4-FC4) hemisphere.
At rest, the inter-hemispheric symmetry index was calculated as:
where f indicates the frequency bin and PSDL and PSDR are the power spectral densities of the \({\text{EEG}}_{{{\text{SM}}_{1} }}^{\text{L}}\) and \({\text{EEG}}_{{{\text{SM}}_{1} }}^{\text{R}}\) [25], estimated by the Welch procedure (2 s lasting non-overlapping Hanning windows, averaging almost 100 epochs). We selected this index since it was observed sensitive to physiological [26] and pathological [27] alteration in resting state. With respect to van Putten’s definition, we considered the ratio without the absolute value transformation. In this way, we maintained the information about the direction of the inter-hemispheric asymmetry in such a way that IHSym_Rest <1 corresponds to R > L and vice versa. To check for the activation level of the sensorimotor area in each hemisphere, we measured the PSD during movements and rest.
To evaluate the functional balance of homologous sensorimotor areas when engaged in motor control, we evaluated the symmetry of their functional connectivity (estimated via spectral coherence in alpha band) when moving the right or the left hand separately. We calculated the cortico-cortical coherence as:
where f is the frequency bin, PCD the power cross spectrum estimated accordingly to the PSD as defined above. Frequency bins were integrated in standard EEG bands: delta (1.5–4 Hz); theta (4.5–8 Hz); alpha (8–12 Hz); beta (12–33 Hz); gamma (33.5–90 Hz, excluding five frequency bins around 50 Hz); whole spectrum (1.5–90 Hz). Thereafter, we considered their asymmetry when moving each hand by
Since here R and L refer to the moved hand, we inverted the order with respect to inter-hemispheric symmetry index at rest (IHSymRest).
The analysis of EEG data was performed with Matlab 2010 (The Mathworks Inc, MA, USA).
Magnetic resonance imaging and derived metrics
Data acquisition
Imaging was performed with a 1.5 T scanner (Achieva, Philips Medical Systems, Best, The Netherlands), provided with a 33 mT/m gradient amplitude, online 2D/3D geometric distortion correction and a standard quadrature head coil. The acquisition protocol is detailed in [26] and consisted of a high-resolution volumetric sequence optimized for morphometric measurements together with routine 2D sequences for lesion characterization. The former was empirically adjusted to allow reliable segmentation of subcortical structures (T1-weighted Turbo Field Echo TR/TE/FA = 8.6 ms/4 ms/8º; 256 × 256 matrix, 160 sagittal contiguous slices, in-plane resolution 1 × 1 mm). The 2D sequences included Dual Turbo Spin Echo, Fluid Attenuated Inversion Recovery (FLAIR) and two T1-Spin Echo sequences before and after intravenous injection of the contrast agent gadolinium (0.2 mmol/kg).
Lesion characterization
Optimized segmentation and volume calculation for normalization are described in Tecchio [28]. Briefly, in the present study, the lesion load was estimated as the lesion relative fraction (LrF), defined as the total lesion volume of white matter (WM) hyperintensities upon T2/FLAIR weighted images, normalized for the overall WM volume. This part is reported in the present work only for completeness of the clinical picture since no association between fatigue and lesion load was found in a previous study (Table 1, [9]).
Thalamic volume and cortical thickness estimate
Automated labeling and quantification of thalamus, supratentorial volumes and cortical thickness of sensorimotor regions were performed using FreeSurfer 5.1 [29, 30] installed on a multiprocessor Apple workstation. This software provides a neuroanatomical label of up to 40 unique structures based on probabilistic information assigned to each voxel in the brain MRI volume automatically estimated from an atlas integrating a manually labeled training set [31]. We selected the G_postcentral, S_central, and G_precentral cortical regions of the left and right hemispheres. A nonlinear transform is initialized with the linear one, and the image is allowed to further deform to better match the atlas. Lastly, a Bayesian segmentation procedure is performed, and the maximum a posteriori estimate of the labeling is computed. This approach provides an anatomically precise rendering of regional volumes that results comparable to manual ROI delineation [32, 33], without the potential for rater bias [30].
The entire cortex was visually inspected prior to analysis. Subjects requiring manual correction underwent: (a) manual realignment to the MNI template; (b) setting intensity normalization control points where brain matter was erroneously skull stripped; (c) adjustment watershed parameters of the skull strip; (d) visual inspection and correction of the automatic subcortical segmentation; and e) accuracy of WM/gray matter (GM) segmentation, to avoid possible misclassifications mostly due to MS lesions. Intracranial volume (ICV) was calculated and used to correct the raw volumetric measures [34], to eliminate the scaling effect with general head size. In the present study, the normalized volumes of thalamus proper were calculated as followed: [raw volume/ICV] × 1000. GM/WM and pial surfaces were then identified and thickness was defined as the shortest distance between their two models [35].
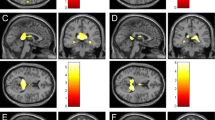
The asymmetry index between the left and right thalamus of each subject was calculated according to formula mentioned above for IHSym_Rest (IHSym_Thal). Accordingly, it was also calculated for the cortical thickness of the central sulcus regions (Fig. 2) among the overall measures provided by the software.
Statistics
Statistical analysis was performed using a Windows PC running SPSS v.19. First, the normal distribution of the variables was verified and logarithmic transformation applied where appropriate. PSD were not normally distributed, so we estimated their logarithmic transformation, which did not differ from a Gaussian (Shapiro–Wilk p > 0.300 consistently). A correlation analysis of inter-hemispheric balances at rest and during movement with fatigue symptoms guided all other steps. Whenever an association was found, the relative hemispheric values were evaluated and compared among the three groups (healthy and MS patients in dependence on the level of fatigue) proper ANOVA model. When comparing more than two groups Bonferroni’s post hoc test was adopted. In the case of inappropriateness of parametric tests, a non-parametric test (U Mann–Whitney and Kruskal–Wallis) was used. An uncorrected two-tailed alpha level of p < 0.05 was set as the significance threshold. P values between 0.05 and 0.10 were considered as trends.
Results
Functional inter-hemispheric balances of homologous sensorimotor cortices
Asymmetry of homologous primary sensorimotor power in resting state
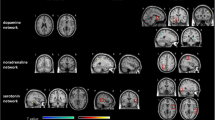
We found a clear positive correlation between fatigue scale and the inter-hemispheric power asymmetry of homologous primary sensorimotor cortices (Table 2; Fig. 3, left). In other words, people with MS suffering more for fatigue had higher left (dominant) than right (non-dominant) hemispheric primary sensorimotor activity power in the resting state. To better understand the origin of this relationship, we calculated the correlation with hemispheric power and found no associations in either side (Table 2). To have an estimate of the direction of the changes, we studied the values of these three variables in healthy people and in people with MS divided for suffering by low or high level of fatigue (see Table 3). Oneway ANOVA indicated that right hemisphere power differed among the three groups (Table 3), and post hoc comparisons evidenced that only high levels of fatigue were associated to lower power than both healthy controls (p = 0.030) and people with MS suffering low levels of fatigue (p = 0.048). Noteworthy, the trend of Groups effect for the inter-hemispheric power symmetry IHSymRest (Table 3, p = 0.052), corresponded to a trend of difference between people with MS suffering different levels of fatigue (p = 0.077). No differences were found between people with MS suffering low level of fatigue and healthy people (Sidak corrected p > 0.500 consistently).
MS fatigue and functional inter-hemispheric primary sensorimotor cortex balances. Scatter plot of mFIS with Left inter-hemispheric symmetry index related to the total power of primary sensorimotor areas at rest (IHSymRest). IHSymRest above 1 correspond to left higher than right powers (L > R) and viceversa for values below 1 (R > L). Right inter-hemispheric symmetry index related to functional connectivity between homologous primary sensorimotor areas during left and right handgrip (IHSymMovement). IHSymMovement above 1 correspond to inter-hemispheric coherence during right handgrip (left SM1 stronger recruitment) higher than during left handgrip and viceversa for values below 1. Linear fitting line in full corresponds to significant correlation
Asymmetry of inter-hemispheric connectivity between homologous primary sensorimotor areas during movement
Preliminarily, we evaluated whether any group effect was present in specific bands for the inter-hemispheric connectivity during movement. ANOVA included the within-subject factors Task-side (right handgrip, Left handgrip) and the between-subject factor Group (healthy controls, MS low fatigue, MS high fatigue). Given the strong dependence of IHCoh on the EEG frequency band (Band factor F(6, 120) = 34.325, p < 0.001), we carried out the analysis in each band and selectively in alpha band we found the Group factor [F(2, 20) = 5.474, p = 0.013]. All further investigation is on the inter-hemispheric coherence in alpha band.
The symmetry of the inter-hemispheric coherence during the left and right handgrips IHSymMovement was positively correlated with fatigue in people with MS, while no relation appeared with hemi-side values (Table 2; Fig. 3, right). This means that when controlling the movement, the left SM1 area establishes a higher inter-hemispheric coherence (connectivity, too strong as revealed in comparison with lower values in healthy controls, Table 3) with right SM1 to control right hand than to control the left hand (right hand movement > left). In other terms, when the left SM1 is more directly recruited (right hand movement), it connects the homologous contralateral area more than when the right SM1 is more directly recruited. To be noted, while no effect appeared in one-way ANOVA, comparing the two movements separately and differentiating the patients depending on the fatigue level (Table 3), the overall inter-hemispheric coherence in the group of people with MS was higher than in healthy controls. In fact, ANOVA including Task-side (Right handgrip, Left handgrip) as within-subjects factor and the 2-level between-subjects factor Group (Healthy Controls, People with MS), displayed the Group effect [F(1, 30) = 4.774, p = 0.037] corresponding to means across the two side tasks: 0.16 ± (SD) 0.08 in healthy control and 0.26 ± 0.13 in people with MS.
Structural inter-hemispheric balances of homologous sensorimotor regions
Regarding the thalamus volumes, no differences were observed among MS patients and controls either in terms of the asymmetry index (IHSym_thal, ANOVA 3-level between-subjects Group: p = 0.267, Table 4), or in terms of normalized thalamus volumes (ANOVA: left, p = 0.259; right, p = 0.866). No association was observed between such indicators and the mFIS scores. The same occurred for Rolandic areas cortical thickness.
Discussion
The main finding was that MS fatigue increased together with the functional imbalance between homologous sensorimotor areas’ activities both at rest and during movement. Our mildly disabled MS patients did not show any structural alteration of the primary sensorimotor network, in terms of thalamic volume or cortical thickness of rolandic regions. They also did not show alterations of primary sensorimotor cortices local neuronal activity. In particular, no alterations in either side associated with fatigue symptoms, which selectively associated with the reduction of their inter-side symmetry, both at rest and during movement. This finding extend to MS fatigue the evidence already got from stroke [20–22, 27, 36] and healthy people [26] that dynamic interplay between homologous cortical areas is critical for the brain networks effective functioning. This impaired pattern of the dynamic indices with little or no parenchymal changes indicates that the sensorimotor system derangement in MS fatigue is primarily functional, with a key role of homologous regions relationship. Our cohort included highly selected lowly disabled MS patients (median EDSS 1, range [0, 3]) enabling to rule out mechanism secondary to disease severity thus enhancing the ability to isolate mechanisms behind fatigue. This new findings strengthen the hypothesis that neuromodulations, i.e., techniques able to modify neuronal excitability of specific brain regions thus changing the interplay among brain areas, are promising treatment for MS fatigue [37]. Behavioral treatments can also modify the hemispheric balances [38, 39]. Thus, in addition to or integrating neuromodulation interventions, behavioral treatments should be tested against MS fatigue.
The intensification of fatigue symptoms is accompanied by an inter-hemispheric imbalance of activity at rest, in which left dominant SM1 areas generate higher power than the right non-dominant one. This could correspond to an impoverishment of the local organization of dominant hand representation. Indeed, in healthy controls we proved that the dominant hand representation (in the left hemisphere) has a lower power at rest than the non-dominant one [40]. In MS patients, an intra-cortical connectivity index specific of the left dominant hemisphere coding for sensorimotor dexterity [41] is distorted [28]. Moreover, the increment of power and inter-hemispheric imbalances show an increase in healthy people with aging in the same direction as in these MS patients, possibly as a sign of reduced functional organization in the region of the hand’s sensorimotor control [26].
In our study, MS fatigue increased with a rise of the inter-hemispheric coherence, possible expression of an increment of synchronization between neuron of homologous SM1. Studies in animals and in humans have demonstrated that cerebral regions, when engaged in shared tasks, start synchronizing the neuronal firings of involved networks [42–44]. This behavior can be hampered by several pathological conditions that shift synchronization levels toward lower values, such as in acute stroke patients [45] or even toward higher values, such as in depression, where an augmented functional connectivity within the anterior medial cortex [46] and an overall greater coherence in the resting state are found [47]. Alternatively and non-mutually exclusive, the increase of synchronization in our cohort can also result from an increment in the number of recruited neurons during movement, as a probable compensatory mechanism of MS fatigue directed to achieve the assigned task, which in turn induces the perception of fatigue. This is in line with previous fMRI studies [11, 13].
In conclusion, the present study strengthens the role of sensorimotor system involvement in MS fatigue, in particular indicating that the symptom increases when functional imbalance between homologous regions of the two hemispheres becomes stronger. Neuromodulation might offer a relief from MS fatigue sufferance, such as interventions able to modify the inter-hemispheric interplay of primary sensorimotor areas.
References
Riccitelli G, Rocca MA, Forn C, Colombo B, Comi G, Filippi M (2011) Voxelwise assessment of the regional distribution of damage in the brains of patients with multiple sclerosis and fatigue. AJNR Am J Neuroradiol 32:874–879
Pittion-Vouyovitch S, Debouverie M, Guillemin F, Vandenberghe N, Anxionnat R, Vespignani H (2006) Fatigue in multiple sclerosis is related to disability, depression and quality of life. J Neurol Sci 243:39–45
Vucic S, Burke D, Kiernan MC (2010) Fatigue in multiple sclerosis: mechanisms and management. Clin Neurophysiol 121:809–817
Asano M, Finlayson ML (2014) Meta-analysis of three different types of fatigue management interventions for people with multiple sclerosis: exercise, education, and medication. Mult Sclerosis Int 2014:798285
Iriarte J, de Castro P (1998) Correlation between symptom fatigue and muscular fatigue in multiple sclerosis. Eur J Neurol 5:579–585
Colombo B, Martinelli Boneschi F, Rossi P, Rovaris M, Maderna L, Filippi M, Comi G (2000) MRI and motor evoked potential findings in nondisabled multiple sclerosis patients with and without symptoms of fatigue. J Neurol 247:506–509
Sheean GL, Murray NM, Rothwell JC, Miller DH, Thompson AJ (1997) An electrophysiological study of the mechanism of fatigue in multiple sclerosis. Brain 120(Pt 2):299–315
Roelcke U, Kappos L, Lechner-Scott J, Brunnschweiler H, Huber S, Ammann W, Plohmann A, Dellas S, Maguire RP, Missimer J, Radu EW, Steck A, Leenders KL (1997) Reduced glucose metabolism in the frontal cortex and basal ganglia of multiple sclerosis patients with fatigue: a 18F-fluorodeoxyglucose positron emission tomography study. Neurology 48:1566–1571
Tomasevic L, Zito G, Pasqualetti P, Filippi M, Landi D, Ghazaryan A, Lupoi D, Porcaro C, Bagnato F, Rossini P, Tecchio F (2013) Cortico-muscular coherence as an index of fatigue in multiple sclerosis. Mult Scler 19:334–343
Leocani L, Colombo B, Magnani G, Martinelli-Boneschi F, Cursi M, Rossi P, Martinelli V, Comi G (2001) Fatigue in multiple sclerosis is associated with abnormal cortical activation to voluntary movement–EEG evidence. Neuroimage 13:1186–1192
Filippi M, Rocca MA, Colombo B, Falini A, Codella M, Scotti G, Comi G (2002) Functional magnetic resonance imaging correlates of fatigue in multiple sclerosis. Neuroimage 15:559–567
Liepert J, Mingers D, Heesen C, Baumer T, Weiller C (2005) Motor cortex excitability and fatigue in multiple sclerosis: a transcranial magnetic stimulation study. Mult Scler 11:316–321
Tartaglia MC, Narayanan S, Arnold DL (2008) Mental fatigue alters the pattern and increases the volume of cerebral activation required for a motor task in multiple sclerosis patients with fatigue. Eur J Neurol 15:413–419
Chaudhuri A, Behan PO (2000) Fatigue and basal ganglia. J Neurol Sci 179:34–42
Leocani L, Colombo B, Comi G (2008) Physiopathology of fatigue in multiple sclerosis. Neurol Sci 29(Suppl 2):S241–S243
Bakshi R, Miletich RS, Henschel K, Shaikh ZA, Janardhan V, Wasay M, Stengel LM, Ekes R, Kinkel PR (1999) Fatigue in multiple sclerosis: cross-sectional correlation with brain MRI findings in 71 patients. Neurology 53:1151–1153
Codella M, Rocca MA, Colombo B, Martinelli-Boneschi F, Comi G, Filippi M (2002) Cerebral grey matter pathology and fatigue in patients with multiple sclerosis: a preliminary study. J Neurol Sci 194:71–74
Pellicano C, Gallo A, Li X, Ikonomidou VN, Evangelou IE, Ohayon JM, Stern SK, Ehrmantraut M, Cantor F, McFarland HF, Bagnato F (2010) Relationship of cortical atrophy to fatigue in patients with multiple sclerosis. Arch Neurol 67:447–453
Sepulcre J, Masdeu JC, Goni J, Arrondo G, Velez de Mendizabal N, Bejarano B, Villoslada P (2009) Fatigue in multiple sclerosis is associated with the disruption of frontal and parietal pathways. Mult Scler 15:337–344
Carter AR, Astafiev SV, Lang CE, Connor LT, Rengachary J, Strube MJ, Pope DL, Shulman GL, Corbetta M (2010) Resting interhemispheric functional magnetic resonance imaging connectivity predicts performance after stroke. Ann Neurol 67:365–375
Deco G, Corbetta M (2011) The dynamical balance of the brain at rest. Neuroscientist 17:107–123
Dimyan MA, Cohen LG (2011) Neuroplasticity in the context of motor rehabilitation after stroke. Nat Rev Neurol 7:76–85
Lublin FD, Reingold SC (1996) Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis. Neurology 46:907–911
Thatcher RW, Krause PJ, Hrybyk M (1986) Cortico-cortical associations and EEG coherence: a two-compartmental model. Electroencephalogr Clin Neurophysiol 64:123–143
van Putten MJ (2007) The revised brain symmetry index. Clin Neurophysiol 118:2362–2367
Cottone C, Tomasevic L, Porcaro C, Filligoi G, Tecchio F (2013) Physiological aging impacts the hemispheric balances of resting state primary somatosensory activities. Brain Topogr 26:186–199
Graziadio S, Tomasevic L, Assenza G, Tecchio F, Eyre JA (2012) The myth of the ‘unaffected’ side after unilateral stroke: is reorganisation of the non-infarcted corticospinal system to re-establish balance the price for recovery? Exp Neurol 238:168–175
Tecchio F, Zito G, Zappasodi F, Dell’ Acqua ML, Landi D, Nardo D, Lupoi D, Rossini PM, Filippi MM (2008) Intra-cortical connectivity in multiple sclerosis: a neurophysiological approach. Brain 131:1783–1792
Fischl B, Dale AM (2000) Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci USA 97:11050–11055
Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, van der Kouwe A, Killiany R, Kennedy D, Klaveness S, Montillo A, Makris N, Rosen B, Dale AM (2002) Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33:341–355
Destrieux CHE, Dale AM, Fischl B, Sereno MI (1998) Variability of the human brain studied on the flattened cortical surface. Abstr Soc Neurosci 24:1164
Cerasa A, Messina D, Nicoletti G, Novellino F, Lanza P, Condino F, Arabia G, Salsone M, Quattrone A (2009) Cerebellar atrophy in essential tremor using an automated segmentation method. AJNR Am J Neuroradiol 30:1240–1243
Jovicich J, Czanner S, Han X, Salat D, van der Kouwe A, Quinn B, Pacheco J, Albert M, Killiany R, Blacker D, Maguire P, Rosas D, Makris N, Gollub R, Dale A, Dickerson BC, Fischl B (2009) MRI-derived measurements of human subcortical, ventricular and intracranial brain volumes: reliability effects of scan sessions, acquisition sequences, data analyses, scanner upgrade, scanner vendors and field strengths. Neuroimage 46:177–192
Buckner RL, Head D, Parker J, Fotenos AF, Marcus D, Morris JC, Snyder AZ (2004) A unified approach for morphometric and functional data analysis in young, old, and demented adults using automated atlas-based head size normalization: reliability and validation against manual measurement of total intracranial volume. Neuroimage 23:724–738
Fischl B, Sereno MI, Dale AM (1999) Cortical surface-based analysis. II: inflation, flattening, and a surface-based coordinate system. Neuroimage 9:195–207
Zappasodi F, Olejarczyk E, Marzetti L, Assenza G, Pizzella V, Tecchio F (2014) Fractal dimension of EEG activity senses neuronal impairment in acute stroke. PLoS One 9:e100199
Tecchio F, Cancelli A, Cottone C, Zito G, Pasqualetti P, Ghazaryan A, Rossini PM, Filippi MM (2014) Multiple sclerosis fatigue relief by bilateral somatosensory cortex neuromodulation. J Neurol 261:1552–1558
Avanzino L, Bassolino M, Pozzo T, Bove M (2011) Use-dependent hemispheric balance. J Neurosci 31:3423–3428
Avanzino L, Pelosin E, Abbruzzese G, Bassolino M, Pozzo T, Bove M (2013) Shaping Motor Cortex Plasticity Through Proprioception. Cereb Cortex
Tecchio F, Zappasodi F, Pasqualetti P, Tombini M, Salustri C, Oliviero A, Pizzella V, Vernieri F, Rossini PM (2005) Rhythmic brain activity at rest from rolandic areas in acute mono-hemispheric stroke: a magnetoencephalographic study. Neuroimage 28:72–83
Tecchio F, Graziadio S, Barbati G, Sigismondi R, Zappasodi F, Porcaro C, Valente G, Balsi M, Rossini PM (2007) Somatosensory dynamic gamma-band synchrony: a neural code of sensorimotor dexterity. Neuroimage 35:185–193
Gray CM, Konig P, Engel AK, Singer W (1989) Oscillatory responses in cat visual cortex exhibit inter-columnar synchronization which reflects global stimulus properties. Nature 338:334–337
Engel AK, Fries P, Singer W (2001) Dynamic predictions: oscillations and synchrony in top-down processing. Nat Rev Neurosci 2:704–716
Fellous JM, Houweling AR, Modi RH, Rao RP, Tiesinga PH, Sejnowski TJ (2001) Frequency dependence of spike timing reliability in cortical pyramidal cells and interneurons. J Neurophysiol 85:1782–1787
Assenza G, Zappasodi F, Pasqualetti P, Vernieri F, Tecchio F (2013) A contralesional EEG power increase mediated by interhemispheric disconnection provides negative prognosis in acute stroke. Restor Neurol Neurosci 31:177–188
Zhu X, Wang X, Xiao J, Liao J, Zhong M, Wang W, Yao S (2012) Evidence of a dissociation pattern in resting-state default mode network connectivity in first-episode, treatment-naive major depression patients. Biol Psychiatry 71:611–617
Leuchter AF, Cook IA, Hunter AM, Cai C, Horvath S (2012) Resting-state quantitative electroencephalography reveals increased neurophysiologic connectivity in depression. PLoS One 7:e32508
Acknowledgments
The Authors wish to thank Prof. Ada Maria Tata for her scientific collaboration and Matilde Ercolani who assisted with electrophysiological acquisition. We are sincerely grateful to all patients for the time and cooperation required to participate in the study. This work was supported by: 1) FISM—Fondazione Italiana Sclerosi Multipla – Cod.2011/R/32 [FaReMuSDiCDiT], 2) Ministry of Health Cod. GR-2008-1138642 [ProSIA], and 3) MIUR Prot. 2010SH7H3F ‘Functional connectivity and neuroplasticity in physiological and pathological aging [ConnAge]’.
Conflicts of interest
The authors have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
I. Cogliati Dezza and G. Zito equally contributed to this work.
Rights and permissions
About this article
Cite this article
Cogliati Dezza, I., Zito, G., Tomasevic, L. et al. Functional and structural balances of homologous sensorimotor regions in multiple sclerosis fatigue. J Neurol 262, 614–622 (2015). https://doi.org/10.1007/s00415-014-7590-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7590-6