Abstract
Age estimation of living individuals is a regular activity in medico-legal practice. Among the available tools for determining skeletal age, some authors have stated that the disappearance of epiphyseal scars could be a useful marker. The aim of the present study was to assess whether the presence of an epiphyseal scar on the knee, as seen on a plain X-ray, was linked to biological age. A total of 988 frontal X-rays of individuals (509 females and 479 males) aged between 15 and 40 years were analyzed to see whether a scar was visible or not on each of the three epiphyses of the knee. A scar was visible for 96 % of the females and 98 % of the males. For each sex, scars were visible at each year of age, from 15 to 40 years. In younger females, there were 15 individuals with no scar visible on the fibula, 16 on the tibia, and 20 on the femur. For males, the ages were respectively 16, 17, and 18 years. On a frontal X-ray, the persistence of epiphyseal scars was not a marker of a recent fusion. All individuals with fully ossified knee that had no scar on the femur were older than 18 years. Further studies focusing on epiphyseal scars on MR and CT scans could be useful, as these techniques allow the more precise analysis of the epiphysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An epiphyseal scar is a thin layer of dense bone localized at the place where the growth plates existed [1], resulting from the fusion between epiphysis and metaphysis. They are also known as “epiphyseal lines”, “lines of persistent fusion”, “terminal lines”, or “epiphyseal ghosts” [1, 2]. On a plain X-ray, they appear as a line of thin compact tissue, sometimes broken, or as a narrow belt of cancellous tissue that is denser than the bone on either side [1]. They can also be seen on dry bones [3]. Cope was the first author to describe them in 1920, as fusion lines of bones. In his publication, he stated that epiphyseal scars can be seen until a late period of life, the most remarkable persistence being at the lower end of the femur and the upper end of the tibia, until 60 and even 70 years old [1]. Cope claimed that they should be interpreted with care, because not acknowledging their persistence may lead to underestimating the age of the individual.
Since then, many studies have been performed on various anatomical regions and have led to different conclusions. In the vast majority of the radiological studies dealing with the chronology of bone fusion [e.g., 4–14], epiphyseal scars are either cited without interpretation [4, 6, 7, 12] or mentioned as a possible indicator of a recent fusion [9–11, 13]. By analyzing the medial clavicular epiphysis on chest X-rays, Schmeling et al. [10] was the first to establish a radiological classification acknowledging scar visibility. In this classification, the two last stages were defined according to whether a scar was visible or not on a fully ossified metaphysis. Schmeling et al. were the first to make the hypothesis that an epiphyseal scar of the clavicle could be incorporated into a radiological classification made for age estimation, its disappearance being an additional stage of maturation. Several further studies have confirmed the accuracy of this classification [e.g., 11, 13, 14].
There is a lack of knowledge about epiphyseal scars and their potential link with the biological age [15], because studies focused on them or taking them on board are few in number. Indeed, the area in which the scar has been the most comprehensively studied is the clavicle [10, 11, 13, 14], and the scars of the tibial extremities were exclusively analyzed in a recent study [15]. This study had not found any relationship between their persistence rate and biological age. Thus, it seems useful to develop studies about epiphyseal scars on different joints, to constitute a reference standard. Cope made the hypothesis that the scars were more persistent on the joints of the lower limbs than the upper limbs, because more mechanical stress must exist on them [1]. Therefore, it is possible that the persistence time frame of scars may be helpful in some areas and not others.
The main aim of our study was to assess whether the presence of an epiphyseal scar on a frontal radiograph of the knee was a predictive marker of biological age for each sex and for each of the three epiphyses of the knee. We chose to study the knee, because the metaphyseal-epiphyseal fusion of the knee has already been widely studied on dry bones [3, 12, 16], plain X-rays [12, 15], or MRI [17, 18], and the ages of union are well documented in the literature [12].
Material and methods
Material
We retrospectively reviewed frontal radiographs of individuals aged between 15 and 40 years, performed in the Radiology Department of a French University Hospital between January 2008 and December 2013. Radiographs were obtained through a Picture Archiving and Communication System (PACS, McKesson Medical Imaging Group, Richmond, BC, Canada) used by the hospital. Twenty radiographs were initially chosen for each year of age for males and females. Subjects were included if they had a good quality X-ray with strict anteroposterior incidence. If right and left sides were available for the same individual, the left one was selected for analysis. The collected variables were sex and age. Subjects were excluded if they had any pathology of the knee (tumor, surgery, bone drilling, infection, cast, or osteosynthesis equipment), and if the prescription of the X-ray was made by endocrinologists, rheumatologists, or an internal medicine department, because this could suggest knee or systemic pathologies that perturb bone maturation. Ethnicity and socioeconomic status were not available for our cohort.
Examination of the radiographs
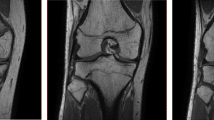
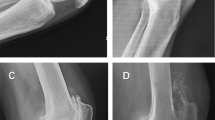
First, all individuals with an incomplete bone fusion on the distal femur or proximal tibia or fibula epiphysis were excluded. Then, for the remaining radiographs, the three epiphyses (the distal femur, the proximal tibia, and the proximal fibula) were evaluated by a first observer (MF) with one criterion: whether an epiphyseal scar was visible (Fig. 1) or not (Fig. 2). A random selection of 200 X-rays was read by the first observer after a 2-week interval for intraobserver variability evaluation and by a second observer (CR) for interobserver variability. The two observers were medico-legal physicians with training in forensic age estimation.
Evaluation of the scars
An epiphysis classified as “visible” was an epiphysis where a scar was visible on the knee anteroposterior X-ray, regardless of whether the scar was full (spreading on all the length of the metaphyseal area), discontinuous, or incomplete. For an analysis free of subjectivity as much as possible, we chose to not retain those pictures with uncertainty regarding the presence of a scar. The thickness of denser bone area had to be larger than those of the framework of cancellous bone in order to be considered as a scar. The areas where two bone structures were superimposed were analyzed by modulating the contrast of the image. Finally, the denser bone area had to correspond to the growth plate by its localization and its form. Those pictures not meeting these criteria were classified as “no scar”.
Statistical analysis
MS Excel© was used to organize and code the variables. Statistical parameters and tests were accomplished by JMP© Pro 10.0.0. Significance was assessed at p < 0.05, two sided. A nonparametric test (Mann–Whitney) was chosen to compare the mean ages of “no scar” and “visible scar” groups, because the age repartition of the sample did not have a Gauss distribution.
Results
In total, 1040 radiographs of individuals aged between 15 and 40 years were initially selected. Here, 52 were excluded because they had ongoing fusion of at least one growth plate of the knee. These individuals were aged between 15 and 19 years, and consisted of 41 males and 11 females. The final sample consisted of 988 individuals, 509 females and 479 males (Table 1). Table 2 shows intra- and interobserver variability.
For each bone, epiphyseal scars could be seen for each age of the sample. Results of the Mann–Whitney test and statistical parameters are presented in Tables 3 (females) and 4 (males). Figure 3 presents the proportions of “Visible Scar” and “No Scar” groups for each year according to sex and bone.
A scar was visible on the three epiphyses for all ages of females and males. The youngest females with no visible scar were 15 years old for the fibula, 16 for the tibia, and 20 for the femur. The youngest males with no visible scar were 16 years old for the fibula, 17 for the tibia, and 18 for the femur.
For the distal femur, a statistically significant age difference was found between the “no scar” and “visible scar” groups for each sex. The mean age of the “no scar” group was higher than the group with a scar for females (p = 0.0086) and males (p = 0.0440). For the proximal tibia and fibula, no significant age difference was found between “no scar” and “visible scar” groups for each sex.
For the females, respectively for the “no scar” and “visible scar” groups, the median age was 32 and 27 years for the femur, 29.5 and 28 years for the tibia, 28 and 27 years for the fibula. For the males, respectively for the “no scar” and “visible scar” groups, the median age was 32.5 and 28 years for the femur, 27 and 29 years for the tibia, 30 and 28 years for the fibula.
A scar could be seen on at least one epiphysis of the knee for 96 % of the females and 98 % of the males. Regardless of sex, the large majority of individuals retained a scar: 95 % of the femur, 96 % of the tibia, and 54 % of the fibula.
Discussion
The present study is, to the best of our knowledge, the third to deal with the topic of epiphyseal scarring and its possible role in forensic age estimation, and the only one to have specifically analyzed three epiphyseal scars of the knee. In 2008, O’Connor et al. performed a large-scale study of a contemporary population. They created a bone fusion classification in which epiphyseal scars were described but not used to define the last stage of bone maturation. They found that sex and the origin of the population had a major influence on the bone fusion. They also highlighted that it was extremely difficult to find a consensus on ages regarding epiphyseal union of the knee. More recently, Davies et al. evaluated the persistence of epiphyseal scars in the proximal and distal extremities of the tibia. They observed that the more persistent the scar, the younger the individuals. However, they concluded that an epiphyseal scar should not be interpreted as a marker of recent bone fusion and should not be used for forensic age estimation, because they found that the factors combining age, sex, body side, and bone extremity could only explain 15.9 % of the variation of the persistence of the scar. They also found that most of their individuals retained a scar.
A statistically significant age difference was found for the distal femur, suggesting that people without a scar were statistically older than those with an X-ray visible scar, supporting the hypothesis that scars can be included in a one-way physiological process, in which the bone grows, can get an epiphyseal scar when ossification is completing, and the scar can eventually persist or disappear after a variable period.
However, our study suggests that the longevity of epiphyseal scars of the knee is not useful for age estimation, for two reasons. The first and main reason is that a scar was visible for all ages of our male and female samples. This implies that the persistence of an epiphyseal scar on an epiphysis of the knee cannot be considered an indicator of its recent fusion. It also suggests that the knee scars persist for a long period of time and is in agreement with Cope’s hypothesis about the influence of mechanical stress. The superior limit of our sample was 40 years; thus, it cannot be excluded that individuals older than 40 years may be more likely to be scar free. Weiss et al. observed epiphyseal scars persisting on the first metatarsal up to 80 years [2]. The second one is that no statistical difference was found for the proximal tibia and fibula. This discrepancy cannot be explained from a physiological point of view. Indeed, the mechanical constraints should be the same within the lower limb and one would expect the same result for the femur and the tibia. Moreover, in two studies, the authors have observed a similar maturation kinetic for the femur and the tibia [12, 18]. Furthermore, this discrepancy can result from a statistical artifact. Indeed, the largely uneven repartition between “no scar” and “visible scar” groups should influence their mean age one way or the other, by the weight of outlier data. Indeed, the mean age of the “no scar” group could be overvalued or undervalued respectively for the femur and the tibia. Therefore, the persistence of an epiphyseal scar on an epiphysis of the knee is not an indicator of its recent fusion.
The main limit of this analysis was superimposed effects, which is a well-known limitation for all studies using conventional radiography [19]. A recent study by Wittschieber [20] showed this limit for the medial clavicular extremity analyzed on chest X-rays. A similar study using a cross-section exam (CT or MR scans) would be interesting, because it will be free of any superimposed effect.
Several studies have been performed on radiography of the lower extremity in the perspective of forensic age estimation. The analysis of iliac crest ossification is interesting for the 14 and 16 year threshold [21, 22], but it leads to irradiation of the gonadal area. The epiphyseal scars of the upper and lower tibial extremities do not seem to be linked to biological age [15]. Other studies have tried to adapt radiological atlases of the knee considered as standard references in a forensic age estimation perspective [12, 23, 24].
During the analysis, the authors noted that individuals who had fully ossified femoral, tibial, and fibular epiphyses and no scar on the femoral epiphysis were at least 18 years old for males and 20 years old for females. This result is particularly interesting, because 18 years is the age of majority—and thus the most important age threshold—in several European countries. Recently, two other examinations have been found to be useful for the 18-year threshold: the clavicular CT scan for both sexes [13, 14] and the femoral MR scan for males [18, 25]. CT scans are known to expose the individual to radiation, and MRI scans are difficult to obtain in public hospitals because they are dedicated to patients. Plain X-ray of the left hand and wrist is analyzed most of the time with the Greulich and Pyle method, but are not very contributive for individuals older than 16 years, because ossification is complete. Thus, the addition of an X-ray of another anatomical area, showing good results regarding the 18 year threshold, would be important in a forensic perspective. However, in our sample, only 5 % of the individuals were concerned by the absence of a femoral scar, which means that a very large majority of our sample had kept a scar. Thus, the frontal X-ray of the knee cannot be recommended as a reference method in forensic age estimation, but can be analyzed if it is already available for the individual, because it has been performed in a medical context for example.
To conclude, epiphyseal scars can be viewed from two approaches: their persistence and their disappearance:
-
1.
Epiphyseal scars of the knee are visible on an anteroposterior X-ray for a long period of time: up to 40 years old, and maybe even beyond that limit. Therefore, the persistence of an epiphyseal scar on an anteroposterior X-ray is not an indicator of a recent fusion of the knee and does not seem to be correlated to biological age.
-
2.
The minimum age of disappearance can be useful for age estimation, because all individuals with a fully ossified knee and no femoral scar were at least 18 years old.
References
Cope Z (1920) Fusion-lines of bones. J Anat 55:36–37
Weiss E, DeSilva J, Zipfel B (2012) Brief communication: radiographic study of metatarsal one basal epiphyseal fusion: a note of caution on age determination. Am J Phys Anthropol 147:489–492
McKern TW, Steward TD (1957) Skeletal age changes in young American males, analysed from the standpoint of age identification. Headquarters Quatermaster Research and Development Command, Technical Report EP-45, Natick
Davis DA, Parsons FG (1927) The age order of the appearance and union of the normal epiphyses as seen by X-rays. J Anat 62(Pt 1):58–71
Paterson RS (1929) A radiological investigation of the epiphyses of the long bones. J Anat 64:28–46
Flecker H (1931) Roentgenographic observations of the times of appearance of epiphyses and their fusion with the diaphyses. J Anat 67(Pt1):118–164
Greulich WW, Pyle SI (1959) Radiographic atlas of skeletal development of the hand and wrist. Stanford University Press, Stanford
Hoerr NL, Pyle SI, Francis CC (1962) Radiographic atlas of skeletal development of the foot and ankle: a standard of reference. Charles C Thomas, Springfield
Pyle SI, Hoerr NL (1969) A radiographic standard of reference for the growing knee. Charles C. Thomas, Springfield
Schmeling A, Schultz R, Reisinger W, Mïhler M, Wernecke KD, Geserick G (2004) Studies on the time frame for ossification of the medial clavicular epiphyseal cartilage in conventional radiography. Int J Legal Med 118:5–8
Schulz R, Mühler M, Mutze S, Schmidt S, Reisinger W, Schmeling A (2005) Studies on the time frame for ossification of the medial epiphysis of the clavicle as revealed by CT scans. Int J Legal Med 119:142–145
O’Connor JE, Bogue C, Spence LD, Last J (2008) A method to establish the relationship between chronological age and stage of union from radiographic assessment of epiphyseal fusion at the knee: an Irish population study. J Anat 212:198–209
Kellinghaus M, Schultz R, Vieth V, Schmidt S, Schmeling A (2010) Forensic age estimation in living subjects based on the ossification status of the medial clavicular epiphysis as revealed by thin-slice multidetector computed tomography. Int J Legal Med 124:149–154
Kellinghaus M, Schultz R, Vieth V, Schmidt S, Pfeiffer H, Schmeling A (2010) Enhanced possibilities to make statements on the ossification status of the medial clavicular epiphysis using an amplified staging scheme in evaluating thin-slice CT scans. Int J Legal Med 124:321–325
Davies C, Hackman L, Black S (2014) The persistence of epiphyseal scars in the adult tibia. Int J Legal Med 128:335–343
Scheuer L, Black S (2000) Developmental Juvenile Osteology. Elsevier/Academic Press, Amsterdam
Dedouit F, Auriol J, Rousseau H, Rougé D, Crubézy E, Telmon N (2012) Age assessment by magnetic resonance imaging of the knee: a preliminary study. Forensic Sci Int 217:231.e1–232.e7
Krämer JA, Schmidt S, Jügens KU, Lentschig M, Schmeling A, Vieth V (2014) Forensic age estimation in living individuals using 3.0T MRI of the distal femur. Int J Legal Med 128(3):509–514
Schulz R, Mühler M, Reisinger W, Schmidt S, Schmeling A (2008) Radiographic staging of ossification of the medial clavicular epiphysis. Int J Legal Med 122:55–58
Wittschieber D, Ottow C, Vieth V, Küppers M, Schulz R, Hassu J, Bajanowski T, Püschel K, Ramsthaler F, Pfeiffer H, Schmidt S, Schmeling A (2014) Projection radiography of the clavicle: Still recommendable for forensic age diagnostics in living individuals? Int J Legal Med. doi:10.1007/s00414-014-1067-0
Wittschieber D, Schmeling A, Schmidt S, Heindel W, Pfeiffer H, Vieth V (2013) The Risser sign for forensic age estimation in living individuals: a study of 643 pelvic radiographs. Forensic Sci Med Pathol 9(1):36–43
Wittschieber D, Vieth V, Domnick C, Pfeiffer H, Schmeling A (2013) The iliac crest in forensic age diagnostics: Evaluation of the apophyseal ossification in conventional radiography. Int J Legal Med 127:473–479
O’Connor JE, Coyle J, Bogue C, Spence LD, Last J (2014) Age prediction formulae from radiographic assessment of skeletal maturation at the knee in an Irish population. Forensic Sci Int 234:188.e1–188.e8
Hackman L, Black S (2013) Age estimation from radiographic images of the knee. J Forensic Sci 58(3):732–737
Saint-Martin P, Rerolle C, Pucheux J, Dedouti F, Telmon N (2014) Contribution of distal femur MRI to the determination of the 18-year limit in forensic age estimation. Int J Legal Med. doi:10.1007/s00414-014-1020-2
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faisant, M., Rerolle, C., Faber, C. et al. Is the persistence of an epiphyseal scar of the knee a reliable marker of biological age?. Int J Legal Med 129, 603–608 (2015). https://doi.org/10.1007/s00414-014-1130-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-014-1130-x