Abstract
Over the past few years, the new psychoactive substances’ phenomenon has been continuously studied. Its dynamic context is characterized by a broad diversity of substances, including several groups, such as synthetic cathinones, synthetic opiates, and synthetic cannabinoids. However, and due both to this diversity and to the low number of detected cases, information on intoxication reports is always important, in order to understand their biological mechanisms. In this case, a male individual was found unresponsive, with some different powders and paraphernalia near him. After toxicological analysis to the powders, paraphernalia, and whole blood samples, five different compounds were identified. From these, two of them (3-MeO-PCP and o-desmethyltramadol) were identified and quantitated in the whole blood sample. The obtained results suggested that death was due to the presence and action of these two substances, in what may be considered an unusual mix of NPS. This case highlights the value of evaluating all the traces found in the scene investigation and the need of sending all the paraphernalia found for toxicological examination, together with all the possible information obtained on the scene, namely by relatives or witnesses. On the other hand, this case shows the significance of broad-spectrum analytical methods, in order to detect and identify, as specifically as possible, eventual substances present and used by victims.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Throughout the last years, the emerging phenomenon of new psychoactive substances (NPS) has been massively studied by research groups and monitored by the authorities, with new information spread both by public reports and by group alerts, in a regular basis [1, 2].
Being promoted as “legal highs,” NPS consumption offers an alternative to classic drugs, mainly due to the easiness of online-purchasing, their low price, and their undetectability by conventional drugs screening tests [3, 4]. Due to an always increasing number of available substances and a growing utilization by users, both consumers of common drugs or inexperienced users, the undesired effects of these NPS, even leading to death, started to be noted and described [1, 3].
Due to its diversity, NPS include several groups of substances. Among those, synthetic cathinones, synthetic cannabinoids, and novel opoids play an important role in this context [3].
Nevertheless, it is regularly reported that the number of detected NPS is quite low, especially if compared to the classical drugs’ groups [1, 2]. As so, evaluation of each particular case may provide further information about a specific substance or context. Thus, the authors intend to report a case of fatal intoxication with an unusual mix of NPS, under specific circumstances.
Case report
An individual, male, 25 years old, student of chemistry, with a past on drugs abuse, was found dead in his room at a boarding house where he lived. Social information referred schizophrenia and bipolar disorder. His relatives also referred that “he was trying to find a cure to his illness using chemical products bought by himself.”
Near him, a spoon, a syringe, and six different plastic bags were found with powders inside. Curiously, all the bags were labeled with the supposed name of the compounds.
A peripheral whole blood sample was collected for toxicological analysis, following the routine procedures applied at the Forensic Clinical and Pathology Service of the North Branch of the Portuguese National Institute of Legal Medicine and Forensic Sciences. This sample was sent to the North Branch lab of the Forensic Chemistry and Toxicology Service, along with the powders.
The powders, the syringe extract, and the spoon extract were analysed by GC–MS single quad. The blood sample was analysed for ethanol, drugs of abuse, and medicines, through the routine procedures applied at the lab, using GC-HS-FID, Enzimatic immunoassays, GC–MS single quadrupole, UPLC-MS/MS, and GC–MS/MS triple quadrupole.
Material and methods
Whole blood
Whole blood sample was collected at the femoral vein, according to the autopsy procedures of the Forensic Clinical and Pathology Department of the National Institute of Legal Medicine and Forensic Sciences.
The sample was analysed through specific procedures in force at the laboratory, namely, by GC-HS-FID for ethanol; screening enzymatic immunoassays for opiates, cocaine and metabolites, cannabinoids, amphetamines and derivates, and benzodiazepines; GC–MS single quadrupole for medicines screening (methods not published). Confirmation and quantification procedures included UPLC-MS/MS for benzodiazepines and GC–MS single quadrupole for the other medicines (procedures not published). As to cannabinoids is concerned, confirmation and quantification procedure was performed according to Castro et al. [5].
Confirmation and quantitation of 3-methoxyphencyclidine (3-MeO-PCP) and O-desmethyltramadol were performed according to Ferreira et al. [6]. In this method, a SPE procedure was applied to the whole blood samples, using OASIS® MCX cartridges. Cartridge condition and equilibration were achieved by adding 2 mL of methanol and 2 mL of deionized water to the cartridge. The sample was loaded onto the conditioned cartridge. For the washing step, 2 mL of sodium carbonate 0.15 M pH 9.5 buffer, followed by 2 mL of deionized water, and 3 mL of hexane were added to the column. After that, vacuum drying was carried out for half an hour. The samples were then eluted with 2 mL of dichloromethane/propan-2-ol/ammonia (78:20:2, v/v/v) mixture and evaporated to dryness. Finally, the dry eluates were silylated with 60 µL of BSTFA:TMCS (99:1) by heating at 65 °C, for 30 min, followed by instrumental analysis using GC–MS. Internal standards were PCP-D5 and tramadol-C13.D3 [6].
GC–MS analysis was performed using an Agilent 6890 N gas chromatograph (Agilent, Santa Clara, USA), with a J&W HP-5MS Capillary Column (30–0.25 mm i.d.–0.25-µm film thickness) (Agilent, Santa Clara, USA), coupled to an Agilent 5973 N simple quadrupole (Agilent, Santa Clara, USA). The temperature of the GC oven was initially set to run at 100 °C for 4 min, increased to 290 °C at 15 °C/min, and held at this temperature for 6 min, with a total run time of 27 min. The temperatures of the injector, transfer line, and source were set at 300 °C, 280 °C, and 230 °C, respectively. Helium (GASIN, Barcelona, Spain) was used as carrier gas with a flow rate of 1 mL/min for 18.5 min and 1.3 mL/min until the end of the run. The splitless mode was used to inject 2 µL of sample and the MS detector was operated in SIM mode. The retention time (in minutes) and monitored ions (m/z) for the analytes are as follows: PCP-D5 (13.165’, 205 m/z), tramadol-C13.D3 mono-TMS (13.611’, 339 m/z), O-desmethyltramadol di-TMS (14.040’, 58 m/z, 303 m/z, 393 m/z), 3-MeO-PCP (14.601’, 230, 272, 273) [6].
Powders, syringe extract, and spoon extract
The powders, the syringe extract, and the spoon extract were diluted in methanol and analysed, without derivatization, using a GC–MS single quad procedure. This direct analysis allowed positive identifications, based on the full scan MS spectrum, compared to Wiley MS Spectrum library.
Results
Powders
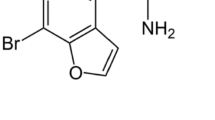
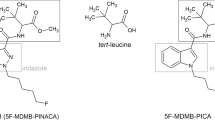
The analysis of the powders allowed a positive identification, compatible with the labeling of the bags. The powders’ identifications are described in Table 1.
Syringe extract and spoon extract
The analysis of the syringe and the spoon extracts detected the presence of three of the compounds, namely: 3-MeO-PCP, 5-MeO-DMT and O-DT.
Autopsy findings
The decedent was found to have pulmonary congestion and edema, as well as mild cerebral edema, aside congestion of internal organs. Needle prick marks in the victim’s arms were also noted.
Whole blood sample
The postmortem whole blood sample was positive for THC (1.2 ng/mL), THCCOOH (4.5 ng/mL), mianserine (74 ng/mL), topiramate (6.4 mg/L), levomepromazine (54 ng/mL), bromazepam (138 ng/mL), 3-MeO-PCP (525 ng/mL), and O-DT (4225 ng/mL). The sample was negative for other substances, namely other illicit compounds, ethanol, and other medicines (Table 2).
Discussion
Results interpretation is always a quest with specific issues, deep related to each case. As so, circumstantial evidence and social information, along with autopsy data and supplemental examinations (toxicology, histology, …) are pivotal for a representative interpretation of the reality of the case.
As to the powders, ID is concerned, and the results were compatible with the respective bags’ labeling. Curiously, the labels had an industrial production aspect, with information on purity (> 98%) and the usual information “not for human consumption.” This aspect suggests a targeted purchase, probably through an online channel, to an industrial producer, one of possible trading and distribution chains [2]. The noted variety of substances may be assessed in two ways: a concordance with social information, which claims a possible search for a cure for the psychiatric context of the victim, or a simple interest of the victim in different substances, experiencing and searching for different effects.
In this case, the presence of the syringe and the spoon may be indicative of the mode of preparation and consumption of the substances. As so, the substances detected in these extracts could be key indicators of the victim’s consumption context. From the five different compounds identified in the powders, three of them (3-MeO-PCP, 5-MeO-DMT, and O-DT) were present in these two extracts, suggestive of their consumption.
The information obtained through these supplemental samples is important and indicative of possible consumption inferences. However, only autopsy and, specifically, the whole blood sample analysis may represent the real state of the victim at the time of death.
Autopsy signs were indicative of drugs abuse, with needle prick marks in the victim’s arms.
As to the whole blood sample is concerned, the results were fruitful, with the identification and quantification of some compounds, representative of the clinical state of the victim and, most important, the identification of two of the compounds present in the spoon and the syringe extracts. As to the medicines are concerned (mianserin, topiramate, levomepromazine, and bromazepam), all of them show values compatible with a therapeutic context [7]. The presence of THC and THCCOOH is compatible with the drugs abuse’ history. So, it becomes clear that the presence of 3-MeO-PCP and O-DT was crucial to the cause of death.
3-Methoxy-PCP (3-MeO-PCP) is an analog of phencyclidine (PCP, “angel dust”), being a “legal high” and belonging to the phencyclidines class [4]. Due to its illicit context, no reference values are available for intoxication or death situations other than case reports. 3-MeO-PCP is expected to elicit effects similar to other NMDA antagonists, such as PCP, being an even more potent NMDA receptor antagonist than PCP [8, 9]. Individuals exposed to PCP and analogs may experience cardiovascular collapse, among other symptoms [8]. Fatal values found in the literature shown a range from 58 to 3200 ng/mL [4, 8,9,10,11] with a total of 11 reported cases. Reports refer generally some swelling of the brain and pulmonary edema [9, 10]. Noticeably, Johansson et al. describes a set of cases, in which just one shows the presence only of 3-MeO-PCP (380 ng/g), suggesting this one as a case of intoxication solely by this compound [9]. Likewise, Ameline et al. reported a fatal case with a concentration of 498 ng/mL [10]. In this case, the concentration detected, alongside autopsy findings, is compatible with an intoxication context.
O-desmethyltramadol (O-DT) is the main metabolite of tramadol, a centrally acting opioid analgesic commonly prescribed for pain control in a therapeutic approach concerning postoperative, dental, cancer, neuropathic, and acute musculoskeletal clinical contexts, being responsible for the main opioid analgesic effect, approximately 300 times more affinity to μ-opioid receptors than the parent compound [12]. To the authors’ knowledge, there are no published intoxication cases solely due to O-DT consumption. As so, all the cases found in the literature relate to tramadol consumption. Fonseca et al. describes mean values of 363 ng/mL of O-DT, in tramadol intoxication context, with a maximum of 3127 ng/mL. Moreover, Johansson et al. describe a case with tramadol (13000 ng/g) and O-DT (4600 ng/g), besides 3-MeO-PCP (80 ng/g) [9]. In this case, autopsy revealed pulmonary edema and congestion of internal organs, compatible with opioids intoxication [9, 13], suggesting that O-DT might have also been pivotal for the situation.
5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) is one of the main psychoactive ingredients of the secretion of the American desert toad, Bufo alvarius [14]. After consumption, 5-MeO-DMT is oxidatively demethylated in the human body, mediated by monoamine oxidase A (MAO-A) [14]. It seems that drug metabolism occurs extremely fast, as 5-MeO-DMT rapidly disappears in plasma. Thus, this substance behaves as a fast-acting hallucinogen with short duration, unless the consumer adds an MAO innibitor (such as harmaline) [15]. After intraperitoneal administration, 5-MeO-DMT reaches the maximum drug concentration (Cmax) at around 5–7 min, being then eliminated with a terminal half-life (t1/2) of 12–19 min in mice [15]. As so, this fact may justify the absence of the substance in the analyzed whole blood sample [14, 15].
As to interactions between drugs of abuse and established medication is concerned, some interesting points may also be considered. Topiramate is a glutamate-activated ion channels inhibitor, with a possible NMDA antagonist action [16]. As so, being 3-MeO-PCP among the most potent known NMDA antagonists [8, 9, 17], one may not rule out a possible potentiation of its effect.
On the other hand, the presence of mianserin might also be considered. Mianserin is known for its antidepressant action, through a dual mode of action. In parallel, its use in the context of chronic pain management has also been considered. Mianserin has shown an antinociceptive effect and, in a controlled study, mianserin induced a statistically significant potentiation of μ and κ-opioid receptors [18]. On the other hand, in tramadol clinical usage, the main opioid analgesic effect is attributed to ODT because it has approximately 300 times more affinity to μ-opioid receptors than the parent compound (tramadol) [12].
As so, one may also consider that it might have been some influence from these two medicines. However, these hypotheses needed further studies, mainly in terms of controlled administration of all the compounds and effects evaluation. Considering also that there is no information on doses and on verified effects before the individual death, no further conclusions can be drawn.
Concluding remarks
This case report’s novelty is based on the unusual mix of substances abused by the deceased.
From the toxicological findings, the 3-MeO-PCP concentration was high enough to contribute to the cause of death [4, 9]. Also, and consistent with an opioid overdose, the decedent was found to have pulmonary congestion and edema, as well as mild cerebral edema [9].
As so, medico-legal conclusions considered death by overdose due to 3-MeO-PCP and O-DT as the cause of death. However, it was not possible to discriminate between suicide and accidental overdose.
The authors would like to point out that, as this is a case report, drawing robust conclusions about the general behavior of the substances will always be risky. Thus, the characterization of these substances can only be consensual with the acquisition of additional data, either from other cases or from controlled studies.
This case highlights the importance of evaluating all the traces found in the scene investigation and sending all the paraphernalia found for toxicological examination, together with all the possible information obtained on the scene, namely by relatives or witnesses. On the other hand, this case shows the significance of broad-spectrum analytical methods, in order to detect and identify, as specifically as possible, eventual substances present and used by victims.
References
Vaiano F, Pascali JP, Bertol E (2019) New psychoactive substances: an actual problem or an overestimated phenomenon? Forensic Sci Int 304:109941. https://doi.org/10.1016/j.forsciint.2019.109941
EMCDDA (2020) European Drug Report 2020: trends and developments Lisbon. https://doi.org/10.2810/420678
Kraemer M, Boehmer A, Madea B, Maas A (2019) Death cases involving certain new psychoactive substances: a review of the literature. Forensic Sci Int 298:186–267. https://doi.org/10.1016/j.forsciint.2019.02.021
Jong LAA, Olyslager EJH, Duijst WLJM (2019) The risk of emerging new psychoactive substances: the first fatal 3-MeOPCP intoxication in The Netherlands. J Forensic Legal Med 65:101–104. https://doi.org/10.1016/j.jflm.2019.05.011
Castro AL, Tarelho S, Melo P, Franco JM (2018) A fast and reliable method for quantitation of THC and its 2 main metabolites in whole blood by GC–MS/MS (TQD). Forensic Sci Int 289:344–351. https://doi.org/10.1016/j.forsciint.2018.06.003
Ferreira AB, Castro AL, Tarelho S, Domingues P, Franco JM (2021) GC-MS – still standing for clinical and forensic analysis: validation of a multidrug method to detect and quantify illicit drugs. Aust J Forensic Sci. https://doi.org/10.1080/00450618.2021.1964598
Schulz M, Iwersen-Bergmann S, Andresen H, Schmoldt A (2012) Therapeutic and toxic blood concentrations of nearly 1,000 drugs and other xenobiotics. Crit Care 16:R136. http://ccforum.com/content/16/4/R136
Bakota E, Arndt C, Romoser AA, Wilson SK (2016) Fatal intoxication involving 3-MeO-PCP: a case report and validated method. J Anal Toxicol 40:504–510. https://doi.org/10.1093/jat/bkw056
Johansson A, Lindstedt D, Roman M, Thelander G, Nielsen EI, Lennborn U, Sandler H, Rubertsson S, Ahlner J, Kronstrand R, Kugelberg FC (2017) A non-fatal intoxication and seven deaths involving the dissociative drug 3-MeO-PCP. Forensic Sci Int 275:76–82. https://doi.org/10.1016/j.forsciint.2017.02.034
Ameline A, Greney H, Monassier L, Raul J, Kintz P (2019) Metabolites to parent 3-MeO-PCP ratio in human urine collected in two fatal cases. J Anal Toxicol 43:321–324. https://doi.org/10.1093/jat/bky097
Mitchell-Mata C, Thomas B, Peterson B, Couper F (2017) Two fatal intoxications involving 3-methoxyphencyclidine. J Anal Toxicol 41:503–507. https://doi.org/10.1093/jat/bkx048
Fonseca S, Amorim A, Costa HA, Franco J, Porto MJ, Santos JC, Dias M (2016) Sequencing CYP2D6 for the detection of poor-metabolizers in post-mortem blood samples with tramadol. Forensic Sci Int 265:153–159. https://doi.org/10.1016/j.forsciint.2016.02.004
Krotulski AJ, Papsun DM, Friscia M, Swartz JL, Holsey BD, Logan BK (2018) Fatality following ingestion of tetrahydrofuranylfentanyl, U-49900 and methoxy-phencyclidine. Anal Toxicol 42(3):e27–e32. https://doi.org/10.1093/jat/bkx092
Araújo AM, Carvalho F, Bastos ML, Pinho PG, Carvalho M (2015) The hallucinogenic world of tryptamines: an updated review. Arch Toxicol 89:1151–1173. https://doi.org/10.1007/s00204-015-1513-x
Shen H, Jiang X, Winter JC, Yu A (2010) Psychedelic 5-methoxy-N, N-dimethyltryptamine: metabolism, pharmacokinetics, drug interactions, and pharmacological actions. Curr Drug Metab 11(8):659–666. https://doi.org/10.2174/138920010794233495
Rawls SM, Thomas T, Adeola M, Patil T, Raymondi N, Poles A, Loo M, Raffa RB (2009) Topiramate antagonizes NMDA- and AMPA-induced seizure-like activity in planarians. Pharmacol Biochem Behav 93:363–367. https://doi.org/10.1016/j.pbb.2009.05.005
Roth BL, Gibbons S, Arunotayanun W, Huang X-P, Setola V et al (2013) The ketamine analogue methoxetamine and 3- and 4-methoxy analogues of phencyclidine are high affinity and selective ligands for the glutamate NMDA receptor. PLoS ONE 8(3):e59334. https://doi.org/10.1371/journal.pone.0059334
Schreiber S, Backer MM, Kaufman JP, Pick CG (1998) Interaction between the tetracyclic antidepressant mianserin HCl and opioid receptors. Eur Neuropsychopharmacol 8:297–302
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
In memoriam
José Eduardo Lima Pinto da Costa (1934–2021)
Rights and permissions
About this article
Cite this article
Castro, A.L., da Costa, M.J.C.S.P., Tarelho, S. et al. Intoxication by 3-MeO-PCP and O-desmethyltramadol: an unusual NPS mix. Int J Legal Med 136, 1297–1301 (2022). https://doi.org/10.1007/s00414-022-02818-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-022-02818-w