Abstract
This study aimed to investigate the effects of high-dose inhaled corticosteroids (ICS) on chronic cough patients with elevated fractional exhaled nitric oxide (FeNO) levels. In a prospective study, adults with chronic cough and FeNO ≥ 25 ppb, without any other apparent etiology, received fluticasone furoate (200 mcg) for three weeks. Outcomes were evaluated using FeNO levels, cough severity, and Leicester Cough Questionnaire (LCQ) before and after treatment. Of the fifty participants (average age: 58.4 years; 58% female), the treatment responder rate (≥ 1.3-point increase in LCQ) was 68%, with a significant improvement in cough and LCQ scores and FeNO levels post-treatment. However, improvements in cough did not significantly correlate with changes in FeNO levels. These findings support the guideline recommendations for a short-term ICS trial in adults with chronic cough and elevated FeNO levels, but the lack of correlations between FeNO levels and cough raises questions about their direct mechanistic link.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 (T2) airway inflammation is a major treatable trait in chronic airway diseases [1, 2]. Fractional exhaled nitric oxide (FeNO) serves as a non-invasive point-of-care test for T2 airway inflammation [3]. Given the technical challenges associated with induced sputum analysis, clinical management often relies on simpler and more feasible measurements, such as FeNO tests.
In the literature, a FeNO cutoff level of ≥ 25 parts per billion (ppb) has been suggested as a useful biomarker for diagnosing cough variant asthma (CVA) or eosinophilic bronchitis (EB), as well as for predicting a response to anti-inflammatory treatment in patients with chronic respiratory symptoms [4,5,6]. However, cough guideline recommendations have been conflicting regarding the use of FeNO measurement, due to a lack of robust evidence [1, 7]. A recent clinical statement by the British Thoracic Society suggested a FeNO level threshold of ≥ 25 ppb as guidance for considering a short-term trial of ICS in patients with cough who exhibit no other symptoms or airflow obstruction [8]. Despite these advances, a gap in clinical evidence persists regarding the ICS treatment based on the FeNO level.
In this background, we conducted a prospective study to investigate the efficacy of high-dose ICS in treating chronic cough. Our aim was to evaluate the response of cough to ICS treatment in patients with chronic cough and FeNO levels ≥ 25 ppb, but with no other apparent etiology, and to explore factors associated with a positive treatment response.
Methods
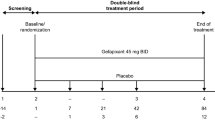
Study Participants and Design
The study was designed as a prospective, multi-center, single-arm study, aiming to investigate cough response to ICS. We recruited adult patients aged ≥ 19 years from referral clinics in South Korea. The inclusion criteria were as follows: (1) chronic cough as the chief complaint, (2) FeNO levels ≥ 25 ppb, (3) a forced expiratory volume in 1 s (FEV1)/forced volume vital capacity (FVC) ratio ≥ 70%, (4) normal chest radiography (or no clinically relevant findings), (5) no current symptom and sign suggestive of other cough etiologies, including fever, purulent sputum, heartburn, or acid regurgitation, (6) no recent history of cigarette smoking, (7) no recent use of angiotensin-converting enzyme inhibitors, (8) no exposure to corticosteroids or anti-leukotrienes within the past 2 weeks, and (9) no exposure to codeine or opiate anti-tussive medications within the past week.
The study participants were treated with a high-dose of fluticasone furoate (200 mcg) for 3 weeks (± 1 week). The treatment dose and duration were selected based on cough guidelines and systematic reviews [1, 9]. ICS adherence was calculated as dividing the used dose by the expected usage, which was presented as a percentage. At the baseline and follow-up visits (V1 and V2), the FeNO level was repeatedly measured using NIOX VERO® (Aerocrine, Solna, Sweden), and the cough status was assessed using patient-reported outcomes (PROs), including the Leicester Cough Questionnaire (LCQ), Cough Hypersensitivity Questionnaire (CHQ), and cough severity score (0–10). The institutional review board of all participating institutions approved the study protocols, which adhered to the principles stipulated in the Declaration of Helsinki. Written informed consent was obtained from all patients before study enrollment.
Outcomes
The primary outcome was the treatment response, which was defined as the proportion of patients achieving a minimal clinically important difference (MCID) of LCQ (> 1.3) [10]. The secondary outcome was the change of CHQ, cough severity, and FeNO levels between V1 and V2. The correlation between the FeNO level and PROs of cough status at baseline and post-treatment change were evaluated. The baseline clinical characteristics were assessed to identify the factors predicting the ICS treatment response.
Statistical Analysis
Parameters were compared using the Mann–Whitney test or Student’s t-test for continuous variables and the chi-square test for categorical variables. Paired t-test or Wilcoxon-signed rank tests were utilized to compare the post-treatment changes in FeNO levels and cough scores. Spearman’s correlation coefficient was calculated to quantify the correlation between FeNO levels and cough scores. The baseline characteristics associated with ICS treatment responders were assessed through a logistic regression analysis. A P value of < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS Statistics 25.0 (IBM Corp., Armonk, NY, USA).
Results
A total of 57 patients were recruited between January 2021 and December 2022. Seven patients were excluded due to follow-up loss, leaving 50 patients in the final study group (mean age: 58.4 ± 12.2 years; and female sex: 58.0%). The median FeNO levels was 37.5 ppb (IQR: 30–55 ppb). The mean LCQ scores were 13.5 ± 3.5. Compared to males, female subjects exhibited lower LCQ scores (12.6 ± 3.6 vs. 14.7 ± 3.0, P = 0.032) and higher cough severity scores (5.0 ± 2.0 vs. 4.0 ± 1.4, P = 0.025) at baseline. However, their FeNO levels were comparable [females, median: 37 ppb (IQR: 29–45 ppb) vs. males, median: 44 ppb (IQR: 32–59 ppb); P = 0.227; Table 1].
The mean duration of ICS treatment (between V1 and V2) was 25.6 ± 3.9 days, with a median treatment adherence rate of 100% (IQR: 90–100%). FeNO levels and cough PRO scores significantly improved following the treatment (Fig. 1A–D). The FeNO levels decreased from a median of 37.5 ppb (IQR: 30–55 ppb) at V1 to 22.0 ppb (IQR: 15–36 ppb) at V2 (P < 0.001). At V2, the FeNO levels were below 25 ppb in 54%. Daily cough severity scores from days 1 to 21 showed slow but steady improvements (Fig. 1E). Similar trends were observed in groups stratified by the median FeNO levels (37.5 ppb) (Fig. 1F).
Changes in FeNO levels (A) and scores for LCQ (B), CHQ (C), and cough severity (D) before (V1) and after treatment with inhaled corticosteroids (V2). Changes in daily cough severity scores from post-treatment days 1 to 21 in all patients (E) and in patients stratified by the median FeNO levels of 37.5 ppb (F). FeNO fractional exhaled nitric oxide, LCQ Leicester Cough Questionnaire, CHQ Cough Hypersensitivity Questionnaire
Spearman analyses revealed no correlation between baseline FeNO levels and LCQ scores (r = 0.063, P = 0.664), nor between post-treatment changes in FeNO levels and LCQ scores (r = − 0.282, P = 0.067).
In total, 68% (34/50) of patients were classified as ICS treatment responders, based on the MCID of the LCQ (> 1.3 increase); 52% showed improvement more than twice the MCID (> 2.6 increase), while 38% showed improvement more than three times the MCID (> 3.9 increase). According to the Patient Global Impression of Severity (PGI-S) scale analysis of post-treatment LCQ scores [11], 20% of patients had no cough (LCQ ≥ 19), and 42% had minimal-to-mild cough (16 ≤ LCQ < 19) at V2.
Baseline characteristics between ICS responders and non-responders (based on the MCID of the LCQ > 1.3 increase) are presented in Table 2. Responders were more often females (70.6% vs 31.1%, P = 0.020) and had lower pre-treatment LCQ scores (12.0 ± 2.9 vs 16.5 ± 2.5, P < 0.001) and higher cough severity scores (4.9 ± 2.0 vs 3.9 ± 1.1, P = 0.022) than non-responders.
Multivariate logistic regression analyses, adjusted for variables with a P value < 0.10 in univariate analyses presented in Table 2 (sex, smoking history, LCQ score, CHQ score, and cough severity score), indicated that female sex (adjusted odds ratio: 13.54, 95% confidence interval: 1.34–137.29; P = 0.027) and pre-treatment LCQ score (0.37, 0.19–0.72; P = 0.004) were significantly associated with ICS treatment response (LCQ > 1.3 increase; Table not shown). However, in another multivariate logistic regression analyzing a larger ICS response (defined by an increase in LCQ score of > 3.9), the associations were not significant for female sex (2.89, 0.48–17.37; P = 0.245) and pre-treatment LCQ score (0.74, 0.54–1.02; P = 0.063; table not shown).
Discussion
In the present study, we investigated the response of chronic cough patients with FeNO levels ≥ 25 ppb to high-dose ICS treatment, where patients had no other apparent etiology. After 3–4 weeks of treatment, the cough PRO scores and FeNO levels showed significant improvement. The treatment responder rate was 68%, based on the MCID of LCQ, and notably, 38% of the patients demonstrated a large treatment effect (more than three times the MCID). These findings support cough guideline recommendations for ICS trial, particularly in adults with chronic cough and elevated FeNO levels [1, 7, 8].
Daily measurements of cough severity scores were performed in our study. Overall, slow but steady improvements were observed following ICS treatment. The trend in cough improvement did not differ among groups stratified by a FeNO level of 37.5 ppb, suggesting that a longer maintenance treatment might provide further therapeutic benefits.
The mechanistic link between nitric oxide and cough remains uncertain [3]. We did not find a significant correlation between FeNO levels and cough scores, both at baseline and after treatment. Similar findings were reported in a study involving patients with CVA, where cough severity score was not correlated with FeNO levels [12]. The lack of correlation between cough severity and FeNO levels suggests their indirect mechanistic relationships. We speculate that eosinophils play a more direct role in sensitizing the cough reflex than nitric oxide does, and the observed effects of ICS treatment on cough might occur through the overall suppression of T2 inflammatory pathways, including those involving eosinophils. The regulatory mechanism of FeNO levels, which is mainly influenced by interleukin (IL)-4 and IL-13, is distinct from that of eosinophils, which are regulated by IL-5 [3].
An interesting finding from our study is the positive association between ICS treatment response and female sex. This association remained significant after adjusting for confounders, including pre-treatment LCQ scores. However, a regression to the mean effect, which is common in chronic respiratory conditions [13], should be also considered. Consequently, our analysis of treatment response should be viewed as exploratory. Among patients with chronic cough, female sex has been linked to increased cough reflex sensitivity and poorer health-related QoL [14, 15]. Additionally, female sex was associated with a better treatment response to codeine in patients with refractory chronic cough [16]. Given these observations, it is tempting to speculate that female sex might serve as a predictor of a better early treatment response, or alternatively, act as a confounder in observational studies of treatment effects. Studies on pain suggested that women might benefit more from interventions, although the findings varied depending on the type of treatment [17].
The present study has several limitations. Firstly, it is a prospective observational study with a single-arm intervention, raising the possibility of regression to the mean or placebo effects. Secondly, our study was conducted in research setting with relatively strict selection criteria, including recent medication exposure, to minimize confounding effects on FeNO levels. Therefore, our findings should be interpreted within this specific clinical context. Thirdly, our sample size was relatively small. During recruitment, we found that more than half of the patients with chronic cough and FeNO levels ≥ 25 ppb presented with one or more indicators of other etiologies, such as abnormal chest X-ray or spirometry results, or additional symptoms. Fourthly, objective cough outcomes were not utilized. Finally, we did not differentiate between CVA and EB using methacholine challenge tests. Although ICS response may vary with airway hyper-responsiveness, we minimized potential confounding by including only patients without airflow obstruction (FEV1/FVC ratio ≥ 0.70). Furthermore, the utility of bronchial challenge tests in predicting ICS treatment response remains unclear in patients with isolated chronic cough (without dyspnea or wheezing) [18, 19].
In conclusion, our findings suggest that the majority of patients with chronic cough and FeNO levels of ≥ 25 ppb may benefit from a high-dose ICS treatment within 4 weeks. Further studies are warranted to validate the role of FeNO measurement in the long-term management of chronic cough.
References
Morice AH, Millqvist E, Bieksiene K et al (2020) ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J 55(1):1901136
Chung KF, McGarvey L, Song WJ, Chang AB, Lai K, Canning BJ, Birring SS, Smith JA, Mazzone SB (2022) Cough hypersensitivity and chronic cough. Nat Rev Dis Primers 8(1):45
Lee JH, Lee JH, Park SY, Koskela HO, Song WJ (2023) Is fractional exhaled nitric oxide a treatable trait in chronic cough: a narrative review. J Thorac Dis 15(10):5844–5855
Song WJ, Kim HJ, Shim JS et al (2017) Diagnostic accuracy of fractional exhaled nitric oxide measurement in predicting cough-variant asthma and eosinophilic bronchitis in adults with chronic cough: a systematic review and meta-analysis. J Allergy Clin Immunol 140(3):701–709
Sutherland L, Shaw K, Parrish C, Singleton N, McKeever TM, Stewart I, Shaw D, Martin MJ, Harrison T (2021) A low exhaled nitric oxide level excludes a short-term benefit from inhaled corticosteroids in suspected asthma: a randomized placebo-controlled trial. Respirology 26(7):666–672
Ambrosino P, Accardo M, Mosella M, Papa A, Fuschillo S, Spedicato GA, Motta A, Maniscalco M (2021) Performance of fractional exhaled nitric oxide in predicting response to inhaled corticosteroids in chronic cough: a meta-analysis. Ann Med 53(1):1659–1672
Song DJ, Song WJ, Kwon JW et al (2018) KAAACI evidence-based clinical practice guidelines for chronic cough in adults and children in Korea. Allergy Asthma Immunol Res 10(6):591–613
Parker SM, Smith JA, Birring SS et al (2023) British Thoracic Society Clinical Statement on chronic cough in adults. Thorax 78(Suppl 6):s3–s19
Lee SE, Lee JH, Kim HJ, Lee BJ, Cho SH, Price D, Morice AH, Song WJ (2019) Inhaled corticosteroids and placebo treatment effects in adult patients with cough: a systematic review and meta-analysis. Allergy Asthma Immunol Res 11(6):856–870
Raj AA, Pavord DI, Birring SS (2009) Clinical cough IV: what is the minimal important difference for the Leicester Cough Questionnaire? Handb Exp Pharmacol 187:311–320
Rhatigan K, Hirons B, Kesavan H, Turner RD, Ebelthite C, Hull JH, Jolley CJ, Birring SS, Cho PSP (2023) Patient global impression of severity scale in chronic cough: validation and formulation of symptom severity categories. J Allergy Clin Immunol Pract 11(12):3706–3712
Lai K, Zhan W, Wu F et al (2021) Clinical and inflammatory characteristics of the Chinese APAC cough variant asthma cohort. Front Med (Lausanne) 8:807385
Lee Y, Lee JH, Park SY, Lee JH, Kim JH, Kim HJ, Kim SH, Chung KF, Song WJ (2023) Roles of real-world evidence in severe asthma treatment: challenges and opportunities. ERJ Open Res 9(2):00248–02022
Morice AH, Jakes AD, Faruqi S et al (2014) A worldwide survey of chronic cough: a manifestation of enhanced somatosensory response. Eur Respir J 44(5):1149–1155
Kang N, Won HK, Lee JH et al (2023) Health-related quality of life and its determinants in chronic cough: the Korean chronic cough registry study. Allergy Asthma Immunol Res 15(3):348–360
Oh JY, Kang SY, Kang N, Won HK, Jo EJ, Lee SE, Lee JH, Shim JS, Kim YC, Yoo Y (2024) Characterization of codeine treatment responders among patients with refractory or unexplained chronic cough: a prospective real-world cohort study. Lung 202(2):97–106
Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd (2009) Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain 10(5):447–485
Rytilä P, Ghaly L, Varghese S, Chung W, Selroos O, Haahtela T (2008) Treatment with inhaled steroids in patients with symptoms suggestive of asthma but with normal lung function. Eur Respir J 32(4):989–996
Ponsioen BP, Hop WC, Vermue NA, Dekhuijzen PN, Bohnen AM (2005) Efficacy of fluticasone on cough: a randomised controlled trial. Eur Respir J 25(1):147–152
Funding
This study was supported by a grant from the Korean Academy of Asthma, Allergy and Clinical Immunology. The grantor had no role in the study design, data collection, analysis, result interpretation, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Consortia
Contributions
SHK, BJL, and WJS contributed to the study design. JHL, SYK, and WJS wrote the main manuscript text and prepared figure 1. IY, JYO, JHL, SYP, MHK, EJJ, JYM, and SHK contributed to the data collection. KEP was responsible for the statistical analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interest
WJS declares grants from Merck Sharp & Dohme Corp. and AstraZeneca, consulting fees from Merck, AstraZeneca, Shionogi, Bellus, and GSK, and lecture fees from Merck, AstraZeneca, GSK, Sanofi, and Novartis. Other authors declare that no conflicts of interest exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, JH., Kang, SY., Yu, I. et al. Cough Response to High-Dose Inhaled Corticosteroids in Patients with Chronic Cough and Fractional Exhaled Nitric Oxide Levels ≥ 25 ppb: A Prospective Study. Lung 202, 275–280 (2024). https://doi.org/10.1007/s00408-024-00698-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-024-00698-y