Abstract
Primary and secondary progressive forms of multiple sclerosis (PPMS and SPMS) have different pathological characteristics. However, it is unknown whether neurodegenerative mechanisms are shared. We measured cerebrospinal fluid (CSF) levels of neurofilament (Nf) light and heavy isoforms and N-acetylaspartic acid (NAA) in 21 PP, 10 SPMS patients and 15 non-inflammatory neurological disease controls (NINDC). Biomarkers were related to Expanded Disability Status Scale (EDSS) and Multiple Sclerosis Severity Score (MSSS) over a long period of follow-up [median (interquartile range) 9 (5.5–12.5) years] in 19 PPMS and 4 SPMS patients, and to T2 lesion load, T1 lesion load, and brain parenchymal fraction at the time of lumbar puncture. Nf light was higher in PPMS (p < 0.005) and Nf heavy was increased in both SPMS and PPMS (p < 0.05 and p < 0.01) compared to NINDC, but were comparable between the two MS subtypes. Nf heavy was a predictor of the ongoing disability measured by MSSS (R 2 = 0.17, β = 0.413; p < 0.05). Conversely, Nf light was the only predictor of the EDSS annual increase (R 2 = 0.195, β = 0.441; p < 0.05). The frequency of abnormal biomarkers did not differ between the two MS progressive subtypes. Our data suggest that PP and SPMS likely share similar mechanisms of axonal damage. Moreover, Nf heavy can be a biomarker of ongoing axonal damage. Conversely, Nf light can be used as a prognostic marker for accumulating disability suggesting it as a good tool for possible treatment monitoring in the progressive MS forms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Axonal loss is the pathological substrate of progressive disability in both primary progressive (PP) and secondary progressive (SP) multiple sclerosis (MS) subtypes. Among these, the PPMS form has been associated with more extensive axonal loss in demyelinated plaques [1]. However, it is still a matter of debate whether these two phenotypes are the result of a shared pathological mechanism [1, 2]. Cerebrospinal fluid (CSF) N-acetyl aspartate (NAA) and neurofilaments (Nf) light and heavy subunit levels were identified as promising markers of axonal damage in relapse-onset MS patients [3], but studies comparing progressive subtypes or longitudinal studies evaluating the relation with clinical decline in these subtypes are lacking. Therefore, we aimed to investigate whether PPMS patients exhibit different levels of axonal damage biomarkers compared to SPMS patients. Moreover, we assessed the aforementioned biomarkers for the prediction potential of long-term disease progression.
Methods
Patients and controls were enrolled at the Cemcat (Barcelona) from 1994 to 2008. MS patients were classified as having PPMS (n = 21) or SPMS (n = 10) as published elsewhere [4], where transitional progressive MS patients were considered as SPMS. Disability was measured using the Expanded Disability Status Scale (EDSS) and Multiple Sclerosis Severity Score (MSSS); a complete clinical dataset was available for 29 patients (20 PPMS, 9 SPMS) out of 31.
Nineteen PPMS and four SPMS patients underwent clinical follow-up [median (interquartile range) duration of follow-up: 9 (5.5–12.5) years].
During the follow-up period, 5 patients out of 23 (3 PPMS, 2 SPMS) received disease-modifying therapy (3 patients had interferon-β1b, 1 patient had mitoxantrone and 1 patient had imurel/mitoxantrone). Three patients (1 PPMS and 2 SPMS) did not experience an increase in EDSS during the follow-up, whereas the remaining patients (18 PPMS and 2 SPMS) experienced an EDSS progression, considered as an increase of 0.5 points in EDSS relative to baseline. Collectively, PPMS patients had a greater annual EDSS increase compared to SPMS patients (see Supplementary Table e1, p < 0.05).
The control group was composed of non-inflammatory neurological disease controls (NINDC, n = 15), as detailed in Supplementary Table e1.
Baseline brain T2 lesion load (T2LL), brain T1 lesion load (T1LL), and brain parenchymal fraction (BPF) were assessed on a Magnetom Vision Plus 1.5 T superconductive magnet (Siemens, Erlangen, Germany) within 48 h after CSF collection in 13 patients (9 PPMS, 4 SPMS) and calculated as described elsewhere [4].
The study was approved by the institutional review board and was in agreement with the principles of Helsinki. Written informed consent was obtained from all participants.
Demographics, baseline clinical and radiological characteristics of MS patients and controls are summarized in supplementary Table e1.
CSF samples were collected in agreement with BioMS-eu consensus guidelines [5]. NAA was determined by stable isotope dilution gas chromatography–mass spectrometry method [3]. Nf light was determined with the Uman Diagnostics ELISA [6, 7]. Phosphorylated Nf heavy was measured by an in-house developed bead-based assay [8]. All samples were analyzed in one batch in Amsterdam, blinded for clinical data.
Group comparisons were performed using Kruskal–Wallis followed by Mann–Whitney U tests, with Bonferroni correction for multiple comparisons. Annual rate of EDSS change was calculated by dividing the difference in EDSS by the follow-up duration. Regression analysis with MSSS or EDSS as dependent variable and Nf heavy, Nf light and NAA as predictors was performed on square root-transformed biomarker levels to normalize the residuals. Since an exploratory analysis on the data showed the presence of few influencing outliers, the annual change in EDSS and the axonal damage biomarkers were converted to ranks with the value of 1 assigned to the lowest value, with increasing numbers while increasing the value of the variable. The new coded variables, which were not influenced by outliers, were used for regression analysis with annual change in EDSS as dependent variable and axonal damage biomarkers as predictors. Frequency distributions were examined using Fisher’s exact test. A p < 0.05 was considered significant.
Results
Axonal damage biomarkers in progressive MS patients and NINDC
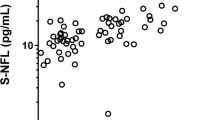
The values of biomarkers are shown in Fig. 1 (panels a–c) and numbers detailed in supplementary Table e1.
Values of biomarkers measured in the CSF of controls and MS patients. Filled horizontal lines indicate median values; dashed horizontal lines indicate the 90 % cut-off values for Nf light (panel a, 981 ng/L) and Nf heavy (panel b, 349 ng/L) and the 10 % cut-off value for NAA (panel c, 0.31 µmol/L), in the NINDC group. The open circles in the NINDC group indicate patients with epilepsy (Nf light = 366 ng/L, Nf heavy = 147 ng/L, NAA = 0.41 µmol/L), trigeminal neuropathy (Nf light = 574 ng/L, Nf heavy = 165 ng/L, NAA = 0.79 µmol/L), polyradiculopathy (Nf light = 812 ng/L, Nf heavy = 278 ng/L, NAA = 0.56 µmol/L) and hydrocephalus secondary to tumor (Nf light = 1018 ng/L, Nf heavy = 312 ng/L, NAA = 0.39 µmol/L)
The CSF levels of Nf light were higher in PPMS patients than NINDC (Fig. 1, panel a. Kruskal–Wallis H(2) = 10.78, p = 0.005; PPMS vs. NINDC, p = 0.003), whereas they were comparable between SPMS and NINDC as well as between the two progressive forms of MS. The levels of the phosphorylated Nf heavy protein were significantly higher in both SPMS and PPMS patients than in the NINDC group (Fig. 1, panel b. Kruskal–Wallis H(2) = 12.96, p = 0.002; SPMS vs. NINDC, p = 0.012; PPMS vs. NINDC, p = 0.003), while they were comparable between the two progressive MS forms (p = 1). We did not find differences in NAA values between the examined groups (Fig. 1, panel c. Kruskal–Wallis H(2) = 1.43, p = 0.489). No effect of age on the biomarker levels was observed (data not shown).
Relation of biomarkers with clinical disease progression
We assessed if Nf heavy, Nf light and NAA could predict the EDSS or MSSS scores at the time of lumbar puncture in a step-down multiple regression analysis.
The axonal damage biomarkers together or alone did not predict the ongoing disability measured by EDSS. On the contrary, they were significant predictors of the disability measured by MSSS score. In particular, the most powerful prediction model contained Nf heavy and NAA (Table 1, Model 1 step 2), whereas Nf light was not a significant predictor either in combination with Nf heavy and NAA or alone (Table 1, Model 4, p = 0.058). The statistically significant model (Table 1, Model 1 step 2; F(2, 26) = 5.359, p = 0.011) accounted for the 29 % of the variance of MSSS. The raw and standardized regression coefficients are reported in Table 1. MSSS was thus primarily predicted by increased levels of Nf heavy and to a lesser extent also by lower levels of NAA. Of note, Nf heavy remained a significant predictor of disability even after removal of NAA (Table 1, Model 2; F(1, 27) = 5.541, p = 0.026) accounting for 17 % of the variance of MSSS, whereas NAA alone failed to predict the disability (F(1, 27) = 2.051, p = 0.164).
Interestingly, the combination of the three biomarkers was able to predict the disability progression measured by the EDSS annual increase (Table 2, step 1; F(3, 19) = 3.220, p = 0.046), although the coefficients for Nf heavy and NAA did not reach the statistical significance. Conversely, the Nf light isoform was the only independent predictor of the disability progression (Table 2, step 3; F(1, 21) = 5.868, p = 0.025), accounting for almost 20 % of the total variance of EDSS annual increase, with a positive relation of the predictor with the outcome.
Combination of abnormal axonal damage biomarkers
Based on a 90 % cut-off value of Nf light and Nf heavy or 10 % cut-off of NAA in the NINDC group (Fig. 1 panels a–c, dashed horizontal lines), we defined in all subjects whether Nf light or Nf heavy was increased and whether the NAA levels were decreased. These values were considered as abnormal. As shown in Table 3, abnormal Nf light and Nf heavy levels were more frequent in MS patients than NINDC (Nf light, 38.7 vs. 6.7 %; Nf heavy, 38.7 vs. 6.7 %; p < 0.05 for both comparisons) as well as the combined neurofilaments (Nfs, 48.4 vs. 13.3 %; p < 0.05). Moreover, 25.8 % of the MS patients experienced simultaneous abnormal levels of Nf light and heavy isoforms, whereas none of the controls had it (p < 0.05). Although the combination of the three biomarkers had the tendency to classify a higher number of patients with abnormal values than controls, it did not reach the statistical significance (Table 3, NAA OR Nfs, 51.6 vs. 20.0 %, p = 0.058). Finally, we did not find any difference in the frequency of abnormal axonal damage biomarkers between PPMS and SPMS patients.
Discussion
Previous studies revealed that Nfs are good markers of the ongoing axonal damage, even at early stages of the disease [3, 9, 10]. However, a different role for the two isoforms in reflecting such a complex pathogenic process as MS pathology has been proposed. Thus, it has been postulated that Nf light might reflect early acute axonal damage since its levels are increased during relapses in relapsing–remitting (RR) MS patients [11], respond to anti-inflammatory treatments [12] and correlate with inflammatory markers [13]. On the other hand, Nf heavy has been proposed as a marker of chronic axonal damage [9], since its levels are increased in progressive forms of MS [9], with a possible prognostic value due to its correlation with disability/disease progression [9, 14]. Conversely, decreased CSF levels of NAA have been found in SPMS patients compared to RRMS and CIS patients [3, 15], with lower levels of NAA correlating with higher EDSS [3, 15], higher MRI lesion loads and lower brain volume [15], pointing it out as a potential marker of axonal damage as well [3]. Nevertheless, their role as prognostic markers in progressive MS was not known. The results of the present study showed higher levels of Nf light and Nf heavy in PPMS patients than NINDC, with no difference in the levels of NAA between MS patients and NINDC, which was in agreement with previous studies [3, 9, 16]. Moreover, only Nf heavy levels were found to be increased in SPMS patients compared to NINDC. This last result agrees only partly with previous studies. Previous studies also showed a difference in the CSF levels of Nf light in SPMS patients compared to controls [11, 16], whereas others did not find any difference [3].
One important result of this study is the lack of difference in Nf light and Nf heavy isoforms between the two progressive forms of MS, suggesting that the axonal damage is an equally important mechanism and probably has the same characteristics in both progressive subtypes. This is also confirmed by the finding of comparable frequency distributions of abnormal axonal damage biomarkers in the two progressive subtypes, while a higher frequency (higher than the 90 % cut-off for Nfs, and lower than the 10 % cut-off for NAA) was seen in the progressive MS patients than controls.
We observed moderate correlations between Nf heavy and MSSS at the time of lumbar puncture in agreement with previous reports [17], NAA and T1LL and T2LL (see supplementary results), along with the ability of Nf heavy alone or in combination with NAA to predict the ongoing disability, supporting the hypothesis that Nf heavy and NAA could be biomarkers for ongoing axonal damage [3, 9]. Of note, age was initially included in the regression models for the prediction of MSSS; however, the backward analysis removed the term as not significant (p = 0.468). In addition, we tried forcing the entry of age in the model but we observed only a change in the regression coefficient less than 9 % for both Nf heavy and NAA (B coefficient after inclusion of age: Nf heavy = 0.065; NAA = −2.025, compared with Model 1, step 2, Table 1). Collectively, our results strengthen the hypothesis of the usefulness of the combination of biomarkers in monitoring the ongoing axonal damage.
However, since median levels of NAA in progressive MS patients were comparable to controls, this marker could be associated to subclinical axonal degeneration or it might reflect aspecific neurodegeneration [18].
An important result was the relation of higher Nf light levels with higher annual increase in disability measured by EDSS, thus predicting disability development. As before, age was not found to be a significant influencing factor since it was excluded from the regression models by the backward analysis (t = −0.623, p = 0.542) and its forced inclusion did not cause an appreciable change in the regression coefficient (B coefficient after inclusion of age: Nf light = 0.411, compared with step 3, Table 2).
Although the regression data might be in contrast with the hypothesis that Nf light reflects acute axonal damage, a study by Salzer et al. [19] showed that Nf isoform could be a long-term prognostic marker in RRMS patients. Thus, the results from our study extend the potential of Nf light as a prognostic marker of axonal damage to progressive forms of MS. However, the number of patients included in our study is still such that replication is warranted.
This study was not without limitations. First, the just mentioned low number of patients with progressive MS over a long time span and the heterogeneous nature of the control groups [20], although obtaining large numbers of CSF samples from progressive MS patients and large control groups is hard as there is usually no diagnostic indication. Second, we failed to replicate the correlation between both Nf light and heavy isoforms with age in the control group, as found in previous studies [9, 16]. Although our control group had a comparable median age as in Kuhle’s studies [38 (27–46) vs. 39 (32–51)] [9, 16], we included fewer patients (NINDC n = 15 vs. controls n = 73) [9, 16]. Thus, the lack of correlation is likely due to the lower sample size, but can also be due to the type of neurological controls included [20]. Third, progressive MS patients were followed up for a variable time ranging from a minimum of 1 year to a maximum of 17 years [median (interquartile range) 9 (5.5–12.5) years] with a drop-out percentage of 26 %. However, the consistency of the results with previous reports [9, 16] and the clinical need for prognostic markers indicate that we can consider this study a good starting point to initiate longitudinal studies.
Fourth, we are aware that Nf isoforms and NAA are not ideal biomarkers, given the overlap between groups as seen in all studies on this subject [3, 16, 21], and the lack of specificity for MS. Indeed, they are not disease specific since they mark generalized axonal damage, a hallmark of several neurological diseases (e.g., Parkinson’s disease, amyotrophic lateral sclerosis, Alzheimer’s disease and traumatic brain injury) [6, 22]. Moreover, there are still controversial data on the power of Nf heavy as therapeutic biomarker over Nf light [12].
Finally, our study lacks of insight to causality since it is a correlative study, without any analyses of biomarkers at follow-up.
In conclusion, although with limitations our study strengthens the hypothesis that Nf heavy and NAA could be good markers for the ongoing axonal damage [3, 9, 15]. Moreover, it expands the concept of Nf light as a prognostic marker [19] to the progressive MS forms. Further studies in larger cohorts are needed to verify the actual significance of both Nf isoforms as markers for the prognosis of the progressive forms of MS.
References
Tallantyre EC, Bø L, Al-Rawashdeh O et al (2009) Greater loss of axons in primary progressive multiple sclerosis plaques compared to secondary progressive disease. Brain 132:1190–1199
Thompson AJ, Kermode AG, Wicks D et al (1991) Major differences in the dynamics of primary and secondary progressive multiple sclerosis. Ann Neurol 29:53–62
Teunissen CE, Iacobaeus E, Khademi M et al (2009) Combination of CSF N-acetylaspartate and neurofilaments in multiple sclerosis. Neurology 72:1322–1329
Montalban X, Sastre-Garriga J, Tintoré M et al (2009) A single-center, randomized, double-blind, placebo-controlled study of interferon beta-1b on primary progressive and transitional multiple sclerosis. Mult Scler 15:1195–1205
Teunissen CE, Petzold A, Bennett JL et al (2009) A consensus protocol for the standardization of cerebrospinal fluid collection and biobanking. Neurology 73:1914–1922
Norgren N, Rosengren L, Stigbrand T (2003) Elevated neurofilament levels in neurological diseases. Brain Res 987:25–31
Petzold A, Altintas A, Andreoni L et al (2010) Neurofilament ELISA validation. J Immunol Methods 352:23–31
Koel-Simmelink MJA, Vennegoor A, Killestein J et al (2014) The impact of pre-analytical variables on the stability of neurofilament proteins in CSF, determined by a novel validated SinglePlex Luminex assay and ELISA. J Immunol Methods 402:43–49
Kuhle J, Leppert D, Petzold A et al (2011) Neurofilament heavy chain in CSF correlates with relapses and disability in multiple sclerosis. Neurology 76:1206–1213
Khalil M, Enzinger C, Langkammer C et al (2013) CSF neurofilament and N-acetylaspartate related brain changes in clinically isolated syndrome. Mult Scler 19:436–442
Norgren N, Sundström P, Svenningsson A et al (2004) Neurofilament and glial fibrillary acidic protein in multiple sclerosis. Neurology 63:1586–1590
Kuhle J, Malmeström C, Axelsson M et al (2013) Neurofilament light and heavy subunits compared as therapeutic biomarkers in multiple sclerosis. Acta Neurol Scand 128:e33–e36
Romme Christensen J, Börnsen L, Khademi M et al (2013) CSF inflammation and axonal damage are increased and correlate in progressive multiple sclerosis. Mult Scler 19:877–884
Petzold A, Eikelenboom MJ, Keir G et al (2005) Axonal damage accumulates in the progressive phase of multiple sclerosis: three year follow up study. J Neurol Neurosurg Psychiatry 76:206–211
Jasperse B, Jakobs C, Eikelenboom MJ et al (2007) N-acetylaspartic acid in cerebrospinal fluid of multiple sclerosis patients determined by gas-chromatography-mass spectrometry. J Neurol 254:631–637
Kuhle J, Plattner K, Bestwick JP et al (2013) A comparative study of CSF neurofilament light and heavy chain protein in MS. Mult Scler 19:1597–1603
Petzold A, Eikelenboom MI, Keir G et al (2006) The new global multiple sclerosis severity score (MSSS) correlates with axonal but not glial biomarkers. Mult Scler 12:325–328
Llufriu S, Kornak J, Ratiney H et al (2014) Magnetic resonance spectroscopy markers of disease progression in multiple sclerosis. JAMA Neurol 71:840–847
Salzer J, Svenningsson A, Sundström P (2010) Neurofilament light as a prognostic marker in multiple sclerosis. Mult Scler 16:287–292
Teunissen C, Menge T, Altintas A et al (2013) Consensus definitions and application guidelines for control groups in cerebrospinal fluid biomarker studies in multiple sclerosis. Mult Scler 19:1802–1809
Eikelenboom MJ, Petzold A, Lazeron RHC et al (2003) Multiple sclerosis: neurofilament light chain antibodies are correlated to cerebral atrophy. Neurology 60:219–223
Ghonemi MO, Rabah AA, Saber HM, Radwan W (2013) Role of Phosphorylated Neurofilament H as a diagnostic and prognostic marker in traumatic brain injury. Egypt J Crit Care Med 1:139–144
Acknowledgments
This study was performed in the context of the BioMS-eu network (http://www.bioms.eu).
Conflicts of interest
The authors declare no financial or other conflicts of interest. In addition, Dr. Korth has a patent EPA 05715297.7-2403 issued. Dr. Teunissen provided consultation for Fujirebio/Innogenetics, and for Roche International Advisory Board; received a grant from Grant of National Science Foundation for joint Programming project BIOMARKAPD, outside the submitted work. In addition, Dr. Teunissen has a patent Novel CSF biomarkers for Alzheimer’s disease pending, and a patent Bri2 as a biomarker for Alzheimer’s disease pending. Dr Killestein received grants from Biogen Idec, Bayer Schering, Teva, Merck-Serono, Genzyme, Novartis, Glaxo SK, UCB. Dr. Tintore reports personal fees and non-financial support for scientific meetings from Biogen-Idec, Bayer, Merck-Serono, Genzyme, Novartis, Teva and Sanofi-Aventis outside the submitted work.
Ethical standard
This study have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All persons gave their informed consent prior to their inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Trentini, A., Comabella, M., Tintoré, M. et al. N-Acetylaspartate and neurofilaments as biomarkers of axonal damage in patients with progressive forms of multiple sclerosis. J Neurol 261, 2338–2343 (2014). https://doi.org/10.1007/s00415-014-7507-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-014-7507-4