Abstract
High-oligomeric and low-total-α-synuclein cerebrospinal fluid (CSF) levels have been found in Parkinson’s disease (PD), but with inconsistent or limited data, particularly on their clinical and structural correlates in earliest (premotor) or latest (dementia) PD stages. We determined CSF oligomeric- and total-α-synuclein in 77 subjects: 23 with idiopathic REM-sleep behaviour disorder (iRBD, a condition likely to include a remarkable proportion of subjects in the premotor stage of PD) and 41 with PD [21 non-demented (PDND) + 20 demented (PDD)], intended to reflect the premotor–motor–dementia PD continuum, along with 13 healthy controls. The study protocol also included the Unified PD Rating Scale motor-section (UPDRS-III), mini mental state examination (MMSE), neuropsychological cognitive testing, 3T brain MRI for cortical-thickness analyses, CSF τ and CSF Aβ. CSF oligomeric-α-synuclein was higher in PDND than iRBD and in PDD than iRBD and controls, and correlated with UPDRS-III, MMSE, semantic fluency and visuo-perceptive scores across the proposed premotor–motor–dementia PD continuum (iRBD + PDND + PDD). CSF total-α-synuclein positively correlated with age, CSF Aβ, and, particularly, CSF τ, tending towards lower levels in PD (but not iRBD) vs. controls only when controlling for CSF τ. Low CSF total-α-synuclein was associated with dysfunction in phonetic-fluency (a frontal-lobe function) in PD and with frontal cortical thinning in iRBD and PDND independently of CSF τ. Conversely, the associations of high (instead of low) CSF total-α-synuclein with posterior-cortical neuropsychological deficits in PD and with posterior cortical thinning in PDD were driven by high CSF τ. These findings suggest that CSF oligomeric- and total-α-synuclein have different clinical, neuropsychological and MRI correlates across the proposed premotor–motor–dementia PD continuum. CSF total-α-synuclein correlations with CSF τ and Aβ support the hypothesis of an interaction among these proteins in PD, with CSF τ probably influencing the presence of high (instead of low) CSF total-α-synuclein and its correlates mostly in the setting of PD-related dementia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The relevance of α-synuclein to intraneuronal Lewy-type inclusions and the close relationship of cerebrospinal fluid (CSF) with brain parenchyma make of α-synuclein determination in CSF a candidate biomarker of Parkinson’s disease (PD) [1, 2]. Detecting in vivo α-synuclein abnormalities would be significant for the study of the so-called premotor PD [3], a stage hypothetically more likely to respond to potential early interventions due to more restricted α-synuclein pathology [4]. A reliable α-synuclein biomarker might also be predictive of cognitive impairment, very frequent as PD progresses [5], and shown to correlate with Braak’s α-synuclein stages [6].
CSF total-α-synuclein levels in PD vs. controls have ranged in different studies from significant reductions [7–12] to similar levels [13–16]. Blood contamination of CSF has been pointed as a possible explanation for such discrepancies, but it remains unclear why among positive studies, some have needed controlling for CSF haemoglobin levels to find significant CSF total-α-synuclein reductions in PD [7, 11], and some have not [8–10]. Still, the intergroup overlap has been large even in positive studies having controlled for CSF haemoglobin levels [7, 11].
CSF levels of oligomeric-α-synuclein, believed to be a toxic α-synuclein fraction [17], have been found increased [8, 14] or non-significantly different [18] in PD vs. controls, with increased oligomeric/total-α-synuclein ratio having been reported in two of these studies [8, 18]. Allegedly, drop in CSF total-α-synuclein might reflect parenchymal sequestration of α-synuclein in Lewy-type lesions or an attempt of retaining the protein to maintain neuronal physiology, whereas increased clearance to CSF of soluble and toxic oligomers might account for raised CSF oligomeric-α-synuclein [1, 2].
Motor and cognitive impairment and cortical atrophy worsen with PD progression [19–21], but as yet there is no information on the clinical, neuropsychological and MRI correlates of these CSF α-synuclein markers across PD progression ranging from early premotor stages to advanced PD with dementia. We hypothesised that high oligomeric- and low total-α-synuclein CSF levels are associated with worsening motor and cognitive function and increasing cortical atrophy across the premotor–motor–dementia PD continuum. To this end we determined CSF oligomeric- and total-α-synuclein and their motor, neuropsychological, and quantitative MRI correlates in a cohort of subjects with idiopathic REM-sleep behaviour disorder (iRBD) and with PD without and with dementia, intended to represent the premotor–motor–dementia PD continuum.
Methods
Design, participants and clinical protocol
Cross-sectional study of a convenience cohort of 77 subjects from the research programs of the Movement Disorders Unit (controls and PD patients) and the Sleep Disorders Unit (iRBD subjects) of our institution, with these programs sharing the clinical and CSF protocol but differing in other aspects. Controls (n = 13) were individuals undergoing intradural anaesthesia for knee surgery who, as per thorough clinical history and examination, did not have any neurological or psychiatric condition. iRBD patients (n = 23) were prevalent cases (iRBD mean duration = 10.65 years) diagnosed by clinical history and video-polysomnography, in the absence of cognitive complaints or other neuro-psychiatric features as detailed elsewhere [22]. PD participants (n = 41) had a definite clinical diagnosis according to the UKPDSBB criteria [23]. Of them, 21 had no dementia (PDND) and 20 fulfilled the PD-dementia (PDD) diagnostic criteria [24]. Severe depression and MRI abnormalities other than mild white matter hyperintensities were exclusion criteria. Demographic and clinical information, including the motor part of the Unified PD Rating Scale (UPDRS-III) [25], Hoehn & Yahr staging [19], and mini mental state examination (MMSE) as a global cognitive indicator [26], were obtained for all participants. All, but one, PD patients have been reported elsewhere [27]. The study received approval from the Ethics Committee. All participants provided written informed consent after full explanation of all procedures.
CSF collection, pre-processing and storage
All participants underwent lumbar puncture in the L3–L4 space using a 22G needle after overnight fasting and before the morning anti-Parkinsonian medication in the case of PD patients. During extraction, CSF visually contaminated with blood was rejected. CSF was immediately centrifuged for 10 min at 4,000g and 4 °C, and subsequently stored at −80 °C in 500 μl polypropylene aliquots until analyses.
CSF analyses
CSF oligomeric-α-synuclein was determined using a modification of the ELISA technique used by others [8, 14], based on the principle of using the same antibody for coating and detection. Shortly, 96-well ELISA plates were coated overnight at 4 °C with anti-α-synuclein antibody (1 μg/ml; mouse 211-antibody, Santa Cruz) in 200 mM NaHCO3, pH 9.6. After 3 × 1 min washes in PBS–Tween and blocking for 2 h in blocking buffer (PBS–Tween–2 % BSA), 50 μl/well of CSF or standard solution were added and incubated for 2 h at 37 °C. Standard α-synuclein oligomers were prepared by incubation at 37 °C for 4 days of a 25 μM α-synuclein solution. After 3 washes in PBS–Tween, 50 μl/well of biotinylated anti-α-synuclein antibody (1:50) was added and incubated for 2 h at 37 °C. Biotinylation of 211-antibody was performed with a kit following the manufacturer’s instructions (EZ-Link Sulfo-NHS-LC-Biotinylation kit, #21435, Thermo Scientific). After 3 washes in PBS–Tween, wells were incubated for 1 h at 37 °C in ExtrAvidin–Alkaline Phosphatase (E2636, Sigma) 1:2,000, washed again 3 × 1 min and incubated for 30 min at 37 °C in p-nitrophenyl phosphate solution (N7653, Sigma). Absorbance was read immediately at 405 nm and results were expressed as absorbance values as in previous reports [8, 14].
CSF total-α-synuclein was determined using a commercial ELISA-kit (KHB0061, Invitrogen, Camarillo, CA, USA) with minor modifications. Briefly, 75 µl of each standard solution, CSF and blanks were dispensed in duplicate into ELISA plates. Plates were incubated for 3 h at 37 °C. Hu α-synuclein detection antibody solution (50 μl/well) was added (except for blank-wells). Plates were incubated overnight at 4 °C. Wells were washed 4 × 1 min with 200 µl of wash solution. 100 µl of goat anti-rabbit IgG HRP (1:100) was dispensed per well and incubated at room temperature for 30 min. Solution was decanted and, after four washes, plates were developed in the dark with 100 µl of TMB for 25 min at room temperature. Then, stop solution (100 µl of 0.6N H2SO4) was added and plates gently mixed. Absorbance was read at 450 nm and results were expressed in ng/ml.
All samples were run at once in two ELISA plates for each CSF α-synuclein form, with three samples of each group run in both plates to check for inter-plate variability. CSF levels of τ and Aβ [1–42] were determined with commercial ELISA kits (Innogenetics, Ghent, Belgium).
Neuropsychological assessment
iRBD and PD patients underwent neuropsychological assessment within 8 weeks of lumbar puncture. Pre-morbid level was established with years of education and the WAIS-III vocabulary subtest. iRBD patients underwent the Buschke memory test, WAIS-III similarities, FAS phonetic-fluency, and the 60-item Boston naming test (BNT-60). PD patients underwent the Rey auditory verbal learning test (RAVLT), phonetic fluency, the working-memory index (WMI) and the 15-item BNT (BNT-15). The iRBD and PD neuropsychological protocols shared semantic fluency and the visual object space (VOSP) object and space variables. PD patients were examined in “on” condition. All these tests were administered according to conventional procedures [28], with abnormal scores being defined as performance >1.5 SD below normative data or scale score ≤6 [29–32]. CSF comparisons dichotomising neuropsychological tests performance as normal vs. abnormal were carried out in PDND + PDD, but not in iRBD + PDND + PDD (due to protocol differences), neither in each group separately (due to small figures of iRBD and PDND subjects with impaired tests and to the fact that, as expected, most of PDD participants were impaired in most tests). CSF-neuropsychological correlations were carried out in each group separately and in PDND + PDD, but also in iRBD + PDND + PDD in the case of semantic fluency and VOSP variables.
MRI acquisition
iRBD and PD patients underwent 3T brain MRI in the same MRI machine (MAGNETOM Trio scanner, Siemens, Germany) without sedation and within 8 weeks of lumbar puncture. The scanning protocol for iRBD patients included high-resolution 3-dimensional T1-weighted images acquired in the sagittal plane (TR = 2,300 ms, TE = 2.98 ms, TI 900 ms, 240 slices, FOV = 256 mm; matrix size = 256 × 256; 1 mm isotropic voxel). In PD patients the MRI protocol included high-resolution 3-dimensional T1-weighted images in the coronal plane (TR = 2,300 ms, TE = 3.01 ms, TI 900 ms, 160 slices, FOV = 240 mm; matrix size = 240 × 240 × 192, 1 mm voxel).
Cortical-thickness (CTh) analyses
Cortical thickness was assessed using the automated FreeSurfer stream (version 5.3; http://surfer.nmr.harvard.edu) by means of removal of non-brain data, intensity normalisation, grey-matter/white matter boundary tessellation, automated-topology correction and accurate surface deformation to identify tissue borders [33, 34]. CTh was calculated as the distance between the white and grey-matter surfaces at each vertex of the reconstructed cortical mantle. Each subject’s results were visually inspected to ensure registration accuracy, skull stripping, segmentation, and cortical-surface reconstruction. Accordingly, MRI was suitable for CTh analyses in 19 iRBD, 16 PDND and 12 PDD patients. Due to different MRI acquisitions, CSF-CTh correlations were run separately in iRBD, PDND and PDD. Briefly, the CSF-CTh correlation was assessed with a vertex-by-vertex general linear model including potentially modifying covariates. Maps were smoothed using a circularly symmetric Gaussian kernel across the surface with a full-width-at-half-maximum of 15 mm. The software Qdec was used and default abs option allowed testing positive and negative correlations. Initial vertex-wise threshold was set at p = 0.05 (1.3) to find clusters, and Monte Carlo simulation (supported by Qdec software) with 10,000 repeats was tested to avoid false positives (clusters by chance due to multiple comparisons), with p ≤ 0.05.
Statistical analyses
Qualitative variables are presented as frequencies/percentages and quantitative ones as medians/interquartile ranges (quantitative variables), and were analysed with PASW 18.0 (IBM, New York, USA). Qualitative variables were compared with Chi-square or Fisher’s exact tests and quantitative ones with Kruskal–Wallis or Mann–Whitney’s U tests. Binary logistic regressions, where appropriate, resulted in odds ratios + 95 % confidence intervals [OR (95 % CIs)], reflecting the risk reduction or increase for each unit increase of the tested variable. Correlations were tested with Spearman’s rho in each group separately and, where applicable, in the entire cohort, in the purported premotor–motor–dementia continuum (iRBD + PDND + PDD), and in all PD (PDND + PDD) patients (see above). All statistical tests were two sided, with p threshold set at ≤0.05. No adjusts for multiplicity were applied (except for CTh analyses) due to the exploratory study design [35].
Results
Demographic, clinical and neuropsychological data
There were no significant differences in demographic and clinical variables among groups other than the expected worse UPDRS-III in PD and MMSE scores in PDD (Table 1). Formal neuropsychological comparisons were precluded by the intergroup protocol differences, but considering data as descriptive, overall cognitive performance worsened from iRBD to PDND and then PDD (Table 2).
CSF biomarkers findings
For both CSF total- and oligomeric-α-synuclein ELISAs, the R2 of the standard curves were >0.99, and the inter-plate variability was <10 %.
CSF oligomeric-αSYN significantly differed across groups (p = 0.003), due to significantly higher levels in PDD patients vs. controls (p = 0.043) and vs. iRBD patients (p = 0.001), and higher levels in PDND vs. iRBD patients (p = 0.043) (Table 1; Fig. 1a). CSF oligomeric-α-synuclein showed a modest significant positive correlation with CSF τ in the entire cohort (Suppl. Table 1).
Box plots of CSF oligomeric-α-synuclein (a) and CSF total-α-synuclein (b) in controls, iRBD, PDND, PDD. In panel a, solid line refers to Kruskall-Wallis test among all 4 groups, dotted line to Mann–Whitney’s U test between PDD and controls, the fine-dashed line to Mann–Whitney’s U test between PDD and iRBD and the thick-dashed line to Mann–Whitney’s U test between PDND and iRBD (asterisk denotes statistical significance)
CSF total-α-synuclein did not significantly differ among groups (Table 1; Fig. 1b), but strongly and consistently correlated with CSF τ (ρ >0.7 in all groups separately, in PDND + PDD, in iRBD + PDND + PDD and in the entire cohort; Fig. 2a; Suppl. Table 1), as well as with CSF Aβ, especially in PDND + PDD and in PDND patients separately (ρ = 0.467 and 0.719, respectively; Fig. 2b; Suppl. Table 1). In view of the strong total-α-synuclein/τ correlation, cases were stratified for varying CSF τ levels, with exclusion of subjects with CSF τ > 250 pg/ml (chosen after the CSF τ cohort median) resulting in a trend to more PD cases than controls with CSF total-α-synuclein below its median value [1 of 6 controls (17 %) vs. 11 of 17 PD patients (65 %); p = 0.059; Suppl. Figure 1]. Such a trend was not seen in iRBD (not shown).
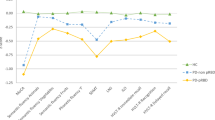
Scatter plots of significant clinical, CSF or neuropsychological correlations of CSF total-α-synuclein (a–c) and CSF oligomeric-α-synuclein (d–f): a significant positive correlation between CSF total-α-synuclein and CSF τ levels in the entire cohort; b significant positive correlation between CSF total-α-synuclein and CSF Aβ levels in all PD (PDND + PDD) patients; c significant positive correlation between CSF total-α-synuclein levels and age at lumbar puncture in the entire cohort; d significant positive correlation between CSF oligomeric-α-synuclein levels and UPDRS-III scores in the entire cohort; e significant negative correlation between CSF oligomeric-α-synuclein levels and MMSE scores in the entire cohort; f significant negative correlation between CSF oligomeric-α-synuclein levels and VOSP-S3 scores in iRBD + PDND + PDD patients
CSF total- and oligomeric-α-synuclein did not significantly correlate to each other in any data-sets, and there were not significant differences in the total-oligomeric ratio (data not shown).
CSF τ levels were similarly low in controls, iRBD, and PDND and significantly higher in PDD, whereas CSF Aβ decreased from controls, iRBD, and PDND to PDD (Table 1).
Correlates of CSF oligomeric α-synuclein
CSF oligomeric-α-synuclein positively correlated with UPDRS-III and negatively with MMSE in the entire cohort and in iRBD + PDND + PDD, in a way that the worse the motor and cognitive scores the higher the CSF oligomeric α-synuclein levels (Fig. 2d, e; Suppl. Table 1). CSF oligomeric-α-synuclein did not significantly differ between PDND + PDD patients with normal vs. impaired neuropsychological tests (Table 3), but showed significant negative correlations with semantic fluency and VOSP-O2, S1, S3 and S4 sub-scores in the iRBD + PDND + PDD continuum, and with VOSP-O1 and S3 sub-scores in PDND + PDD (Table 4; Fig. 2f). CSF oligomeric-α-synuclein did not correlate with any CTh measures (data not shown).
Correlates of CSF total α-synuclein
CSF total-α-synuclein positively correlated with age (Fig. 2c; Suppl. Table 1) in the entire cohort, in controls, and, especially, in PDD patients (ρ = 0.62; p = 0.004). CSF total-α-synuclein was lower in PDND + PDD patients with impaired vs. normal phonetic fluency (p = 0.026), but higher in those with impaired vs. normal RAVLT-recognition and BNT-15 (p = 0.030 and p = 0.049, respectively) (Table 3). However, only the association of low CSF total-α-synuclein with impaired phonetic fluency remained significant when including both CSF total-α-synuclein and CSF τ as covariates in a binary logistic regression with these tests as outcome, while in contrast RAVLT-recognition and BNT-15 were actually associated with high CSF τ (Table 3). CSF total-α-synuclein positively correlated with phonetic fluency and VOSP-O4 scores in PDND patients (Table 4).
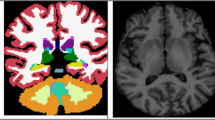
CSF total-α-synuclein co-varied for age and for both age and CSF τ showed significant positive correlations with CTh (the lower the CSF total-α-synuclein, the thinner the cortex) mainly of frontal structures in both iRBD and, with greater significance, PDND subjects (Table 5; Fig. 3, top–middle). In PDD patients, CSF total-α-synuclein co-varied for age showed negative correlations with CTh (the higher the CSF total-α-synuclein, the thinner the cortex) mainly of a large right parahippocampal cluster expanding to the isthmus and the precuneus. These correlations did not remain significant when co-varying for both age and CSF τ (Table 5; Fig. 3, bottom), with CSF τ levels negatively correlating with CTh from similar areas (Suppl. Table 2; Suppl. Figure 2).
Significant positive correlations between CSF total-α-synuclein levels and CTh in iRBD (upper panel) and PDND (middle panel) co-varied for age only (left) or for age and CSF τ (right), as well as significant negative correlations between CSF total-α-synuclein levels and CTh in PDD patients only when co-varying for age (bottom left), not resisting co-variation for both age and CSF τ (bottom right). Results were obtained using Monte Carlo simulation with 10,000 iterations applied to CTh maps to provide cluster-wise correction for multiple comparisons (p threshold <0.05; 1.3)
Discussion
In this cross-sectional study of a cohort intended to represent the premotor–motor–dementia PD continuum, we have found higher levels of CSF oligomeric-α-synuclein in PD mostly in the setting of dementia, albeit without differences in putative premotor (iRBD) cases, and a trend to low CSF total-α-synuclein in PD (but again not iRBD) when controlling for high CSF τ. We have identified clinical, neuropsychological and/or MRI correlates for the studied CSF α-synuclein markers across the premotor–motor–dementia categories. CSF total-α-synuclein correlations with CSF Aβ and CSF τ favour the shared relevance of these proteins in PD, with the correlation with CSF τ potentially accounting for high (instead of low) CSF total-α-synuclein (and its neuropsychological and MRI correlates) in PD patients with cognitive impairment.
The finding of increased CSF oligomeric-α-synuclein in PD and mostly PDD is in keeping with previous reports [8, 14, 36]. Lack of differences in the oligomeric-total ratio in contrast to two previous reports [8, 18] might be due to lack of differences in CSF total-α-synuclein in our cohort. The large overlap among groups and the lack of association with iRBD cast doubt on CSF oligomeric-α-synuclein as a standalone diagnostic or premotor PD biomarker. Still, high CSF oligomeric-α-synuclein levels, besides being particularly associated with PDD, also showed modest yet significant correlations with motor and both global and specific (posterior-cortical) cognitive dysfunction across the premotor–motor-dementia continuum, in a way that the higher CSF oligomeric-α-synuclein, the greater UPDRS-III and lower MMSE, semantic fluency and several VOSP-variables scores. Notably, the latter neuropsychological functions with a posterior-cortical basis were predictors of PDD in a longitudinal population-based study [20]. Thus, CSF oligomeric-α-synuclein might be a biomarker of disease progression or severity. The lack of correlations in groups separately might be due to smaller size and predominance of normal scores in iRBD and impaired performance in PDD. The lack of significant CTh correlates of CSF oligomeric-α-synuclein might be due to stringently adjusted CTh analyses and the fact that these were limited to part of the participants and not carried out across the entire continuum after the use of different MRI protocols.
CSF total-α-synuclein has ranged in previous studies from non-significant [13–16] to modest lowering in PD vs. controls [7–12]. Even though the lack of differences in CSF total α-synuclein in our study including for the first time iRBD patients might suggest that CSF total α-synuclein is not a premotor or diagnostic PD biomarker, the presence of significant MRI correlates of this CSF marker even in iRBD patients supports further longitudinal research of the combined use of CSF total α-synuclein and quantitative MRI (CTh) as candidate biomarkers of progression of iRBD to PD. We acknowledge that we have not measured CSF haemoglobin, but the true impact of α-synuclein from red blood cells on CSF total-α-synuclein remains unclear as some studies have found CSF total-α-synuclein differences without adjusting for CSF haemoglobin [8–10]. Besides, the intergroup overlap has been large even in studies controlling for CSF haemoglobin [7, 11]. Our findings suggest an alternative potential confounding factor in CSF total-α-synuclein studies: CSF τ. The strong positive total-α-synuclein/τ correlation in PD besides being partly a result of low levels of both CSF markers in some cases [11], implies that both markers can also be increased in some PD patients (Fig. 2a). The mechanisms why CSF total-α-synuclein and CSF τ can be either reduced or increased in PD are unknown. Parenchymal sequestration and reduced clearance into CSF might account for their reduction. Conversely, increased leakage to CSF might underlie their increase. Notably, high levels of both CSF total-α-synuclein and CSF τ are being increasingly reported in Alzheimer’s disease (AD) [16, 37], and cortical τ neurofibrillary pathology is not rare in PDD and correlates with cortical Lewy pathology [38]. In the light of all this and of the trend to low CSF total-α-synuclein in PD when controlling for high CSF τ, it can be hypothesised that greater cortical pathology (including Alzheimer-type lesions in some instances) in the setting of advanced PD with cognitive impairment or dementia might result in increased leakage of intracellular proteins as α-synuclein and tau to CSF from neurons undergoing degeneration. The lack of a trend to low CSF total-α-synuclein in iRBD when controlling for high CSF τ might be due to more restricted α-synuclein pathology in premotor PD [4].
Besides correlating with CSF τ, CSF total-α-synuclein has also shown a significant correlation with CSF Aβ. These correlations could be an in vivo reflection of the close association between all three proteins shown by clinico-pathological studies [39]. Furthermore, Aβ can enhance fibrillisation of α-synuclein [40] and specific α-synuclein strains can induce τ aggregation [41], suggesting a synergism between these proteins. The significant correlation with CSF Aβ in contrast to the preliminary PPMI report in early PD patients [11] might be due to inclusion in our study of more advanced PD patients with dementia and clearly lowered CSF Aβ.
As for the correlates of CSF total-α-synuclein, it has shown modest (entire cohort) to moderate (PDD) positive correlation with age. Thus, caution will probably also be needed when interpreting CSF total-α-synuclein in elder and demented PD patients. In terms of neuropsychological associations, CSF total-α-synuclein was significantly lower in PD patients with impaired phonetic fluency, a typical attentional/frontosubcortical cognitive indicator, in keeping with its mostly frontal CTh correlates, not only in PDND, but also in iRBD. Such associations raise the question whether, despite the lack of cross-sectional significant differences, iRBD and PDND patients with low CSF total-α-synuclein and frontal cortical thinning are at risk of further progression within the PD continuum. Longitudinal studies should address this.
The unexpected neuropsychological and CTh correlates of high (instead of low) CSF total-α-synuclein might also be due to a potential modifying effect of high CSF τ, as these associations did not resist adjust for CSF τ, an AD biomarker. Interestingly these neuropsychological (recognition memory and naming) and MRI (parahippocampal and precuneus cortical thickness) correlates were also AD like. Both in our previous reports with almost the same PD participants and in the current one, high CSF τ has been associated with AD-type neuropsychological and quantitative MRI changes [27, 42]. As speculated above, more aggressive neurodegeneration and sometimes comorbid AD-type τ pathology in PD might contribute to cognitive impairment, greater atrophy, and increased (instead of decreased) CSF total-α-synuclein. It is noteworthy that high (not low) CSF total-α-synuclein has been recently associated with cognitive deterioration in PD using samples from the DATATOP cohort [43]. In this study the authors provided an alternative potential explanation of the presence of high (instead of low) CSF total-α-synuclein in patients with cognitive impairment, suggesting that it might reflect the inability of neurons undergoing more aggressive neurodegeneration of retaining the physiologically active α-synuclein protein intracellularly thus resulting in higher extracellular (i.e., CSF) concentration of this protein [43].
Both CSF α-synuclein markers did not significantly correlate to each other and their correlates have differed, suggesting that they might differently reflect functional and structural changes in the proposed PD continuum. Thus, while the neuropsychological and MRI correlates of both low and high CSF total-α-synuclein were noticeably congruent (mostly frontal in the case of low levels and posterior cortical in the case of high levels), the motor and cognitive correlates of CSF oligomeric-α-synuclein were not mirrored by any MRI correlations. Studies of larger cohorts shall better characterise CTh correlates of both CSF oligomeric- and total-α-synuclein.
This study has a number of limitations. The convenience cohort has the hurdle of differences in neuropsychological and MRI protocols that have precluded performing all correlations across all groups. However, it has enabled putting together a cohort that otherwise would not have been easily accessible. The non-availability of neuropsychological assessment and MRI in the small-sized control group does not allow for concluding that the observed correlations are disease specific and future studies shall definitely include larger control groups and ensure the availability of all biomarker studies in the majority of participants. A limitation of the neuropsychological protocols was the fact that these differed between iRBD and PD patients, along with the lack of tests specifically covering certain functions (i.e., problem-solving and set-shifting abilities), but still most tests used in the present study are part of the recommendations by the international Parkinson’s disease and movement disorders society to assess cognition in PD [44]. As stated above, the non-availability of MRI in part of the participants may have accounted for underpowered CTh analyses. This study is cross-sectional and longitudinal surveys combining CSF, MRI and other putative premotor biomarkers (smell testing, transcranial ultrasound, DAT SPECT) will be needed, particularly in the case of iRBD, as it can herald other synucleinopathies, albeit PD is its most frequent outcome [22]. In our cohort disease duration was not significantly longer in PDND vs. PDD groups when it might be expected to be longer in PDD. However, disease progression in terms of both dementia and spread of neuropathological damage to cortical areas does not always correlate with disease duration. Finally, our findings have to be taken with caution due to lack of adjust for CSF haemoglobin and technical differences with other studies. However, the CSF, clinical, neuropsychological and MRI associations in our cohort are plausible and partly in keeping with existing evidence [11, 14, 36, 43].
The present study has also important strengths, as being the first, to the best of our knowledge, assessing both oligomeric and total CSF α-synuclein forms in a cohort attempted to reflect the premotor–motor–dementia PD continuum. The multimodal approach, assessing the clinical, neuropsychological and MRI correlates of both CSF α-synuclein markers, not only in PDND, but also, for the first time, in iRBD and in PDD, is another strength.
In summary, the observed correlates of CSF oligomeric- and total-α-synuclein in a cohort ranging from putative premotor-PD to advanced PD-dementia suggest that these CSF measures might be progression or severity PD biomarkers, differently reflecting functional and/or structural changes across the premotor–motor–dementia PD continuum. Factors such as high CSF τ and increasing age were associated with high CSF total-α-synuclein, thus being potential confounders to consider in future research. The correlations of CSF total-α-synuclein not only with CSF τ but also CSF Aβ are in keeping with the suggestion of synergism between these proteins in PD [38–41]. It remains to be seen whether other CSF α-synuclein-related biomarkers as phosphorylated-α-synuclein [45], DJ-1 [7], glucocerebrosidase [18], or, in the future, molecular imaging of α-synuclein-containing lesions, will eventually overcome the limitations of CSF oligomeric- and total-α-synuclein as PD biomarkers.
References
Mollenhauer B (2014) Quantification of α-synuclein in cerebrospinal fluid: how ideal is this biomarker for Parkinson’s disease? Parkinsonism Relat Disord 20(Suppl 1):S76–S79
Magdalinou N, Lees AJ, Zetterberg H (2014) Cerebrospinal fluid biomarkers in parkinsonian conditions: an update and future directions. J Neurol Neurosurg Psychiatry 85:1065–1075
Tolosa E, Gaig C, Santamaría J, Compta Y (2009) Diagnosis and the premotor phase of Parkinson disease. Neurology 72:S12–S20
Braak H, Del Tredici K, Rüb U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Hely MA, Reid WG, Adena MA, Halliday GM, Morris JG (2008) The Sydney multicenter study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord 23:837–844
Braak H, Rüb U, Jansen Steur EN, Del Tredici K, de Vos RA (2005) Cognitive status correlates with neuropathologic stage in Parkinson disease. Neurology 64:1404–1410
Hong Z, Shi M, Chung KA, Quinn JF, Peskind ER, Galasko D, Jankovic J, Zabetian CP, Leverenz JB, Baird G, Montine TJ, Hancock AM, Hwang H, Pan C, Bradner J, Kang UJ, Jensen PH, Zhang J (2010) DJ-1 and alpha-synuclein in human cerebrospinal fluid as biomarkers of Parkinson’s disease. Brain 133:713–726
Tokuda T, Qureshi MM, Ardah MT, Varghese S, Shehab SA, Kasai T, Ishigami N, Tamaoka A, Nakagawa M, El-Agnaf OM (2010) Detection of elevated levels of α-synuclein oligomers in CSF from patients with Parkinson disease. Neurology 75:1766–1772
Mollenhauer B, Locascio JJ, Schulz-Schaeffer W, Sixel-Döring F, Trenkwalder C, Schlossmacher MG (2011) α-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with parkinsonism: a cohort study. Lancet Neurol 10:230–240
Parnetti L, Chiasserini D, Bellomo G, Giannandrea D, De Carlo C, Qureshi MM, Ardah MT, Varghese S, Bonanni L, Borroni B, Tambasco N, Eusebi P, Rossi A, Onofrj M, Padovani A, Calabresi P, El-Agnaf O (2011) Cerebrospinal fluid Tau/α-synuclein ratio in Parkinson’s disease and degenerative dementias. Mov Disord 26:1428–1435
Kang JH, Irwin DJ, Chen-Plotkin AS, Parkinson’s Progression Markers Initiative et al (2013) Association of cerebrospinal fluid β-amyloid 1-42, T-tau, P-tau181, and α-synuclein levels with clinical features of drug-naive patients with early Parkinson disease. JAMA Neurol 70:1277–1287
van Dijk KD, Bidinosti M, Weiss A, Raijmakers P, Berendse HW, van de Berg WD (2014) Reduced α-synuclein levels in cerebrospinal fluid in Parkinson’s disease are unrelated to clinical and imaging measures of disease severity. Eur J Neurol 21:388–394
Ohrfelt A, Grognet P, Andreasen N, Wallin A, Vanmechelen E, Blennow K, Zetterberg H (2009) Cerebrospinal fluid alpha-synuclein in neurodegenerative disorders-a marker of synapse loss? Neurosci Lett 450:332–335
Park MJ, Cheon SM, Bae HR, Kim SH, Kim JW (2011) Elevated levels of α-synuclein oligomer in the cerebrospinal fluid of drug-naïve patients with Parkinson’s disease. J Clin Neurol 7:215–222
Aerts MB, Esselink RA, Abdo WF, Bloem BR, Verbeek MM (2012) CSF α-synuclein does not differentiate between parkinsonian disorders. Neurobiol Aging 33:430.e1–430.e3
Slaets S, Vanmechelen E, Le Bastard N, Decraemer H, Vandijck M, Martin JJ, De Deyn PP, Engelborghs S (2014) Increased CSF α-synuclein levels in Alzheimer’s disease: correlation with tau levels. Alzheimers Dement. doi:10.1016/j.jalz.2013.10.004
Winner B, Jappelli R, Maji SK, Desplats PA, Boyer L, Aigner S, Hetzer C, Loher T, Vilar M, Campioni S, Tzitzilonis C, Soragni A, Jessberger S, Mira H, Consiglio A, Pham E, Masliah E, Gage FH, Riek R (2011) In vivo demonstration that alpha-synuclein oligomers are toxic. Proc Natl Acad Sci USA 108:4194–4199
Parnetti L, Chiasserini D, Persichetti E, Eusebi P, Varghese S, Qureshi MM, Dardis A, Deganuto M, De Carlo C, Castrioto A, Balducci C, Paciotti S, Tambasco N, Bembi B, Bonanni L, Onofrj M, Rossi A, Beccari T, El-Agnaf O, Calabresi P (2014) Cerebrospinal fluid lysosomal enzymes and α-synuclein in Parkinson’s disease. Mov Disord 29(8):1019–1027
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Williams-Gray CH, Foltynie T, Brayne CEG, Brayne CE, Robbins TW, Barker RA (2007) Evolution of cognitive dysfunction in an incident Parkinson’s disease cohort. Brain 130:1787–1798
Weintraub D, Doshi J, Koka D, Davatzikos C, Siderowf AD, Duda JE, Wolk DA, Moberg PJ, Xie SX, Clark CM (2011) Neurodegeneration across stages of cognitive decline in Parkinson disease. Arch Neurol 68:1562–1568
Iranzo A, Tolosa E, Gelpi E, Molinuevo JL, Valldeoriola F, Serradell M, Sanchez-Valle R, Vilaseca I, Lomeña F, Vilas D, Lladó A, Gaig C, Santamaria J (2013) Neurodegenerative disease status and post-mortem pathology in idiopathic rapid-eye-movement sleep behaviour disorder: an observational cohort study. Lancet Neurol 12:443–453
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Emre M, Aarsland D, Brown R, Burn DJ, Duyckaerts C, Mizuno Y, Broe GA, Cummings J, Dickson DW, Gauthier S, Goldman J, Goetz C, Korczyn A, Lees A, Levy R, Litvan I, McKeith I, Olanow W, Poewe W, Quinn N, Sampaio C, Tolosa E, Dubois B (2007) Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord 22:1689–1707
Fahn S, Elton RL, Members of the UPDRS Development Committee Unified Parkinson’s disease rating scale (1987) Unified Parkinson’s disease rating scale. In: Fahn S, Marsden CD, Calne DB, Lieberman A (eds) Recent developments in Parkinson’s disease. McMillan Health Care Information, Florham Park, p 153
Folstein MF, Folstein SE, McHugh PR (1975) ‘‘Mini-Mental state.’’ A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Compta Y, Martí MJ, Ibarretxe-Bilbao N, Junqué C, Valldeoriola F, Muñoz E, Ezquerra M, Ríos J, Tolosa E (2009) Cerebrospinal tau, phospho-tau, and beta-amyloid and neuropsychological functions in Parkinson’s disease. Mov Disord 24:2203–2210
Lezak MD, Howieson DB, Loring DW (2004) Neuropsychological assessment, 4th edn. Oxford University Press Inc., New York
Peña-Casanova J, Gramunt-Fombuena N, Quiñones-Ubeda S, Sánchez-Benavides G, Aguilar M, Badenes D, Molinuevo JL, Robles A, Barquero, Payno M, Antúnez C, Martínez-Parra C, Frank-García A, Fernández M, Alfonso V, Sol JM, Blesa R, NEURONORMA Study Team (2009) Spanish multicenter normative studies (NEURONORMA project): norms for the Rey-Osterrieth complex figure (copy and memory), and free and cued selective reminding test. Arch Clin Neuropsychol 24:371–393
Peña-Casanova J, Quiñones-Ubeda S, Gramunt-Fombuena N, Aguilar M, Casas L, Molinuevo JL, Robles A, Rodríguez D, Barquero, Antúnez C, Martínez-Parra C, Frank-García A, Fernández M, Molano A, Alfonso V, Sol JM, Blesa R, NEURONORMA Study Team (2009) Spanish multicenter normative studies (NEURONORMA Project): norms for boston naming test and token test. Arch Clin Neuropsychol 24:343–354
Peña-Casanova J, Quiñones-Ubeda S, Gramunt-Fombuena N, Quintana-Aparicio M, Aguilar M, Badenes D, Cerulla N, Molinuevo JL, Ruiz E, Robles A, Barquero, Antúnez C, Martínez-Parra C, Frank-García A, Fernández M, Alfonso V, Sol JM, Blesa R, NEURONORMA Study Team (2009) Spanish Multicenter normative Studies (NEURONORMA Project): Norms for verbal fluency tests. Arch Clin Neuropsychol 24:395–411
Peña-Casanova J, Quintana-Aparicio M, Quiñones-Ubeda S, Aguilar M, Molinuevo JL, Serradell M, Robles A, Barquero, Villanueva C, Antúnez C, Martínez-Parra C, Frank-García A, Aguilar MD, Fernández M, Alfonso V, Sol JM, Blesa R, NEURONORMA Study Team (2009) Spanish Multicenter normative Studies (NEURONORMA Project): norms for the visual object and space perception battery-abbreviated, and judgment of line orientation. Arch Clin Neuropsychol 24:355–370
Dale AM, Fischl B, Sereno MI (1999) Cortical surface-based analysis. I. segmentation and surface reconstruction. Neuroimage 9:179–194
Fischl B, Dale AM (2000) Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci USA 97:11050–11055
Perneger TV (1998) What’s wrong with Bonferroni adjustments. Br Med J 316:1236–1238
Hansson O, Hall S, Ohrfelt A, Zetterberg H, Blennow K, Minthon L, Nägga K, Londos E, Varghese S, Majbour NK, Al-Hayani A, El-Agnaf OM (2014) Levels of cerebrospinal fluid α-synuclein oligomers are increased in Parkinson’s disease with dementia and dementia with Lewy bodies compared to Alzheimer’s disease. Alzheimers Res Ther 6:25
Wennström M, Suroya Y, Hall S, Nilsson C, Minthon L, Boström F, Hansson O, Nielsen HM (2008) Low CSF levels of both α-synuclein and the α-synuclein cleaving enzyme neurosin in patients with synucleinopathy. PLoS ONE 8:e53250
Apaydin H, Ahlskog JE, Parisi JE, Boeve BF, Dickson DW (2002) Parkinson disease neuropathology: later-developing dementia and loss of the levodopa response. Arch Neurol 59:102–112
Compta Y, Parkkinen L, O’Sullivan SS, Vandrovcova J, Holton JL, Collins C, Lashley T, Kallis C, Williams DR, de Silva R, Lees AJ, Revesz T (2011) Lewy- and Alzheimer-type pathologies in Parkinson’s disease dementia: which is moreimportant? Brain 134:1493–1505
Masliah E, Rockenstein E, Veinbergs I, Sagara Y, Mallory M, Hashimoto M, Mucke L (2001) Beta-amyloid peptides enhance alpha-synuclein accumulation and neuronal deficits in a transgenic mouse model linking Alzheimer’s disease and Parkinson’s disease. Proc Natl Acad Sci USA 98:12245–12250
Guo JL, Covell DJ, Daniels JP, Iba M, Stieber A, Zhang B, Riddle DM, Kwong LK, Xu Y, Trojanowski JQ, Lee VM (2013) Distinct α-synuclein strains differentially promote tau inclusions in neurons. Cell 154:103–117
Compta Y, Ibarretxe-Bilbao N, Pereira JB, Junqué C, Bargalló N, Tolosa E, Valldeoriola F, Muñoz E, Camara A, Buongiorno M, Martí MJ (2012) Grey matter volume correlates of cerebrospinal markers of Alzheimer-pathology in Parkinson’s disease and related dementia. Parkinsonism Relat Disord 18:941–947
Stewart T, Liu C, Ginghina C, Cain KC, Auinger P, Cholerton B, Shi M, Zhang J, Parkinson Study Group DATATOP Investigators (2014) Cerebrospinal fluid α-synuclein predicts cognitive decline in Parkinson disease progression in the DATATOP cohort. Am J Pathol 184:966–975
Litvan I, Goldman JG, Tröster AI, Schmand BA, Weintraub D, Petersen RC, Mollenhauer B, Adler CH, Marder K, Williams-Gray CH, Aarsland D, Kulisevsky J, Rodriguez-Oroz MC, Burn DJ, Barker RA, Emre M (2012) Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: movement disorder society task force guidelines. Mov Disord 27:349–356
Wang Y, Shi M, Chung KA, Zabetian CP, Leverenz JB, Berg D, Srulijes K, Trojanowski JQ, Lee VM, Siderowf AD, Hurtig H, Litvan I, Schiess MC, Peskind ER, Masuda M, Hasegawa M, Lin X, Lin X, Pan C, Galasko D, Goldstein DS, Jensen PH, Yang H, Cain KC, Zhang J (2012) Phosphorylated α-synuclein in Parkinson’s disease. Sci Trasnl Med 4:121ra20
Acknowledgments
The authors are most grateful to all the study participants, and acknowledge the help of Dr. M. Salazar, Dr. F. Basora, Dr. G. Sánchez-Etayo (Anesthesiology Service), Dr. F. Macule (Knee Surgery Unit), Mrs. A Martín, Mr. C. Garrido, Mr. M. Fabregat and Mr. S. Sotes (MRI Unit technicians). This study was funded through “Premio de la Federación Española de Parkinson [FEP] 2011” (PI041833; P. I.: Y. Compta) and “Fundació La Marató de TV-3” (N-2006-TV060510; P. I.: M.J. Marti).
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standard
This study was approved by the Institution Ethics Committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their informed consent prior to their inclusion in the study. There are no details in this manuscript that might disclose the identity of the participants.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
415_2014_7560_MOESM1_ESM.jpg
Box plots of CSF total-α-synuclein in controls vs. PD (PDND + PDD) after excluding cases with CSFτ > 400 pg/mL [A], >300 pg/mL [B] and >250 pg/mL [C]. Mann–Whitney’s U test comparisons were non-significant (p > 0.05), but there was a trend towards more subjects with CSF total-α-synuclein below the median value of this CSF biomarker in PD vs. controls (Fisher’s exact test, p = 0.059) (JPEG 115 kb)
415_2014_7560_MOESM2_ESM.jpg
Significant negative correlations between CSF τ levels and cortical thickness (CTh) in the left pars opercularis, right middle frontal and middle temporal gyri, and the right cuneus, in PDD patients (co-varied for age). Results were obtained using Monte Carlo simulation with 10,000 iterations applied to CTh maps to provide cluster-wise correction for multiple comparisons (p threshold <0.05; 1.3) (JPEG 145 kb)
Rights and permissions
About this article
Cite this article
Compta, Y., Valente, T., Saura, J. et al. Correlates of cerebrospinal fluid levels of oligomeric- and total-α-synuclein in premotor, motor and dementia stages of Parkinson’s disease. J Neurol 262, 294–306 (2015). https://doi.org/10.1007/s00415-014-7560-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7560-z