Abstract
Introduction
People with chronic obstructive pulmonary disease (COPD) present high prevalence of physical inactivity that leads to a negative effect on health-related quality of life (HRQoL). The present study investigated COPD phenotypes according to their levels of physical activity and sedentary behaviour, as well as body composition and skeletal muscle strength.
Methods
This is an observational and cross-sectional study. Anthropometric data and COPD clinical control were collected and all participants underwent assessments of lung function, HRQoL, dyspnoea, levels of physical activity and sedentary behaviour, body composition and skeletal muscle strength. Participants were classified using hierarchical cluster analysis. Age, dyspnoea and obstruction (ADO) index was used to determine prognosis and calculated for each cluster.
Results
One hundred and fifty-two participants were included. Three distinct phenotypes were identified. Participants in phenotype 1 were more physically active, less sedentary and had better body composition and lower ADO index (p < 0.0001 for all variables). Overall, participants in phenotypes 2 and 3 were less physically active, more sedentary having a higher ADO index. However, participants in phenotype 2 were older, whereas participants in phenotype 3 had worse HRQoL, clinical control and body composition. Lung function did not differ across the three phenotypes.
Conclusions
Our results show that physical activity, sedentary behaviour and body composition should be considered to determine phenotypes in people with COPD and are involved in the prognosis of the disease. Less sedentary patients have better prognosis while age, body composition and clinical control seems to differentiate physically inactive patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is considered a complex heterogeneous syndrome, having both pulmonary and extrapulmonary features [1, 2]. The increased interest in better understanding the determinants of the COPD heterogeneity is leading to the investigation of COPD phenotypes. The phenotype is defined as the structural and functional organism, and determined by the genotype and modulated by the environment [3]. The COPD phenotype is defined as “a single or combination of disease attributes that describe differences between individuals with COPD as they relate to clinically meaningful outcomes” (i.e. symptoms, exacerbations, hospitalization or death) [2].
Several authors have described COPD phenotypes [4,5,6,7,8,9]. In people with COPD, it is well established that loss of muscle mass and reduced body mass index are related to worsening health status and high mortality rates [10]. Therefore, it is reasonable to consider both muscle strength and body composition when investigating different phenotypes in this population. Despite the relevance of the phenotypes, few studies have investigated COPD phenotypes in people from developing countries or considered physical activity as a variable to determine COPD phenotypes [11, 12].
The benefits of increased physical activity in people with COPD are well established [13, 14], and increasing physical activity has been included as a recommendation in the guidelines for the clinical management in the population [1]. In addition to physical activity, recent literature has highlighted the importance of investigating time spent in sedentary behaviour in people with COPD [15, 16]. Physical activity and sedentary behaviour are multifactorial spectrums of activity influenced by as exercise capacity, depression symptoms, ethnicity, education level and socioeconomic status [17,18,19]. For instance, the difference in the levels of physical activity between people with COPD from Brazil and Central Europe has been mainly attributed to socioeconomic status [20].
Physical activity, sedentary behaviour, skeletal muscle strength and body composition are important for people with COPD; however, there is a lack of data on COPD phenotypes that have taken these outcomes into account. The aim of this study was to investigate different phenotypes of people with COPD according to their levels of physical activity and sedentary behaviour, as well as skeletal muscle strength and body composition.
Participants and Methods
Study Design and Participants
This is an observational and cross-sectional study. This study was approved by the Ethics Review Board of the Clinical Hospital of the Faculty of Medicine at the University of Sao Paulo (protocol 569.243). Participants with COPD were screened and recruited in an outpatient clinic of a tertiary University Hospital between February 2014 and December 2015. The inclusion criteria were as follows: COPD diagnosed according to the GOLD [1], who were clinically stable (i.e. without exacerbations for at least 30 days). The exclusion criteria were the following: continuous use of oxygen therapy, musculoskeletal or other chronic lung diseases and current participation in a programme of supervised exercise training.
On the first assessment day, anthropometric data and clinical history were collected and participants performed spirometry. In addition, information was obtained on clinical control [Clinical Control Questionnaire (CCQ), health-related quality of life (HRQoL) Chronic Respiratory Questionnaire (CRQ)] and functional limitation resulting from dyspnoea [modified Medical Research Council scale (mMRC)]. Participants were also given an accelerometer (Actigraph GT3X+) to be worn over 6 days. After that, participants patients returned the accelerometer and initiated a second assessment day, during which measures were collected of quadriceps muscle strength (dynamometer) and body composition (octapolar bioimpedance).
Outcomes and outcome measures
Pulmonary function the tests were performed according to the American Thoracic Society and European Respiratory Society (ATS/ERS) recommendations [21]. FVC and FEV1 were expressed as both absolute values and as a percent of the predicted value for the Brazilian population [22].
Functional limitation resulting from dyspnoea was assessed using the mMRC [23]. The scale is a valid method, recommended by the GOLD and validated in Brazilian Portuguese [24].
Health-related quality of life was assessed using the CRQ,[25]. This questionnaire is validated in Brazilian Portuguese and a self-reported measure of HRQoL shown to be valid and reliable in patients with COPD. Higher scores indicate better HRQoL [26].
COPD clinical control was measured by the CCQ [27]. This is validated in Brazilian Portuguese, valid, reliable and responsive instrument used to detect clinical changes in people with COPD. A higher score represents poorer clinical control [28].
Physical activity and sedentary behaviour were quantified with a triaxial accelerometer; the ActiGraph model GT3X (Health One Technology, Fort Walton Beach, FL), which has been shown to be an accurate instrument to measure physical activity in people with COPD [29]. Participants were asked to wear the device on their waist for six consecutive days, during waking hours. They were also instructed to remove it only during showering and swimming activities.
Skeletal muscle isometric strength was measured in the quadriceps femoral of the dominant leg using a digital dynamometer (Gauge® Force, FG-100 kg model). The results were expressed in kilogram–force (kg–f) and as a percentage of predicted value in a healthy population [30].
Body composition body mass index (BMI, kg/m2) was assessed according to procedures described by Lohman et al. [31] Body composition was analysed using octapolar tactile bioelectrical impedance analysis (InBody720 - Biospace, Seoul, South Korea) [32, 33].
Age, dyspnoea and obstruction index the prognosis of the participants was evaluated by the ADO index [34]. Higher ADO values indicate a worse prognosis.
Statistical Analysis
Data were analysed using the Statistical Package for Social Sciences (SPSS) version 18.0 for Windows (SPSS Inc, Chicago, USA).
Principal component analysis (PCA) was used to correct the correlations between variables. The Kaiser–Meyer–Olkin (KMO) measure of sampling adequacy test and Bartlett’s Test of Sphericity were used to confirm whether the PCA was appropriate for these variables.
Cluster analysis the cluster analysis was performed using the six components identified in the PCA. A hierarchical cluster analysis was used to identify the number of clusters and cluster centroids. Possible cluster divisions were determined by inconsistent jumps between stages in an agglomeration schedule. Once cluster numbers and centroids were decided, a K-means cluster analysis was used to cluster cases to centroids. To test for the stability of clusters, K-means clustering was repeated with a random sample containing 50% of the cases [35, 36].
Between-cluster differences the comparison between cluster was tested by one-way analysis of variance followed by Tukey’s multiple comparison test and Kruskal–Wallis test followed by Dunn’s multiple comparison test according to normality. A P value < 0.05 was considered statistically significant.
Results
In total, 311 participants were screened, of whom, 178 met the inclusion criteria. Of the 178 participants included in the study, 26 (11%) did not complete all assessments, despite all the attempts. Therefore, 152 participants completed the study.
Characteristics of the participants the characteristics of the 152 participants are shown in Table 1. Levels of physical activity and sedentary behaviour as well as quadriceps muscle strength and body composition are presented in Table 2.
Components identified in PCA the KMO (0.74) and Bartlett’s Test of Sphericity (p < 0.001) confirmed that the analysis was appropriate for these variables. Six components were identified in this study, and each component encompassed some variables (Table 3).
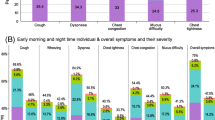
Identification and characterisation of COPD phenotypes Ward’s cluster analysis was based on the significant components identified by the PCA. Participants in phenotype 1 (n = 61) had median [interquartile range; IQR] age of 65 (60–70) years and moderate to severe airflow obstruction. Compared to participants in phenotypes 2 and 3, phenotype 1 was more physically active (p < 0.0001), less sedentary (p < 0.0001), and presented with higher skeletal muscle mass (SMM; % total body-weight) (p < 0.0001) (Table 4) and better ADO index score (p < 0.0001) (Fig. 1). Phenotype 1 can be defined as the “Younger and more active” phenotype.
Participants in phenotype 2 (n = 60) were older than those in the other two phenotypes [median (IQR) age of 73 (68–78) years; p < 0.0001] (Table 4) and presented moderate to severe airflow obstruction. Compared to participants in phenotypes 1 and 3, phenotype 2 presented better HRQoL (emotional, self-control and total score of the CRQ; p < 0.0001 for all) (Table 4). Phenotype 2 was defined as the “Older and more inactive” phenotype.
Participants in phenotype 3 (n = 31) had a median [IQR] age of 63 (60–69) years and presented severe to very severe airflow obstruction. Compared to participants in phenotypes 1 and 2, phenotype 3 presented worse HRQoL (dyspnoea, fatigue, self-control and total score of the CRQ; p < 0.0001 for all), clinical control (p < 0.0001) and more functional limitation resulting from dyspnoea (p < 0.0001) (Table 4). Regarding body composition, the proportion of participants in phenotype 3 with a BMI ≥ 25 kg/m2 was significantly greater than the proportion in phenotypes 1 and 2 (p = 0.001) (Table 4). Phenotype 3 was defined as the “Younger and more inactive” phenotype.
Discussion
The present study identified three distinct groups of people with COPD in terms of physical activity, sedentary behaviour, body composition and quadriceps muscle strength. Phenotype 1 (“Younger and more active” phenotype) included people with COPD who were younger than those in phenotype 2, and, in general, were more physically active, with greater percentage of SMM, lesser fat mass and presented with a better disease prognosis as measured by the ADO index. Compared to phenotype 1, participants in phenotypes 2 (“Older and more inactive” phenotype) and 3 (“Younger and more inactive” phenotype) were less physically active, spent more time in sedentary behaviour and had worse disease prognosis. Of note, participants in phenotype 2 were older and reported a better HRQoL.
Physical inactivity is common in people with COPD and it has been associated with poorer outcomes, independent of the degree of airway obstruction [37]. Notwithstanding these associations, only one previous study objectively measured physical activity or sedentary behaviour to define COPD phenotypes [38]. However, that study did not take into account other important variables that are related to physical activity, such as comorbidities, percentage of lean and fat mass, muscle strength, HRQoL and clinical control of the disease [39,40,41]. Participants in phenotype 1 had a greater daily step count than the cut-off to be a considered an active COPD patient (i.e. 4580 steps/day) [42]. Further, compared to phenotypes 2 and 3, participants in phenotype 1 spent more time in MVPA and less time in sedentary behaviour. These results place phenotype 1 in a position of better potential benefit, as there is evidence supporting the health benefits of participating in MVPA in healthy people [42, 43]. In addition, there is evidence demonstrating longer survival in people with COPD who are less sedentary [44,45,46]. Participants in phenotype 1 also presented with less functional limitation resulting from dyspnoea and better HRQoL, clinical control and percentage of skeletal muscle mass (SMM). These findings are in agreement with previous findings that suggested a strong association between levels of physical activity and HRQoL [46] and SMM [47, 48].
Participants in phenotypes 1 and 3 had similar age and airway obstruction. However, those in phenotype 1 performed 3186 steps/day more than those in phenotype 3. Importantly, this difference in daily steps is likely to be considered clinically significant (i.e. > 600 steps/day) [43]. A difference in body composition between phenotypes 1 and 3 was also observed. That is, phenotype 3 presented with lower percentage of SMM, fat-free mass (FFM) and higher fat mass. Of note, reduced lean body mass [49] and obesity [50, 51] have been demonstrated to contribute to physical inactivity in COPD patients. Therefore, it appears that phenotype 3 is characterized by a vicious cycle, which includes physical inactivity, worse body composition and worse health status [17].
Phenotype 2 was represented by older and more inactive people with COPD. It is expected that older people are more inactive than younger people [52, 53]. However, the finding of the present study that was not expected was that the “Older and more inactive” phenotype would present with better HRQoL than the other two phenotypes. A possible explanation for this finding may be that, compared to younger people, older people with chronic disease can have better perceived HRQoL [54]. Despite being older and having similar levels of physical activity as phenotype 3, participants in phenotype 2 presented with higher percentage of SMM and lower fat mass. The present study is cross-sectional, and thus, cannot establish a causality between body composition and HRQoL. However, there is evidence suggesting a positive association between body composition and HRQoL [55]. Overall, our results may suggest that the more positive perception of HRQoL in phenotype 2 participants is probably due to the fact they were older and had a better body composition.
Participants in phenotype 3 had similar levels of physical (in)activity than those in phenotype 2. However, compared to participants in phenotypes 1 and 2, phenotype 3 presented worse HRQoL and clinical control as well as more dyspnoea and lower percentage of SMM and FFM. There is evidence suggesting that dyspnoea, age, and HRQoL are predictors of physical performance in people with COPD [15]. For instance, Katajisto et al. demonstrated that the perception of breathlessness was a barrier for daily life physical activities in patients with COPD [56]. Additionally, higher dyspnoea symptoms have been associated with lower levels of physical activity in patients with COPD [57]. Interestingly, Cheni et al. suggest that COPD patients with more symptoms represent a distinct clinic phenotype [58].
Obesity can also interfere in the physical activity levels. Monteiro et al. demonstrated that obese people with COPD had lower levels of physical activity than those who were underweight or normal-weight [50]. In our study, the proportion of patients who were overweight or obese in phenotype 3 was significantly higher than the proportion in the other two phenotypes. We also observed a higher number of women in the phenotype 3; however, we do not consider that the difference in body composition observed between phenotypes is related to gender, because we did not observe difference in the free fat mass index that takes the gender in consideration.
HRQoL is also likely to explain the lower physical activity levels observed in phenotype 3. This hypothesis can be supported by the findings of Patel et al. showing that health status is a predictor of daily physical activity [12]. Then, it is possible that the phenotype 3 is less active due to a complex association between the health-related and the psychosocial and the COPD symptoms [59]. For instance, Oga et al. demonstrated that dyspnoea symptoms and HRQoL are associated with anxiety and depression symptoms in COPD patients [60]. Additionally, lower levels of physical activity were associated with higher risk for anxiety and depression symptoms [61]. As a consequence, the phenotype 3 might require a motivational programme to become more active and they also could benefit for an improvement in the fat mass loss and reduction of symptoms.
Unexpectedly, a difference in quadriceps muscle strength among the phenotypes described in the present study was not observed. This is likely to have occurred due to the use of an equation to predict quadriceps muscle strength was not developed for the Brazilian population [30]. The FEV1 was not also different across the three phenotypes despite have been considered the main marker of severity in COPD [1].
However, the disease prognosis as measured by the ADO index was significantly different across the phenotypes. The two most inactive phenotypes (phenotypes 2 and 3) presented with a worse disease prognosis. These findings confirm that, even when pulmonary function is similar across groups of people with COPD, heterogeneity can still be present [62]. Also, reinforce the need to investigate different phenotypes according to other characteristics.
Clinical implications the characteristics of the phenotypes identified in the present study, provide substantial information for the development of treatment strategies for people with COPD. Patients from all phenotypes seem to require an intervention to become more active or to remain active and to remain as quiet as possible in sedentary behaviour, but the peculiarities of each group should be considered. For instance, patients from the phenotype 1 need to maintain their levels of physical activity. On the other hand, patients from the phenotypes 2 and 3 need to improve their physical activity levels; however, it seems that the strategies in both phenotypes should be different. In phenotype 2, the age effect should be considered while in phenotype 3 the body composition and clinical control seem more important. Changes in physical activity and sedentary behaviour are difficult, so further studies are necessary.
Limitations
The present study had some limitations. Participants were recruited from an outpatient clinic in a tertiary University Hospital what may explain the higher proportion of more severe COPD patients. A cross-sectional study design does not allow to establish a cause-effect relationship; however, these results may provide direction for future longitudinal studies to evaluate a causal effect in more detail.
Conclusions
The present study demonstrated different phenotypes in people with COPD according to their levels of physical activity and sedentary behaviour. The results have practical implications for the management of people with COPD and future studies should consider the peculiarities of each phenotype for the development of strategies to change the physical activity and sedentary behaviour in this population.
References
GOLD (Global Initiative for Chronic Obstructive Lung Disease). Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. GOLD. 2016
Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL et al (2010) Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med 182(5):598–604
Rice JP, Saccone NL, Rasmussen E (2001) Definition of the phenotypes. Adv Genet 42:69–76
Langel P, Halpin DM, O’Donnell D, MacNee W (2016) Diagnosis, assessment, and phenotyping of COPD: beyond FEV1. Int J Chron Obstruct Pulmon Dis 11:3–12
Garcia-Aymerich J, Agustí A, Barberà JA, Belda J, Farrero E, Ferrer A, Ferrer J et al (2009) Phenotypic heterogeneity of chronic obstructive pulmonary disease. Arch Bronconeumol 45(3):129–138
Burgel PR, Paillasseur JL, Caillaud D, Tillie-Leblond I, Chanez P, Escamilla R et al (2010) Clinical COPD phenotypes: a novel approach using principal component and cluster analyses. Eur Respir J 36(3):531–539
Burgel PR, Paillasseur JL, Peene B, Dusser D, Roche N, Coolen J et al (2012) Two distinct chronic obstructive pulmonary disease (COPD) phenotypes are associated with high risk of mortality. PLoS ONE 7(12):e51048
Agustí A, Edwards LD, Rennard SI, MacNee W, Tal-Singer R, Miller BE et al (2012) Persistent systemic inflammation is associated with poor clinical outcomes in COPD: a novel phenotype. PLoS ONE 7(5):e37483
Tse HN, Tseng CZ, Wong KY, Ng LY, Lai TL, Yee KS (2016) Frequent Exacerbator: the phenotype at risk of depressive symptoms in geriatric COPD patients. Lung 194(4):665–673
Marquis K, Debigare R, Lacasse Y, LeBlanc P, Jobin J, Carrier G (2002) et.al. Midthigh muscle cross-sectional area is a better predictor of mortality than body mass index in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 166(6):809–813
Koblizek V, Milenkovic B, Barczyk A, Tkacova R, Somfay A, Zykov K et al (2017) Phenotypes of COPD patients with a smoking history in Central and Eastern Europe: the POPE Study. Eur Respir J 11(5):1601446
Patel MS, Mohan D, Andersson YM, Baz M, Samantha Kon SC, Canavan JL et al (2014) Phenotypic characteristics associated with reduced short physical performance battery score in COPD. Chest 145(5):1016–1024
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM et al (2011) American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 43(7):1334–1359
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC et al (2007) Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 116(9):1094–1105
Hill K, Gardiner PA, Cavalheri V, Jenkins SC, Healy GN (2015) Physical activity and sedentary behavior: applying lessons to chronic obstructive pulmonary disease. Intern Med J 45(5):474–482
Cavalheri V, Straker L, Gucciardi DF, Gardiner PA, Hill K (2016 Apr) Changing physical activity and sedentary behaviour in people with COPD. Respirology 21(3):419–426
Bourbeau J (2009) Activities of life: the COPD patient. COPD 6(3):192–200
Marshall SJ, Jones DA, Ainsworth BE, Reis JP, Levy SS, Macera CA (2007) Race/ethnicity, social class, and leisure-time physical inactivity. Med Sci Sports Exerc 39(1):44–51
Parks SE, Housemann RA, Brownson RC (2003) Differential correlates of physical activity in urban and rural adults of various socioeconomic backgrounds in the United States. J Epidemiol Commun Health 57(1):29–35
Pitta F, Breyer MK, Hernandes NA, Teixeira D, Sant’Anna TJ, Fontana AD et al (2009) Comparison of daily physical activity between COPD patients from Central Europe and South America. Respir Med 103(3):421–426
Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F et al (2005) Standardisation of the measurement of lung volumes. Eur Respir J 26(3):511–522
Pereira CA, Sato T, Rodrigues SC (2007) New reference values for forced spirometry in white adults in Brazil. Braz J Pulmonol 33(4):397–406
Kovelis D, Segretti NO, Probst VS, Lareau SC, Brunetto AF, Pitta F (2008) Validation of the Modified Pulmonary Functional Status and Dyspnea Questionnaire and the Medical Research Council scale for use in Brazilian patients with chronic obstructive pulmonary disease. J Bras Pneumol 34(12):1008–1018
GOLD (Global initiative for chronic Obstructive Lung Disease). Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. GOLD; 2013
Williams JE, Singh SJ, Sewell L, Guyatt GH, Morgan MD (2001) Development of a self-reported Chronic Respiratory Questionnaire (CRQ-SR). Thorax 56(12):954–959
Moreira GL, Pitta FO, Ramos D, Nascimento CC, Barzon D, Kovelis D et al (2009) Versão em português do Chronic Respiratory Questionnaire: estudo da validade e reprodutibilidade. J Bras Pneumol 35(8):737–744
Van der Molen T, Willemse BW, Schokker S, ten Hacken NH, Postma DS, Juniper EF et al (2003) Development, validity and responsiveness of the clinical COPD questionnaire. Health Qual Life Outcomes 28:1–13
Silva LCS. Validação do questionário clínico de doença pulmonar obstrutiva crônica (CCQ) para a língua portuguesa. Dissertação de mestrado 2012; 1–98
Van Remoortel H, Raste Y, Louvaris Z, Giavedoni S, Burtin C, Langer D et al (2012) Validity of six activity monitors in chronic obstructive pulmonary disease: a comparison with indirect calorimetry. PLoS ONE 7:e39198
Hogrel J-Y, Payan C, Ollivier G, Tanant V, Attarian S, Couillandre A et al (2007) Development of a french isometric strength normative database for adults using quantitative muscle testing. Arch Phys Med Rehabil 88(10):1289–1297
Lohman TG, Roche AF, Martorell R. (1988) Anthropometric standardization reference manual. Human Kinetics, Champaign
Gibson AL, Holmes JC, Desautels RL, Edmonds L, Nuudi L (2008) Ability of new octapolar bioimpedance spectroscopy analyzers to predict 4-component-model percentage body fat in Hispanic, black, and white adults. Am J Clin Nutr 87(2):332–338
Cunningham JJ (1991) Body composition as a determinant of energy expenditure: a synthetic review and a proposed general prediction equation. Am J Clin Nutr 54(6):963–969
Riet G. Antó JM. Agustí AG et al (2009) Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet 374(9691):704–1152 ter
Clatworthy J, Hankins M, Buick D, Weinman J, Horne J (2007) Cluster analysis in illness perceptions research: a Monte Carlo study to identify the most appropriate method. Psychol Health 22(2):123–142
Harrison SL, Robertson N, Graham CD, Williams J, Steiner MC, Morgan MD et al (2014) Can we identify patients with different illness schema following an acute exacerbation of COPD: a cluster analysis. Respir Med 108(2):319–328
Watz H, Pitta F, Carolyn L, Garcia-Aymerich J, ZuWallack R, Troosters T et al (2014) An official European Respiratory Society statement on physical activity in COPD. Eur Respir J 44(6):1521–1537
Mesquita R, Spina G, Pitta F, Donaire-Gonzalez D, Deering BM, Patel MS et al (2017) Physical activity patterns and clusters in 1001 patients with COPD. Chronic Respiratory Disease 14(3):256–269
Yoshimura K, Sato S, Muro S, Yamada M, Hasegawa K, Kiyokawa H et al (2018) Interdependence of physical inactivity, loss of muscle mass and low dietary intake: Extrapulmonary manifestations in older chronic obstructive pulmonary disease patients. Geriatr Gerontol Int 18(1):88–94
Mantoani LC, Dell’Era S, MacNee W, Rabinovich RA (2017) Physical activity in patients with COPD: the impact of comorbidities. Expert Rev Respir Med 11(9):685–698
Duenas-Espín I, Demeyer H, Gimeno-Santos H, Polkey MI, Hopkinson NS, Rabinovich RA et al (2016) Depression symptoms reduce physical activity in COPD patients: a prospective multicenter study. Int J Chron Obstruct Pulmon Dis 10(11):1287–1295
Depew Z, Novotny P, Benzo R (2012) How many steps are enough to avoid severe physical inactivity in patients with chronic obstructive pulmonary disease? Respirology 17(6):1026–1027
Demeyer H, Burtin C, Hornikx M, Camillo CA, Van Remoortel H, Langer D et al (2016) The minimal important difference in physical activity in patients with COPD. PLos One 11(4):1–11
O’Donovan G, Blazevich AJ, Boreham C, Cooper AR, Crank H, Ekelund U et al (2010) The ABC of Physical Activity for Health: a consensus statement from the British Association of Sport and Exercise Sciences. J Sports Sci 28(6):573–591
Kushi LH, Doyle C, McCullough M, Rock CL, Demark-Wahnefried W, Bandera EV et al (2012) American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin 62(1):30–67
Waschki B, Kirsten AM, Holz O, Mueller KC, Schaper M, Sack AL et al (2015) Disease progression and changes in physical activity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 192(3):295–306
Esteban C, Arostegui I, Aburto M, Moraza J, Quintana JM, Aizpiri S et al (2014) Influence of changes in physical activity on frequency of hospitalization in chronic obstructive pulmonary disease. Respirology 19(3):330–338
Miravitlles M, Cantoni J, Naberan K (2014) Factors associated with a low level of physical activity in patients with Chronic Obstructive Pulmonary Disease. Lung 192(2):259–265
Gurgun A, Deniz S, Argin M, Karapolat H et al (2013) Effects of nutritional supplementation combined with conventional pulmonary rehabilitation in muscle-wasted chronic obstructive pulmonary disease: A prospective, randomized and controlled study. Respirology 18(3):495–500
Monteiro F, Camillo CA, Vitorasso R, Sant’Anna T, Hernandes NA, Probst VS et al (2012) Obesity and physical activity in the daily life of patients with COPD. Lung 190(4):403–410
Vozoris NT, O’Donnell DE (2012) Prevalence, risk factors, activity limitation and health care utilization of an obese, population-based sample with chronic obstructive pulmonary disease. Can Respir J 19(3):18–24
Centers for disease control and prevention (CDC) (2003) Prevalence of physical activity, including lifestyle activities among adults United States, 2000–2001. MMWR Morb Mortal Wkly Rep 15(52):764–769
Tsukino M, Nishimura K, Ikeda A, Koyama H, Mishima M, Izumi T et al (1996) Physiologic factors that determine the health-related quality of life in patients with COPD. Chest 110(4):896–903
Laudański K, Nowak Z, Niemczyk S (2013) Age-related differences in the quality of life in end-stage renal disease in patients enrolled in hemodialysis or continuous peritoneal dialysis. Med Sci Monit 19:378–385
Jones PW (2001) Health status measurement in chronic obstructive pulmonary disease. Thorax 56(11):880–887
Katajisto M, Kupiainen H, Rantanen P, Lindqvist A, Kilpeläinen M, Tikkanen H et al (2012) Physical inactivity in COPD and increased patient perception of dyspnea. Int J Chron Obstruct Pulmon Dis 7:743–755
Watz H, Waschki B, Meyer T, Magnussen H (2009) Physical activity in patients with COPD. Eur Respir J 33(2):262–272
Chen C, Wang L, Ou C, Lee C, Lin C, Hsiue T (2014) Using cluster analysis to identify phenotypes and validation of mortality in men with COPD. Lung 192(6):889–896
Lopes A, Xavier R, Caporali A, Stelmach R, Fernandes F, Harrison S, Carvalho C (2018) Identifying COPD patients at risk for worse symptoms, HRQoL, and self-efficacy: a cluster analysis. Chronic Illness 1:1742395317753883
Oga T, Tsukino M, Hajiro T, Ikeda A, Nishimura K (2012) Analysis of longitudinal changes in dyspnea of patients with chronic obstructive pulmonary disease: an observational study. Respir Res 13(1):85
Yu T, Ter Riet G, Puhan MA, Frei A et al (2017) Physical activity and risk of comorbidities in patients with chronic obstructive pulmonary disease: a cohort study. NPJ Prim Care Respir Med 18(1):27 36.
Carolan BJ, Sutherland R (2013) Clinical phenotypes of chronic obstructive pulmonary disease and asthma:Recent advances. JAllergy Clin Immunol 131(3):627–634
Funding
Funding was provided by Fundação de Amparo à Pesquisa do Estado de São Paulo with Grant No. 2013/20676-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report having no real or perceived conflicts of interest.
Rights and permissions
About this article
Cite this article
Xavier, R.F., Pereira, A.C.A.C., Lopes, A.C. et al. Identification of Phenotypes in People with COPD: Influence of Physical Activity, Sedentary Behaviour, Body Composition and Skeletal Muscle Strength. Lung 197, 37–45 (2019). https://doi.org/10.1007/s00408-018-0177-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-018-0177-8