Abstract
Although radiotherapy is widely employed in the treatment of various malignancies in oncology patients, its use is limited by the toxic effects it causes in surrounding tissues, including the gastrointestinal system. Korean Red Ginseng (KRG) is a traditional drug reported to possess antioxidant and restorative properties in various studies. The purpose of the present study was to investigate the protective effects of KRG against radiation-associated small intestinal damage. Twenty-four male Sprague Dawley rats were randomly assigned into three groups. No procedure was performed on Group 1 (control) during the experiment, while Group 2 (x-irradiation) was exposed to radiation only. Group 3 (x-irradiation + ginseng) received ginseng via the intraperitoneal route for a week prior to x-irradiation. The rats were killed 24 h after radiation. Small intestinal tissues were evaluated using histochemical and biochemical methods. An increase in malondialdehyde (MDA) levels and a decrease in glutathione (GSH) were observed in the x-irradiation group compared to the control group. KRG caused a decrease in MDA and caspase-3 activity and an increase in GSH. Our findings show that it can prevent damage and apoptotic cell death caused by x-irradiation in intestinal tissue and can therefore play a protective role against intestinal injury in patients receiving radiotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global death toll due to cancer is approximately 7.6 million (Jemal et al. 2011). Radiotherapy, widely employed to kill cancer cells and shrink tumor cells, is performed on 50% of cancer patients and is known to exhibit therapeutic effects in 40% of patients (Delaney et al. 2005). Although radiation therapy is a successful technique in cancer patients, it can also harm surrounding cells since it is not selective (Bellïes et al. 2017). Studies have reported that radiotherapy also leads to damage in the gastrointestinal system (Mercantepe et al. 2019). Even low doses of radiation therapy applied for tumors in the pelvis, abdomen, and colorectal system induce chronic intestinal problems (Zhang et al. 2013; Suman et al. 2017). Radiotherapy-related intestinal damage affects the treatment of various types of cancer and adversely impacts on quality of life (Lu et al. 2019).
Although the damage mechanism of radiotherapy is not yet fully understood, radiation is known to cause damage through an increase in reactive oxygen species (ROS) as a result of direct and indirect exposure of the target molecule to ionization (Broin et al. 2015). Studies show that an increase in ROS causes changes in antioxidant enzyme levels by triggering oxidative stress. In addition, recent studies have shown that oxidative stress associated with an increase in ROS triggers caspase-dependent apoptosis by leading to damage in DNA (Cho et al. 2017; Mercantepe et al. 2019).
Korean Red Ginseng (KRG), used as a traditional medicinal plant in Asian countries in particular for many hundreds of years, is a phytotherapeutic agent containing phenolic acids, flavonoids, and triterpenoid saponins. Studies have shown that ginseng possesses antibacterial, antiviral, antioxidative, antiapoptotic, antitumor, and immune modulatory properties (Park et al. 2009, 2012; Xu et al. 2011). KRG is also reported to be effective in various forms of tissue damage, including radiation-related tissue injury (Verma et al. 2011). However, the effect of ginseng on small intestinal damage caused by x-irradiation is unknown.
This study examined the contribution of phytoprotective agents to antioxidant mechanisms in future novel therapeutic methods against oxidative stress and apoptotic cell injury caused by x-irradiation in the rat small intestine.
Materials and methods
Animals
Twenty-four male Sprague–Dawley rats weighing 280 ± 30 g and aged 14–16 weeks were obtained from the Recep Tayyip Erdoğan University Experimental Animals Application and Research Center (Rize, Turkey). The rats were housed under controlled conditions in 50–60% humidity, 22 ± 1 °C temperature, and a 12-h light:dark cycle. Ad libitum access was permitted to drinking water and standard pellet chow (Bayramoğlu, Erzurum, Turkey). Experimental procedures were carried out in accordance with the directives for the care and use of laboratory animals. The study protocol was approved by the Recep Tayyip Erdoğan University local animal care committee (Rize, Turkey, decision no. 2021/14 dated 27.05.2021).
Experimental design
The rats were randomly assigned into a control group, an x-irradiation group, and an x-irradiation + ginseng group (n = 8). In Control (Group 1), only saline solution was administered intraperitoneally without any irradiation. (Uzal et al. 2012). Group 2 (the x-irradiation group) was exposed to a single dose of 6 Gy whole-body x-irradiation. Group 3 (x-irradiation + ginseng) was exposed to a single dose of 6 Gy whole-body X-ray irradiation and a single dose of 200 mg/kg Korean red ginseng was administered intraperitoneally a week prior to irradiation (Lee et al. 2013; Ullah et al. 2021).
All rats were sacrificed 24 h after irradiation, and their small intestinal tissues were successfully removed. One part of the small intestinal specimens was stored at − 80 °C for biochemical examination, and the other part was kept in 10% formalin for histochemical and immunohistochemical examinations.
Abdominal irradiation
Prior to irradiation, rats were anesthetized using ketamine and xylazine and were fixed in a supine position by the legs and tail. The animals were irradiated from the posterior and anterior using a 1 cm bolus in a 20 cm × 40 cm field with a 6-MV isometric method. Photon radiation (X-Ray) was applied at a dose of 6 Gy at 6 MV a minute using a linear accelerator (Elekta Synergy; Elekta, Crawley, UK) and a CMS-XIO radiotherapy treatment planning system (version 13.2) (Rakici 2020). Irradiation was carried out in our center’s radiation oncology department. The dose employed was set at 6 Gy in accordance with the dosage employed in previous studies (Zhang 2013).
Chemicals and extract
Irradiation and sacrification procedures were performed while the rats were under anesthesia. Anesthesia was induced with ketamine (100 mg/kg, Ketalar, Pfizer Pharma, Istanbul, Turkey) and xylazine (3.9 mg/kg, Xylazin Bio 2%, Interhas A.S., Istanbul, Turkey). Korean red ginseng extract (Dong il Co. Ltd., Gyeonggi-do, Korea) contained 6-year-old, domestic, the sum of ginsenoside Rg1 and Rb1 is 7.3 mg/g, solid contents are 60% or more, and 37% other minor ginsenosides.
Histopathological examination
Small intestine specımens were fixed for 48 h in 10% formaldehyde (Sigma-Aldrich, St. Louis, MO, USA). After fixation, they were passed through increasing alcohol series for dehydration (Sigma-Aldrich, St. Louis, MO, USA) and rendered transparent with xylol (Sigma-Aldrich, St. Louis, MO, USA). Following the absorption procedure, the specimens were embedded in paraffin blocks (Merck, Darmstadt, Germany). Tissue processing was conducted using an autotechnicon device (Citadel 2000 Shandon, Thermo Scientific, Cheshire, UK). Small intestine specimens were stained with hematoxylin (Harris hematoxylin, Merck, Darmstadt, Germany) and eosin (Merck, Darmstadt, Germany) on a staining device (Leica St 5020, Leica Microsystems, Wetzlar, Germany) for morphological examination. Sections 2–3 µ in thickness were collected from the paraffin blocks using a microtome (Leica R < 2525, Lecia, Germany) and deparaffinized for 1 h in a 60 ℃ stove. The tissues were then passed through decreasing alcohol series and washed with distilled water for 5 min. The tissues stained with hematoxylin and eosin (H&E) were passed through increasing alcohol series, placed into xylol, and covered with Entellan (Merck, Darmstadt, Germany). The small intestine sections obtained after staining were examined under a light microscope (Olympus BX51, Olympus Corporation, Tokyo, Japan) and photographed (Olympus DP71, Olympus Corporation, Tokyo, Japan).
Immunohistochemical examination
In order to determine apoptotic cell death in the small intestinal tissues, these were subjected to immunohistochemical staining using cleaved caspase-3 primary antibody (Asp175, 1/200, Cell Signaling Technology, Leiden, The Netherlands), secondary antibody (Goat Anti-Rabbit IgG H&L, HRP, ab205718, Abcam), and an immunohistochemistry detection kit (ab64264, Abcam). Sections 2–3 µ in thickness from the paraffin blocks were placed onto poly-l-lysine-coated slides for immunohistochemical examination. Following deparaffinization with xylol (Sigma-Aldrich, St. Louis, MO, USA), the small intestinal tissues were rehydrated by being passed through decreasing alcohol series. The tissues were then washed with PBS (phosphate-buffered solution) and treated with hydrogen peroxide (H2O2) to prevent endogenous peroxidase activity. After washing with PBS, protein blocking solution was dropped onto the tissues, which were then incubated with caspase-3 primary antibody for 1 h. Following primary antibody application, the tissues were then treated with secondary antibody for 30 min. Streptavidin peroxidase was dropped onto the tissues. This was followed by DAB being dropped onto the tissues, after which they were left in the dark. After DAB staining, the tissues were counterstained with Harris hematoxylin and covered with Entellan (Merck, Darmstadt, Germany). The preparates were examined and evaluated under a light microscope (Olympus BX51, Olympus Corporation, Tokyo, Japan).
Semi-quantitative analysis
Histopathological changes observed in villi and crypts in small intestine sections following H&E staining were scored using Elliot’s intestinal mucosal damage score (Table 1) (Elliott et al. 2014).
Caspase-3 immunoreactivity in small intestine tissues was scored 1 (mild; ≤ 5%), 2 (moderate; ≥ 10%), 3 (severe; ≥ 25%), and 4 (extremely severe; ≥ 50%), depending on positivity distribution at semi-quantitative analysis (Mercantepe et al. 2019). Histochemical and immunohistochemical scoring was performed by two blinded independent histologists.
Biochemical analysis
Tissue sampling and homogenization
A mixture of 20 mM 1L sodium phosphate + 140 mM potassium chloride (pH 7.4) was first prepared. Next, 1 mL homogenate buffer per 100 mg tissue was homogenized for 5 min with a Tissue Lyser II device (Qiagen, Hilden, Germany), followed by centrifugation for 10 min at 800g at 4 °C. The resulting supernatant was then used for malondialdehyde (MDA) and GSH assays.
Malondialdehyde analysis
Malondialdehyde levels were measured using a modified Draper and Hadley technique (Draper and Hadley 1990). The reaction mixtures made ready by following this method were kept in ice water for 15 min following the incubation period. The final pink color was read on a spectrophotometer at 532 nm.
Glutathione analysis
Reduced glutathione (GSH) assay was performed with Ellman’s reagent (Ellman 1959). The objective here was to determine the color of free sulfhydryl groups in ovarian tissue homogenates by means of Ellman’s reagent and spectrophotometry. Briefly, a mixture of 200 µL 3 M Na2HPO4 and 50 µL DTNB (4 mg DTNB prepared in 1% 10 mL sodium citrate solution) were added to 50 µL supernatant. The resulting mixture was then vortexed, and the absorbance measurement was at 412 nm.
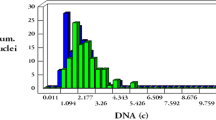
Statistical analysis
The study data were analyzed using the Shapiro–Wilk, Q-Q plot, Skewness–Kurtosis, and Levene’s tests on SPSS version 18.0 software (SPSS Inc., Chicago, IL, USA). Parametric data were calculated as mean ± standard deviation. Differences between groups were analyzed using One-Way ANOVA followed by Tukey’s HSD test. Non-parametric data were calculated as median values (25–75% interquartile range). Differences between groups were analyzed using the Kruskal–Wallis and Tamhane T2 tests. p values < 0.05 were regarded as significant for all analyses.
Results
Histopathological analysis
Examination of H&E-stained small intestinal tissue sections under light microscopy revealed a normal-appearing morphology in the control group. The intestinal villi were surrounded by regular epithelial cells with a normal brush border appearance and a normal lamina propria (damage score: 0.5(0–1)) (Fig. 1A–B, Table 2). However, in the x-irradiation group, fusions were present in the intestinal villi, and villus numbers had decreased. In addition, impairments were observed in the epithelial cells surrounding the villi and the brush borders. Moreover, hemorrhagic areas were observed in the lamina propria, together with vascular congestion (damage score: 2(2–3)) (Fig. 1C–D, Table 2). In the x-irradiation + ginseng group, the structures of the intestinal and crypt exhibited a typical appearance. The intestinal villus epithelium was regular in appearance, with a marked brush border. Decreases were also observed in hemorrhagic areas and vascular (damage score: 2(1–2)) (Fig. 1E–F, Table 2).
Representative light microscopic image of small intestinal tissues stained with H&E H. A (× 20) and B (× 40): Villus (v) with lamina propria surrounded by epithelium and crypt (c) in small intestinal tissues from the control group. Typical brush border (arrow) and goblet cell (arrow head). C (× 20) and D (× 40): Fusions in villus structures and decreased crypt structures in small intestinal tissues from the radiotherapy group. Impairments (tailed arrow) in the appearance of the brush borders in epithelial cells and widespread hemorrhagic areas (star) and vascular congestions (Vc) can also be seen. E (× 20) and F (× 40): Numerous typical villi and crypt structures in small intestinal tissues from the radiotherapy + ginseng group. Regular brush borders and normally distributed goblet cells can also be seen
Immunohistochemical analysis
Caspase-3-positive cells with brown cytoplasmic content were determined following caspase-3 immunostaining of small intestinal tissues. Caspase-3 positivity scores increased significantly in the x-irradiation group (Caspase-3 positivity score: 3(2–3.5)) compared to the control group (Caspase-3 positivity score: 1(1–1.5, p < 0.05, Fig. 2A–B, Table 3). However, caspase-3 positivity scores decreased significantly in the x-irradiation + ginseng (Caspase-3 positivity score: 1(1–2)) compared to the x-irradiation group (p < 0.05, Fig. 2B–C, Table 3).
Representative image of small intestinal tissues stained immunohistochemically with cleaved caspase-3. A (40×) Normal-looking enterocytes from the control group (arrow) (cleaved caspase-3 positivity score: 1(1–1.5)). B (40×) widely stained apoptotic cells (arrow head) X-ray in the villus epithelium and a small number of normal enterocyte cells (arrow) in the x-irradiation group (cleaved caspase-3 positivity score: 3(2–3.5)). C (40×) a small number of apoptotic cells (arrow head) and widespread typical enterocyte cells in the x-irradiation + ginseng group (cleaved caspase-3 positivity score: 1(1–2))
Biochemical analysis
MDA analysis results
MDA values in the control group were significantly lower than those in both the X-ray irradiation group and the x-irradiation + ginseng group (p = 0.016 and p = 0.043, respectively, Table 4). MDA values were also significantly lower in the x-irradiation + ginseng group than in the x-irradiation group (p = 0.014, Table 4).
GSH analysis results
GSH levels were significantly higher than in the control group and the x-irradiation group (p = 0.003, Table 4). Similarly, a significant difference was observed between the x-irradiation + ginseng group and the x-irradiation group (p = 0.009, Table 4).
Discussion
Radiotherapy widely used in the treatment of various forms of cancer can result in damage to surrounding tissue after application (De Ruysscher et al. 2019). Small intestinal injury is a severe complication capable of emerging following radiotherapy in abdominal and pelvic cancers (Lu et al. 2019). The present study represents the first investigation of the protective effect of ginseng in x-radiation-induced intestinal damage.
Small intestinal damage is a very widespread complication of radiotherapy, and the small intestine is one of the most radiosensitive organs. Monti et al. reported that intestinal mucosal damage was the principal determinant of survival in patients exposed to high-dose radiation (Monti et al. 2005).
Although the mechanism involved in intestinal damage stimulated by radiation is not yet fully understood, studies have shown that an increase in ROS is one of the most important causes of radiation-induced small intestinal damage (Keskek et al. 2006; Mercantepe et al. 2019). Previous studies have also shown that reduction and oxidation metabolism in cells changes as a response to ionizing radiation and that this results in radiation toxicity-related damage in healthy tissues (Yahyapour et al. 2018). ROS occurring in tissues affect antioxidant enzyme activity. A number of studies have shown that radiation causes an increase in MDA levels and a decrease in GSH (Yahyapour et al. 2018; Abou-Zeid et al. 2018). Consistent with previous research, single-dose 2 Gray x-radiation also produced changes in antioxidant enzyme activities in the present study by causing an increase in MDA and a decrease in GSH.
Radiation therapy generally led to irregularity in the morphological structure of the intestine in this study. Previous research has shown that the application of radiation triggers disturbance in the intestinal epithelium, villus fusions, and degeneration in villus structures, including hemorrhage (Elliott et al. 2014; El-Ghazaly et al. 2015). Consistent with previous studies, the application of 6 Gy radiation in the present research led to degeneration and losses in villus and crypt structures and also caused intestinal damage by triggering hemorrhage and vascular congestion. Studies have also shown that free radicals emerging after ionizing radiation lead to DNA damage and cell death (Leach et al. 2001). In agreement with prior research, x-radiation was also found to trigger apoptosis by causing an increase in caspase-3 positivity in small intestinal tissues in the present study (Poindexter et al. 2015; Orhon et al. 2016; Jalili-Firoozinezhad et al. 2018; Mercantepe et al. 2019).
Ginseng is employed as a therapeutic agent in the treatment of various diseases. Studies have shown that it possesses antibacterial, antiviral, antioxidant, and anti-inflammatory properties (Huang et al. 2017; Bai et al. 2018; Nguyen and Nguyen 2019). In addition to these activities, ginseng also exerts a regulatory effect on lipid peroxidation (Zhang et al. 2020). In the present study, the administration of ginseng was seen to cause a decrease in MDA activity and to play a role in the prevention of lipid peroxidation caused by x-irradiation. Additionally, ginseng can trigger improvements in antioxidant enzyme levels. Consistent with this research, previous studies have also reported that the application of ginseng led to a change in antioxidant enzyme levels by causing an increase in GSH activities (Mansour 2013; Xing et al. 2019).
Previous research has also shown that ginseng exhibits an antiapoptotic effect in various tissues (Na et al. 2012; Bai et al. 2018). In a study from 2020, Zhang et al. showed that ginseng pretreatment significantly improved cisplatin-induced apoptosis in the intestines (Zhang et al. 2020). Similarly in the present study, ginseng significantly prevented apoptosis by causing a decrease in caspase-3 activity resulting from x-irradiation.
There are also a number of limitations to this research. First, oxidative stress, MDA, and the antioxidant enzyme GSH were evaluated. This study therefore needs to be supported by research examining other oxidant/antioxidant enzymes and proteins. In addition, we determined apoptosis by means of cleaved caspase-3 antibody. Our apoptosis finding needs to be supported by studies examining the damage mechanism and mitochondrial Ca+2 levels.
In conclusion, the findings of this study showed that a single 6 Gy dose of x-irradiation caused lipid peroxidation in small intestine tissue and induced enterocyte loss by causing apoptosis in enterocytes. In addition, the application of KRG exhibited a protective role in intestinal damage caused by x-irradiation by suppressing apoptosis caused by x-irradiation and reducing caspase-3 activity and prevented oxidative stress by reducing antioxidant enzyme levels and reduced lipid peroxidation.
Availability of data and materials
All data are available upon request.
Code availability
Not applicable.
References
Abou-Zeid SM, El-Bialy BE, El-Borai NB et al (2018) Radioprotective effect of Date syrup on radiation-induced damage in Rats. Sci Rep. https://doi.org/10.1038/S41598-018-25586-3
Bai L, Gao J, Wei F et al (2018) Therapeutic potential of ginsenosides as an adjuvant treatment for diabetes. Front Pharmacol 9:1–14. https://doi.org/10.3389/fphar.2018.00423
Bellïes M, Gonzalo S, Serra N et al (2017) Environmental exposure to low-doses of ionizing radiation. Effects on early nephrotoxicity in mice. Environ Res 156:291–296. https://doi.org/10.1016/j.envres.2017.03.034
Broin PÓ, Vaitheesvaran B, Saha S et al (2015) NIH public access. Int J Radiat Oncol Biol Phys 91:360–367. https://doi.org/10.1016/j.ijrobp.2014.10.023.Intestinal
Cho HJ, Lee WH, HA HOM, et al (2017) Role of NADPH oxidase in radiation-induced pro-oxidative and pro-inflammatory pathways in mouse brain. Physiol Behav 176:139–148. https://doi.org/10.1080/09553002.2017.1377360.Role
De Ruysscher D, Niedermann G, Burnet NG et al (2019) Radiotherapy toxicity. Nat Rev Dis Prim. https://doi.org/10.1038/s41572-019-0064-5
Delaney G, Jacob S, Featherstone C, Barton M (2005) The role of radiotherapy in cancer treatment: Estimating optimal utilization from a review of evidence-based clinical guidelines. Cancer 104:1129–1137. https://doi.org/10.1002/cncr.21324
Draper HH, Hadley M (1990) Malondialdehyde determination as index of lipid Peroxidation. Methods Enzymol 186:421–431. https://doi.org/10.1016/0076-6879(90)86135-I
El-Ghazaly MA, El-Hazek RM, Khayyal MT (2015) Protective effect of the herbal preparation, STW 5, against intestinal damage induced by gamma radiation in rats. Int J Radiat Biol 91:150–156. https://doi.org/10.3109/09553002.2014.954059
Elliott TB, Deutz NE, Gulani J et al (2014) Gastrointestinal acute radiation syndrome in Göttingen minipigs (Sus Scrofa Domestica). Comp Med 64:456–463
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82:70–77
Huang Q, Wang T, Yang L, Wang HY (2017) Ginsenoside Rb2 alleviates hepatic lipid accumulation by restoring autophagy via induction of sirt1 and activation of AMPK. Int J Mol Sci 18:1–15. https://doi.org/10.3390/ijms18051063
Jalili-Firoozinezhad S, Prantil-Baun R, Jiang A et al (2018) Modeling radiation injury-induced cell death and countermeasure drug responses in a human Gut-on-a-Chip article. Cell Death Dis. https://doi.org/10.1038/s41419-018-0304-8
Jemal A, Bray F, Ferlay J (2011) Global Cancer Statistics: 2011. CA Cancer J Clin 61:69–90. https://doi.org/10.3322/caac.20107.Available
Keskek M, Gocmen E, Kilic M et al (2006) Increased expression of cyclooxygenase-2 (COX-2) in radiation-induced small bowel injury in rats. J Surg Res 135:76–84. https://doi.org/10.1016/j.jss.2006.03.031
Leach JK, Van TG, Lin P et al (2001) Ionizing radiation-induced, mitochondria-dependent generation of reactive oxygen. Nitrogen 1:3894–3901
Lee JH, Lee HJ, Yang M et al (2013) Effect of Korean Red Ginseng on radiation-induced bone loss in C3H/ HeN mice. J Ginseng Res 37:435–441. https://doi.org/10.5142/jgr.2013.37.435
Lu L, Li W, Chen L et al (2019) Radiation-induced intestinal damage: latest molecular and clinical developments. Futur Oncol 15:4105–4118. https://doi.org/10.2217/fon-2019-0416
Mansour HH (2013) Protective effect of ginseng against gamma-irradiation-induced oxidative stress and endothelial dysfunction in rats. EXCLI J 12:766–777
Mercantepe F, Topcu A, Rakici S et al (2019) The effects of N-acetylcysteine on radiotherapy-induced small intestinal damage in rats. Exp Biol Med 244:372–379. https://doi.org/10.1177/1535370219831225
Monti P, Wysocki J, van der Meeren A, Griffiths NM (2005) The contribution of radiation-induced injury to the gastrointestinal tract in the development of multi-organ dysfunction syndrome or failure. Br J Radiol Suppl. https://doi.org/10.1259/bjr/53186341
Na JY, Kim S, Song K et al (2012) Anti-apoptotic activity of ginsenoside Rb1 in hydrogen peroxide-treated chondrocytes: Stabilization of mitochondria and the inhibition of caspase-3. J Ginseng Res 36:242–247. https://doi.org/10.5142/jgr.2012.36.3.242
Nguyen NH, Nguyen CT (2019) Pharmacological effects of ginseng on infectious diseases. Inflammopharmacology 27:871–883. https://doi.org/10.1007/s10787-019-00630-4
Orhon ZN, Uzal C, Kanter M et al (2016) Protective effects of Nigella sativa on gamma radiation-induced jejunal mucosal damage in rats. Pathol Res Pract 212:437–443. https://doi.org/10.1016/j.prp.2016.02.017
Park SE, Park C, Kim SH et al (2009) Korean red ginseng extract induces apoptosis and decreases telomerase activity in human leukemia cells. J Ethnopharmacol 121:304–312. https://doi.org/10.1016/j.jep.2008.10.038
Park HM, Kim SJ, Kim JS, Kang HS (2012) Reactive oxygen species mediated ginsenoside Rg3- and Rh2-induced apoptosis in hepatoma cells through mitochondrial signaling pathways. Food Chem Toxicol 50:2736–2741. https://doi.org/10.1016/j.fct.2012.05.027
Poindexter SV, Reddy VK, Mittal MK et al (2015) Transcriptional corepressor MTG16 regulates small intestinal crypt proliferation and crypt regeneration after radiation-induced injury. Am J Physiol - Gastrointest Liver Physiol 308:G562–G571. https://doi.org/10.1152/ajpgi.00253.2014
Rakici SY, Guzel AI, Tumkaya L, Sevim Nalkiran H, Mercantepe T (2020) Pelvic radiation-induced testicular damage: an experimental study at 1 gray. Syst Biol Reprod Med 66:89–98. https://doi.org/10.1080/19396368.2019.1679909
Suman S, Kumar S, Moon BH et al (2017) Increased transgenerational intestinal tumorigenesis in offspring of ionizing radiation exposed parent APC1638N/+ mice. J Cancer 8:1769–1773. https://doi.org/10.7150/jca.17803
Ullah HMA, Lee YY, Kim M et al (2021) Red ginseng oil attenuates oxidative stress and offers protection against ultraviolet-ınduced photo toxicity. Oxid Med Cell Longev. https://doi.org/10.1155/2021/5538470
Uzal C, Sezer A, Usta U et al (2012) The protective effect of amifostine on radiation-induced proctitis: systemic versus topical application. Balkan Med J 29:32–38. https://doi.org/10.5152/balkanmedj.2011.005
Verma P, Jahan S, Kim TH, Goyal PK (2011) Management of radiation injuries by Panax ginseng extract. J Ginseng Res 35:261–271. https://doi.org/10.5142/jgr.2011.35.3.261
Xing J, jing, Hou J gang, Ma Z na, et al (2019) Ginsenoside Rb3 provides protective effects against cisplatin-induced nephrotoxicity via regulation of AMPK-/mTOR-mediated autophagy and inhibition of apoptosis in vitro and in vivo. Cell Prolif 52:1–16. https://doi.org/10.1111/cpr.12627
Xu X, Ling Q, Wei Q et al (2011) Korean Red Ginseng: a new approach for the treatment of graft-versus-host disease after liver transplantation. Transpl Proc 43:2651–2655. https://doi.org/10.1016/j.transproceed.2011.06.032
Yahyapour R, Motevaseli E, Rezaeyan A et al (2018) Reduction–oxidation (redox) system in radiation-induced normal tissue injury: molecular mechanisms and implications in radiation therapeutics. Clin Transl Oncol. https://doi.org/10.1007/s12094-017-1828-6
Zhang C, Ni J, Li BL et al (2013) CpG-oligodeoxynucleotide treatment protects against ıonizing radiation-ınduced ıntestine ınjury. PLoS ONE. https://doi.org/10.1371/journal.pone.0066586
Zhang JJ, Wang JQ, Xu XY et al (2020) Red ginseng protects against cisplatin-induced intestinal toxicity by inhibiting apoptosis and autophagy: via the PI3K/AKT and MAPK signaling pathways. Food Funct 11:4236–4248. https://doi.org/10.1039/d0fo00469c
Author information
Authors and Affiliations
Contributions
AO and LT designed the study. AO, LT, TM, TCS, MU, SK, GD and AP performed the experiments. TM and TCS performed the histopathological analysis. HKY and EYK performed the biochemical analysis. AO, LT, TM and TCS wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The animal experiments were performed in conformity with the laws and regulations for animal experiments in Helsinki Declarations and were approved by the Recep Tayyip Erdoğan University local animal care committee (Rize, Turkey, decision no. 2021/14 dated 27.05.2021). Experimental procedures were carried out following the directives for the care and use of laboratory animals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ozdemir, A., Tumkaya, L., Mercantepe, T. et al. The protective effects of ginseng on x-irradiation-induced intestinal damage in rats. Radiat Environ Biophys 62, 395–402 (2023). https://doi.org/10.1007/s00411-023-01039-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-023-01039-y