Abstract
Purpose
We performed a retrospective analysis of a sarcoidosis cohort who had sACE obtained at their initial clinic visit, but the treating physician was blinded to the results. We examined the relationship between sACE and the treating physician’s decision to escalate sarcoidosis treatment.
Methods
Treatment was considered escalated if the prednisone dose was increased or if the prednisone dose was not changed but an additional anti-sarcoidosis drug was added or the dose was increased.
Results
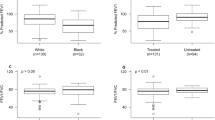
561 sarcoidosis patients were analyzed. The most common target organ was the lung (84%). Using a cut-off of > 82 units/L for an elevated sACE, 31/82 (38%) with an elevated sACE had treatment escalation whereas 91/497 (18%) had treatment escalation with a normal sACE (p < 0.0001). For the need of treatment escalation, a sACE (cut-off of > 82) had sensitivity 0.25, specificity 0.89, positive predictive value 0.38, negative predictive value 0.81. These results were not appreciably different using other sACE cut-off values such as 70, 80, 90, or 100. A multivariable logistic regression model that included demographics, the target organ, spirometry results estimated that sACE level and lower FVC were significantly associated with the likelihood of treatment escalation. These findings held when sACE > 82 replaced sACE level in the multivariable logistic regression model.
Conclusions
Although there was a strong correlation between sACE at the initial sarcoidosis clinic visit and subsequent treatment escalation of sarcoidosis, the predictive power was such that sACE is not adequately reliable to be used in isolation to make this determination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiotensin converting enzyme (ACE) is a carboxypeptidase enzyme that converts angiotensin I into angiotensin II [1]. ACE is produced by the epithelioid cell within the sarcoid granuloma [2, 3], and serum ACE levels (sACE) are thought to correlate with the granuloma burden of the disease [3]. Over the past several decades, there has been controversy concerning the clinical usefulness of sACE. The reliability of ACE as a biomarker of active sarcoidosis has been questioned [4], as sACE is neither perfectly sensitive or specific for the disease [4]. Furthermore, sACE is affected by genetic polymorphisms, variation in assays, and the effects of medications including ACE-inhibitors and anti-sarcoidosis drugs [4]. Even if sACE is a reliable measure of sarcoidosis disease activity, such activity does not necessarily mandate sarcoidosis treatment [5]. Nevertheless, the relationship between sACE and the need for sarcoidosis treatment has not been rigorously evaluated. We performed a retrospective analysis of a large cohort of sarcoidosis patients seen for an initial visit at a university medical center sarcoidosis clinic. All patients had sACE obtained on the day of their initial visits, but the treating physician was blinded to the results. We examined the relationship between sACE and the treating physician’s decision to escalate sarcoidosis treatment at this initial visit.
Methods
This study was approved by the Albany Medical Center Institutional Review Board (study number 6272). This is a retrospective analysis of data obtained for clinical purposes. These data were collected in real time in an institution-approved sarcoidosis clinical database. All patients were analyzed who had a diagnosis of sarcoidosis based by established international criteria [6] and had their initial visit at Albany Medical Center for the care of sarcoidosis with one of the authors (MAJ) between February 2013 and September 2021. The following data were collected on all patients for this analysis included: (a) demographics (sex, self-designated race); (b) age at sarcoidosis diagnosis, (c) age at their initial clinic visit; (d) the specific organs that were treated or were being considered for treatment by the clinician described as "the target organ(s)”; (e) anti-sarcoidosis medications currently prescribed at the time of the initial visit. These medications included corticosteroids, antimetabolites, anti-malarials, tumor necrosis factor antagonists, and other systemic immunosuppressive treatments; (f) sACE levels obtained within 24 h of first visit. The sACE levels were not available to the treating physician for at least 48 h after the initial clinic visit, and therefore the clinician was “blinded” to the sACE results when treatment decisions were made; (g) the clinician’s decision to escalate or not escalate anti-sarcoidosis treatment. It should be noted that it is routine policy that all sarcoidosis patients initially seen undergo sACE testing; no patients are excluded from testing. Treatment was considered to be escalated if the corticosteroid dose was increased or if the corticosteroid dose was not changed but an additional anti-sarcoidosis drug was added or increased. All other medication changes and no changes in anti-sarcoidosis medications were considered not to be treatment escalations; (h) % predicted forced vital capacity (FVC) and forced expiratory volume in 1 s (FEV1) at the initial clinic visit as determined by Hankinson and colleagues [7]; (i) for those patients who returned for a second visit, the clinician routinely subjectively evaluated change in the target organ in real time using the following qualitative 5-point system—improved, worse, no change, could not reliably assess change, resolved. The serum ACE test was performed through Labcorp (Burlington, North Carolina USA) and is an activity (kinetic) test where the normal range is considered 14 to 82 units/L.
The primary goal of these analyses was to explore the relationship between the sarcoidosis patient’s sACE level at the initial clinic visit and the treating physician’s decision to escalate or not escalate treatment. We used demographic and clinical information in multivariable models as covariates for adjustment.
Statistical Methods
All cases with no sACE value available were excluded from the analysis. Descriptive statistics (means, standard deviation, or proportion) were used to summarize the characteristics of patients. Test of significance was performed in both treatment and no treatment subgroups. Chi-square test was used to examine the relationship between ACE levels (dichotomized using various cutoff values), the need for treatment, and treatment outcomes. Sensitivity, specificity, and positive and negative predictive values were estimated at different ACE cut-off values to determine the predictive power of the sACE level on treatment escalation. Logistic regression models adjusted for age, sex, race, duration of the disease, sACE level, and target organs to predict the probability of escalating or not escalating treatment. A p value < 0.05 was considered statistically significant. All statistical analyses were performed using SAS version 9.4.
Results
This analysis was performed in 561 consecutive sarcoidosis patients who met the study entry criteria. Table 1 shows the baseline demographics, clinical features and sACE levels of these patients. The patients were predominantly white (83%) and there were slightly more females (55%) than males. Mean spirometric values were in the low-normal range, and the duration of disease was quite scattered with a median of less than 2 years and a mean of 7 years. Table 2 shows the target organs (organs that required treatment). The most common target organ was the lung at nearly 84%, with no other single organ requiring treatment in more than 14% of the patients.
Table 3 compares the corticosteroid doses at the initial clinic visit. Corticosteroids were most common medications used, and all analyses were performed using prednisone dose equivalents. One hundred and forty-four of 561 patients (26%) were receiving corticosteroids. Fifty-seven (10%) were receiving a non-corticosteroid agent for sarcoidosis at their initial clinic visit. In those receiving corticosteroids at their initial visit, the mean daily dose of prednisone was approximately 20 mg.
Table 4 shows the relationship between an elevated ACE level > 82 (units/liter) and the decision to escalate treatment. There was a strong positive association (p < 0.0001) between these variables. In terms of the predictive power of a sACE level of > 82 to determine dose escalation, the sensitivity was 25.4%, specificity 88.3%, positive predictive value 37.8%, and negative predictive value 81.0%. In addition, we used alternative cutoff values for sACE of > 70, > 80, > 90, and > 100 (Table e1). In terms of the predictive power of sACE to determine dose escalation at these different cutoffs, the sensitivities were progressively lower and the specificities were progressively higher as the ACE cutoff was raised. At the cutoff of sACE > 100, the sensitivity was 17.2%, specificity 93.2%, positive predictive value 41.2%, and negative predictive value 80.2%. Although a sarcoidosis patient sACE level of > 100 is likely to need treatment escalation, the low sensitivity suggests that this will not occur in many patients.
Table 5 shows the results of a multivariable logistic regression estimating the association of sACE level and several clinical variables with treatment escalation. Only sACE level and a low FVC % predicted at the initial clinic visit were significantly associated with treatment escalation. In Table 6, a similar multivariable logistic regression was performed where a dichotomous variable was used for the sACE level: > 82 versus ≤ 82. The results of this analysis were very similar to that in Table 5: only the sACE > 82 and a low FVC % predicted were associated with treatment escalation.
Table 7 shows association between treatment escalation at the initial visit and the clinician’s assessment of improvement or no improvement at the subsequent visit (506/579, 87.6% had a subsequent clinic visit). There was a strong association (p < 0.001) between these variables.
We performed all of the above analyses in the subgroup of 385 patients who were “treatment naïve” (not receiving any sarcoidosis treatment at their initial visit, and all the aforementioned results of the entire cohort held with this subgroup, Tables e2–e5). The only additional association found in this subgroup was that the multivariate logistic regressions (both with a dichotomous and continuous sACE level) found an association between the skin as a target organ and the need to escalate treatment.
Discussion
In this retrospective analysis of 561 sarcoidosis patients seen for an initial visit at a university sarcoidosis clinic, there was a strong association between an elevated sACE level and the clinician’s decision to escalate sarcoidosis treatment. Despite this strong association, the sensitivity (25.4%), specificity (88.3%), positive and negative predictive value (37.8% and 81%) were inadequate for an elevated sACE level to be used in isolation to make treatment decisions. Similar findings were observed when this analysis was restricted to patients who were not receiving any anti-sarcoidosis treatment initially. In a multivariable logistic regression, demographic characteristics, duration of disease, and target organ did not significantly affect these results. Similar findings were also observed when the cutoff value for an elevated sACE level was raised to > 100, where although the specificity of the association between sACE and treatment escalation increased to 93.1%, the positive predictive value was only 41.2%. These data suggest that although an elevated serum ACE is supportive evidence that treatment of sarcoidosis should be escalated, such decision needs to be augmented by other clinical data. In the multivariable logistic regression analysis, a low FVC % predicted was associated with treatment escalation. As the lung was the overwhelmingly most common target organ for treatment, we suspect that the low FVC % predicted was an indicator of active pulmonary sarcoidosis that warranted treatment. These results were not significantly affected by whether the patient was treatment naive at the time that a sACE level was obtained.
The use of sACE as a measure of sarcoidosis activity and the need for treatment is controversial. The sACE level has been shown to correlate with the overall disease activity, total body granuloma burden, and total number of extrapulmonary organs involved [8,9,10,11]. Serial sACE measurements have been suggested to be useful to assess the clinical course of disease [12,13,14]. However, others have found that the sACE level does not correlate with the severity of alveolitis in pulmonary sarcoidosis [15], the initial sACE level does not reliably predict progression of pulmonary sarcoidosis [5, 16] and sACE is not a reliable predictor of corticosteroid responsiveness for pulmonary sarcoidosis [17,18,19,20]. The recent European Respiratory Society clinical practice guidelines on the treatment of sarcoidosis did not mention the use of sACE or any other serum biomarker as useful in making treatment decisions. [21]
This analysis has several limitations. First and foremost, the decision to escalate treatment was not determined by protocol but by the subjective determination of a single clinician (MAJ). Although this individual is experienced in the treatment of sarcoidosis, his approach may not be optimal and might be prone to personal subjective assumptions. To account for the subjective nature of the decision to treat these patients, all patients who returned for a follow-up clinic visit were assessed for improvement or lack of improvement of their condition. This analysis showed a strong correlation between treatment escalation and improvement in the target organ, suggesting that treatment was indicated. This method of assessment is routine in this clinic and was not performed for study purposes. However, it is possible that the clinician’s assessment of improvement was influenced by his previous decision to escalate treatment. Clearly, the limitation of a single clinician determining the need for treatment escalation could only be resolved by duplicating this study with the participation of multiple clinicians. A second limitation was that this analysis was performed on sarcoidosis patients in one medical center, and the results may not reliably extend universally. However, our cohort was demographically diverse, and in a multivariate logistic analysis, there was no significant effect of demographics upon the study results. Thirdly, sACE is affected by many factors including the use of angiotensin converting enzyme inhibitor drugs, the specific sACE assay, and the status of the patient’s ACE gene deletion/insertion polymorphism genotype [4]. Although we used the same sACE assay for these patients, we did not control for these other factors. Finally, the patients were also diverse in terms of their clinical course of sarcoidosis, with some patients having their initial clinic visit soon after diagnosis whereas others had chronic disease and had an initial clinic visit several years after diagnosis. However, in the multivariate logistic regression analysis, the duration of disease did not affect the relationship between sACE level and treatment escalation.
In conclusion, our retrospective analysis of patients with an initial visit in one university sarcoidosis clinic found a strong correlation between the sACE level and the clinician’s decision to escalate therapy. The clinician was blinded to the sACE result when the treatment decision was made. However, despite this strong association, the predictive power of the sACE level to determine the need for treatment escalation was inadequate to be used in isolation. The sACE level may possibly be useful as adjunctive data that could be used in combination with other clinical information to make treatment decisions. It is also possible that other promising serum biomarkers such as serum IL2-receptor [22], chitotriosidase [23], or Krebs von den Lungen-6 (KL-6) [24] may be helpful in determining the need to treat sarcoidosis.
References
Shen XZ, Billet S, Lin C et al (2011) The carboxypeptidase ACE shapes the MHC class I peptide repertoire. Nat Immunol 12(11):1078–1085
Sheffield EA (1997) Pathology of sarcoidosis. Clin Chest Med 18(4):741–754
Lynch JP 3rd, Kazerooni EA, Gay SE (1997) Pulmonary sarcoidosis. Clin Chest Med 18(4):755–785
Chopra A, Kalkanis A, Judson MA (2016) Biomarkers in sarcoidosis. Expert Rev Clin Immunol 12(11):1191–1208
Finkel R, Teirstein AS, Levine R, Brown LK, Miller A (1986) Pulmonary function tests, serum angiotensin-converting enzyme levels, and clinical findings as prognostic indicators in sarcoidosis. Ann N Y Acad Sci 465:665–671
Crouser ED, Maier LA, Wilson KC et al (2020) Diagnosis and detection of sarcoidosis: an official american thoracic society clinical practice guideline. Am J Respir Crit Care Med 201(8):e26–e51
Hankinson JL, Odencrantz JR, Fedan KB (1999) Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med 159(1):179–187
Klech H, Kohn H, Kummer F, Mostbeck A (1982) Assessment of activity in sarcoidosis: sensitivity and specificity of 67Gallium scintigraphy, serum ACE levels, chest roentgenography, and blood lymphocyte subpopulations. Chest 82(6):732–738
Selroos OB (1984) Value of biochemical markers in serum for determination of disease activity in sarcoidosis. Sarcoidosis 1(1):45–49
Selroos OB (1986) Biochemical markers in sarcoidosis. Crit Rev Clin Lab Sci 24(3):185–216
Teirstein AS, Judson MA, Baughman RP, Rossman MD, Yeager H Jr, Moller DR (2005) The spectrum of biopsy sites for the diagnosis of sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 22(2):139–146
Vorselaars AD, van Moorsel CH, Zanen P et al (2015) ACE and sIL-2R correlate with lung function improvement in sarcoidosis during methotrexate therapy. Respir Med 109(2):279–285
Lieberman J, Sastre A (1980) Serum angiotensin-converting enzyme: elevations in diabetes mellitus. Ann Intern Med 93(6):825–826
DeRemee RA, Rohrbach MS (1980) Serum angiotensin-converting enzyme activity in evaluating the clinical course of sarcoidosis. Ann Intern Med 92(3):361–365
Cohen RD, Bunting PS, Meindok HO, Chamberlain DW, Rebuck AS (1985) Does serum angiotensin converting enzyme reflect intensity of alveolitis in sarcoidosis? Thorax 40(7):497–500
Rust M, Bergmann L, Kuhn T et al (1985) Prognostic value of chest radiograph, serum-angiotensin-converting enzyme and T helper cell count in blood and in bronchoalveolar lavage of patients with pulmonary sarcoidosis. Respir Int Rev Thoracic Dis 48(3):231–236
Baughman RP, Fernandez M, Bosken CH, Mantil J, Hurtubise P (1984) Comparison of gallium-67 scanning, bronchoalveolar lavage, and serum angiotensin-converting enzyme levels in pulmonary sarcoidosis: predicting response to therapy. Am Rev Respir Dis 129(5):676–681
Baughman RP, Ploysongsang Y, Roberts RD, Srivastava L (1983) Effects of sarcoid and steroids on angiotensin-converting enzyme. Am Rev Respir Dis 128(4):631–633
Snider GL (1985) Prediction of therapeutic response in steroid-treated pulmonary sarcoidosis. Am Rev Respir Dis 132(5):1139–1140
Hollinger WM, Staton GW Jr, Fajman WA, Gilman MJ, Pine JR, Check IJ (1985) Prediction of therapeutic response in steroid-treated pulmonary sarcoidosis: evaluation of clinical parameters, bronchoalveolar lavage, gallium-67 lung scanning, and serum angiotensin-converting enzyme levels. Am Rev Respir Dis 132(1):65–69
Baughman RP, Valeyre D, Korsten P et al (2021) ERS clinical practice guidelines on treatment of sarcoidosis. Eur Respir J 58(6):158
Kobayashi Y, Sato T, Nagai T et al (2021) Association of high serum soluble interleukin 2 receptor levels with risk of adverse events in cardiac sarcoidosis. ESC Heart Fail 8(6):5282–5292
Bennett D, Cameli P, Lanzarone N et al (2020) Chitotriosidase: a biomarker of activity and severity in patients with sarcoidosis. Respir Res 21(1):6
Bergantini L, Bianchi F, Cameli P et al (2019) Prognostic biomarkers of sarcoidosis: a comparative study of serum chitotriosidase, ACE, lysozyme, and KL-6. Dis Markers 2019:8565423
Acknowledgements
The authors wish to acknowledge Sooyeon-Kwon, PhD for her assistance with manuscript tables and her guidance.
Funding
There was no funding for this research.
Author information
Authors and Affiliations
Contributions
BS: Assisted in study design, data collection, writing and editing of the manuscript. RS: Statistical analysis, writing and editing the manuscript. MS: Data collection, writing and editing the manuscript. GK: Data collection, writing and editing the manuscript. SG: Data collection, writing and editing the manuscript. GK: Data collection, writing and editing the manuscript. ASP: Data collection, writing and editing the manuscript. GK: Data collection, writing and editing the manuscript. KMF: Assisted with data management and statistical analysis. RD: Assisted with data management and statistical analysis. RY: Statistical analysis, writing and editing the manuscript. MAJ: Study design; data collection, assisted in statistical analysis, writing and editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MAJ: Consultant for Prometheus; Star Therapeutics; has received grants for his institution from Mallinckrodt, aTyr Pharmaceuticals, and Foundation for Sarcoidosis Research. No other author has any competing interests.
Ethical Approval
This study was approved by the Albany Medical Center Institutional Review Board (study number 6272).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shkolnik, B., Sore, R., Salick, M. et al. The Relationship Between Serum Angiotensin Converting Enzyme Level and the Decision to Escalate Treatment of Sarcoidosis. Lung 201, 381–386 (2023). https://doi.org/10.1007/s00408-023-00629-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-023-00629-3