Abstract
Objectives
To compare characteristics of patients readmitted after discharge by chronic obstructive pulmonary disease (COPD) exacerbation with those who were not readmitted and to identify factors associated with readmission risk.
Patients and Methods
We randomly selected a group of 40 COPD patients with high frequency of readmissions (HFR), who had ≥ 2 admissions by COPD exacerbation within 30 days after the last admission in 2015, and another group of 40 COPD patients with low frequency of readmissions (LFR), with 0–1 admissions in that period.
Results
Patients of the HFR group, compared to those in LFR group, were more frequently males (p = 0.009), older (p = 0.022), had a higher degree of dyspnea (p = 0.044), worse lung function (p = 0.049), belonged more frequently to exacerbator emphysema phenotype (p < 0.001), and had a higher frequency of diabetes (p = 0.049). The variables independently associated with increased risk of HFR were sex (OR 0.06, 95% CI 0.01–0.63, in women in relation to males), exacerbator emphysema phenotype (OR 28.61, 95% CI 3.59 compared to non-exacerbator phenotype), complications during hospitalization (OR 0.09, 95% CI 0.01–0.62, compared with those without complications), destabilized heart failure (OR 5.25, 95% CI 1.11–24.75, compared to those who did not), and length of hospital stay (OR 0.79, 95% CI 0.65–0.95, per day).
Conclusions
Chronic obstructive pulmonary disease patients with HFR are more frequently male, older, have worse dyspnea, lower lung function, belong more frequent to exacerbator emphysema phenotype, and more frequently diabetics. The variables that continued to be independent predictors of HFR in the multivariate analysis were sex, phenotype, occurrence of complications during admission, destabilized heart failure, and length of hospital stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by a decrease in airflow, not completely reversible, usually progressive and associated with an inflammatory response of the lung to toxic particles and gases, especially to tobacco smoke [1]. It is a disease with a high prevalence. According to data from the EPI-SCAN study, 10.2% of the general population in Spain between 40 and 80 years of age suffer COPD [2]. It is currently the fourth leading cause of death in the world, but is predicted to be the third leading cause in the year 2020 [1].
In the hospital setting, it is frequent to request care for patients with exacerbation of COPD. Even in many cases, it occurs after a recent hospitalization. The hospitalizations for this disease generate a high health resources use, being able to cause a decrease of the quality of life related to the health, an increase of the mortality and frequent readmissions [3,4,5,6]. In fact, it has been shown that the risks of hospitalization and death were significantly higher following discharge for COPD compared to the general population [7]. In this sense, it has been previously reported that, at 3 months after discharge due to an exacerbation, the overall mortality rate exceeds 10%, with the probability of readmissions being 20% per month and 35% at 3 months, in most cases due to respiratory causes [3, 8, 9]. The most frequent causes of death in patients with mild COPD are cardiovascular disease and lung cancer, whereas when the disease is more severe, the main cause of death is the evolution of the disease itself [10].
The objectives of this study were to compare the characteristics of the patients who required hospitalization within 30 days after a discharge due to exacerbation of COPD during the year 2015 with those who were not readmitted after hospital discharge in that period of time; to identify factors associated with readmission after discharge due to an exacerbation of COPD; and to determine the characteristics of the patient with COPD presenting a high risk of readmission.
Patients and Methods
Patients and Study Design
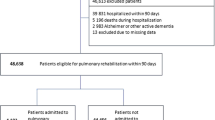
Patients with a COPD exacerbation admission during the year 2015 in the University General Hospital Gregorio Marañón (Madrid, Spain) were collected from the Spanish minimum basic dataset, which compiles clinical and personal information from patients at the moment of discharge. During 2015, we identified 1114 episodes of admission due to COPD exacerbation in the hospital, according with any of the COPD codes (ICD-9 CM) from Spanish minimum basic dataset (excluding acute bronchitis). These episodes correspond to 59 patients with two or more readmissions during the year and 775 patients with one readmission or none. By simple random sampling, of them, we selected a group of 40 COPD patients who had had in 2015 two or more admissions due to a COPD exacerbation within 30 days of the previous discharge (high frequency of readmission group, from this point forward, HFR). Concurrently, we randomly selected another group of 40 COPD patients with one or no readmission due to COPD exacerbation within 30 days of the last discharge (low frequency of readmission group, from this point forward, LFR). These sample sizes are obtained for an estimated difference in percentages of patients with an exacerbator phenotype (emphysema or chronic bronchitis) of 55% in HFR group versus 25% in LHR group (COPD phenotype according to the Spanish COPD guide—GesEPOC [2]), to achieve 80% power for a 95% confidence level. Once the two groups of patients were settled, clinical data from the patients and their admissions were collected retrospectively following a questionnaire designed ad hoc after reviewing the existing literature. Data retrieved from the clinical records included basic data (sex, age), smoking status, vaccine administration, degree of dyspnea, baseline spirometry parameters (forced expiratory volume in 1 s—FEV1, forced vital capacity—FVC), COPD phenotype according to the Spanish COPD guide (GesEPOC) [2], comorbidities (including Charlson Comorbidity Index—CCI), number of admissions by COPD exacerbation in the last year, arterial blood gas and symptoms at admission, length of hospital stay, complications during hospitalization, and treatment (both pharmacological and non-pharmacological) prescribed following discharge. After hospital discharge, we recorded the number of readmissions in less than 30 days in the same year, as well as the diagnosis, the length of hospital stay, and the mortality during readmissions.
Statistical Methods
Descriptive statistics were used to describe the study population. Data are presented as mean ± SD for quantitative variables or as number and percentage for categorical variables. First, univariate analysis was performed to determine the association between the variables and the outcome (frequency of readmissions). The associations with categorical variables were assessed by means of the Chi-square test while the t Student test or the Wilcoxon rank-sum test were used to evaluate the association with quantitative continuous variables. Later, an exploratory assessment of predictors of high frequency of readmission was conducted through a logistic regression model with the forward method in terms of the likelihood ratio, where the dependent variable was to be either from the HFR or the LFR. Variables were initially included if they had a significance of < 0.20 in the univariate analysis. Variables eventually remained in the final model if they were significantly associated, considering as significant p values < 0.05.
Secondly we described the characteristics of subsequent hospitalizations of the HFR group of patients. Finally, a further characterization of patients in a high risk of readmission was performed. For this purpose, only the variables that remained in the final logistic regression model were considered. In the first model (A), those patients who met the characteristics of these variables were described. In the subsequent models (B, C, D), the variable with lower statistical significance from was progressively removed. Stata® version 14 was used for the statistical analyses.
Ethics
Data were treated with full confidentiality, according to the Spanish legislation. Patient identifiers were deleted before the database was provided to the authors in order to keep strict patient confidentiality. It is not possible to identify patients at individual level either in this paper or in the database. Given the anonymous and mandatory nature of the data, informed consent was not required or necessary. The Spanish Ministry of Health previously evaluated this type of research and considered that it met all ethical aspects according to the Spanish legislation and so provided us the anonymous database. For all previous reasons, the requirement for ethical approval was not necessary.
Results
Patient Characteristics
The mean age of the patients was 75.8 ± 10.7 years and most of them (85%) were men. Eighty percent of the patients were former smokers. In relation to previous vaccinations, 75% of patients had received influenza vaccine in the last year and 78.75% had been vaccinated against pneumococcus (Table 1), most of them (76.25%) with the polysaccharide vaccine. The most frequent degree of dyspnea was 3 and the mean FEV1 was 53.4 ± 19,7%. The most frequent phenotype was non-exacerbator (47.5%), followed by exacerbator emphysema (20%), exacerbator chronic bronchitis (13.75%), and mixed phenotype (2.5%). The average of hospitalizations during the last 12 months was 2.1 ± 2.3 admissions. The mean Charlson Comorbidity Index was 3.9 ± 2.8 (Table 1). Among the associated comorbidities, hypertension was the most prevalent (73.75%), followed by dyslipidemia (51.25%) and diabetes (30%) (Table 2).
Characteristics of patients during admission are shown in Table 3. The most common symptom referred at the arrival at the emergency department was increased dyspnea (93.75%). The most frequent reason for admission was respiratory infection (78.75%). During admission 37.5% of the patients suffered from destabilization of any chronic disease, heart failure being the most frequent (25%). In addition, 21.25% of the patients also had some complications, highlighting pneumonia as the most frequent (10%).
Risk Factors for High Frequency of Readmission
The percentage of men in the HFR group was higher than in the LFR group (p = 0.012). With regard to age, patients of the LFR group were on average 5.3 years younger than those in HFR group (p = 0.024). Regarding spirometric parameters, there were differences for FEV1 (p = 0.049), being higher in the LFR group. As expected for the phenotype, there was a higher percentage of non-exacerbators (72.5%) in the LFR group (p < 0.001), while HFR patients had a higher degree of dyspnea (p = 0.044) (Table 1).
In relation to associated comorbidities (Table 2), significant differences were found for diabetes (p = 0.049), as well as for mild liver disease (p = 0.040). The length of hospital stay was not significantly different between the two groups. However, there was a significant difference (p = 0.006) in the number of hospitalizations in the last year, with a higher number of admissions in the HFR group. Regarding previous vaccination, there were no significant differences in the state of vaccination against influenza and pneumococcus between the two groups.
The only difference concerning symptoms was the presence of rest dyspnea (p = 0.002), more frequent in the HFR group. HFR patients also suffered from heart failure destabilization during hospitalization more frequently than LFR (p = 0.009). With regard to the treatment prescribed on discharge, there were significant differences for oral corticosteroids (p = 0.048), prescribed in 80% of patients of the HFR group compared with 55% in those of the LFR group (Table 3).
The multivariate analysis showed that the variables that continued to be independent predictors of HFR (p < 0.05) were phenotype, occurrence of complications during admission, sex, duration of stay, and destabilized heart failure (Table 4). Patients with exacerbator emphysema phenotype had a 28-fold greater risk of belonging to the HFR group than those with non-exacerbator phenotype (OR 28.61, 95% CI 3.59–227.98). Patients who had suffered a complication during hospitalization had a 91% lower risk of belonging to the HFR group compared to those who did not had complications (OR 0.09, 95% CI 0.01–0.62). With respect to sex, women had a 94% lower risk of belong to HFR group than men (OR 0.06, 95% CI 0.01–0.63). Taking into account the duration of initial admission, for each day of hospitalization, the risk of belong to HFR group decreased by 21% (OR 0.79, 95% CI 0.65–0.95). Those patients who presented with destabilized heart failure had a risk of belonging to the HFR group five times higher than those without heart failure (OR 5.25, 95% CI 1.11–24.75).
HFR Readmissions Characteristics
Patient of the HFR group (n = 40) had a mean of four readmissions in 2015 after baseline admission (rank 2–10), with a mean of 2.3 admissions within the following 30 days of the last hospital discharge (rank 1–8). The mean duration of these readmissions was 8.3 days (range 1–50). Seven of the patients (17.5%) died during one of the readmissions. Among the causes of readmission, COPD exacerbation was the most frequent (96.5%), followed by pneumonia and heart failure (24.7%) and respiratory infection (22.5%).
Characteristics of Patients in High Risk of Readmission
Based on the results of multivariable analysis, we proceeded to describe the characteristics of the COPD patients in high risk of readmission (Table 5). Model A describes the characteristics of a male patient, exacerbator emphysema phenotype, with a length of hospital stay in the initial admission lower than the mean (8.2 days), without complications during hospitalization and with destabilized heart failure, who were the most at risk of readmission (n = 2). After removing exacerbator emphysema phenotype as a predictive variable (Model B), the characteristics of patients with a high risk of readmission (n = 8) were quite similar to the previously described. The main differences were that these patients had a higher mean age and FEV1/FVC ratio, an increased Comorbidity Index, and more admissions during the last year. Along the same lines, after excluding heart failure (model C), the characteristics of these patients (n = 24) were also quite similar to patients from the previous model except that they were younger and had slightly higher Charlson Comorbidity Index, and lower prevalence of diabetes, obesity, and sleep apnea. Finally, keeping only the characteristics of being male and the absence of complications as risk factors (n = 33) (model D), the patients profile was quite similar to model C, except for a lower age but higher Charlson Comorbidity Index.
Discussion
In our study, we observed that patients who were readmitted during the month following discharge by COPD exacerbation, compared with those who were not readmitted during that period, were more frequently males, had older age, worse degree of dyspnea, lower FEV1, belonged more frequently to exacerbator emphysema phenotype, and they had a higher frequency of diabetes. Other studies have also demonstrated an increased risk of readmission in males and in older subjects [4, 11,12,13,14,15].
Several studies have shown the prognostic value of dyspnea, which could be used to complement FEV1 in the classification of COPD severity. Even in some studies, it has been observed that dyspnea exceeds FEV1 in predictive value of mortality [16, 17]. In our study, most of the patients had a degree of dyspnea of 2–3, being worst the grade in the HFR group. Some authors have identified a greater degree of dyspnea as a risk factor for readmission in these patients [18, 19].
Regarding spirometric parameters, the severity of airway obstruction was greater in HFR group compared to LFR in our study. Some authors have shown that there is a statistically significant relationship between COPD severity and the number of hospitalizations per year [20]. In some studies, it has also been observed that a lower FEV1 value is a high-risk factor for hospital readmission [18, 19].
An interesting and novel finding of our study is the relationship between the COPD phenotype and the risk of readmission. Patients with exacerbator emphysema phenotype had a risk of readmission of almost 30 times greater than those with non-exacerbator phenotype. These results complement those obtained by other authors [21], who have shown that patients requiring readmission within 30 days following an acute exacerbation have predominantly an emphysematous phenotype.
Comorbidities are common in COPD hospitalized patients, and they are related to their short-term prognosis [22, 23]. In our study, no differences were found in Charlson Comorbidity Index in HRF and LFR groups, although there were significant differences for diabetes. Some authors have observed, as in our study, that diabetes was associated with an increase in readmissions rates within 30 days after discharge [13, 14]. Others have shown that patients with more comorbidities and with chronic conditions such as congestive heart failure, osteoporosis, anemia, depression, and psychosis or history of lung cancer, are readmitted more frequently [13, 14, 24,25,26].
Several studies have found that pneumococcal vaccination is a very important tool for the prevention of pneumococcal pneumonia, both in general population and in COPD patients [27, 28]. However, other authors have suggested that the decrease in mortality in these patients is more related to influenza vaccination and not so much to the pneumococcal vaccine [29, 30]. In our study, there were no differences in the proportion of patients vaccinated against influenza or pneumococcus in the two groups analyzed.
Regarding arterial blood gas parameters, in our study we did not find significant differences in PaO2 levels at discharge between patients of the HFR and LFR groups. In previous studies it has been shown that this parameter does not seem to contribute to predicting the following exacerbation and it is an indicator of the severity of the illness, so it is more related to in-hospital mortality [31,32,33].
More than one-third of the patients in our study suffered from a decompensation of some underlying chronic condition during hospital admission, being heart failure the most frequent, with a greater percentage in the HFR group compared to LFR group. In addition, those patients who experienced onset or decompensation of heart failure during admission had a fivefold higher risk of hospital readmission. The high prevalence of heart failure among COPD patients is not surprising since these subjects have an increased risk of cardiovascular morbidity and mortality, regardless of other factors [12, 34]. Other authors have shown that patients with congestive heart failure have a higher rate of readmissions and earlier [13, 14, 24].
Previous studies have shown that COPD patients who have been treated with non-invasive mechanical ventilation (NIMV) during severe exacerbation have a high probability of readmission in the year following discharge and they have high mortality [35,36,37]. In ours we observed that, although this therapeutic modality was required by a greater percentage of patients in the HFR group, no differences were found in the readmission risk in relation to their use between the two groups. There were also no differences in the readmission risk according to the history of admissions to an intensive care unit.
An area for future investigations is to explore the relationship between length of stay and readmission for high-risk patients. In our study, the length of hospital admission was lower in the patients of HFR group compared to those of the LFR group. The higher frequency of complications during admission in this last group of patients could justify these results. Several studies have also shown an inverse relationship between days of hospital stay and readmissions, and that higher length of stay seem to be related to lower mortality during follow-up [3, 25, 38]. Thus, increasing the lengths of stay in the original hospitalization may lead to fewer readmissions and better outcomes. In any case, other authors have observed that, more than the length of hospital stay, a factor that could influence the risk of readmission is the patient’s condition at discharge, so that clinical stability at discharge could be associated with lower readmission rates at 30 days [8].
From the results obtained the multivariable analysis, the profile of COPD patients with high risk of readmission has been established. Some authors have objectified factors similar to those obtained in our study: age, male gender, degree of dyspnea, associated comorbidities (including heart failure), a lower value of FEV1, a higher Charlson Comorbidity Index, and a shorter duration of initial admission [3, 13,14,15, 18, 19, 24, 35, 38]. In contrast to our results, other authors have also found that the following were risk factors for rehospitalization: active smokers, chronic bronchitis phenotype, high length of hospital stay, low prevalence of vaccination, and complications during admission, with worse recovery/higher incidence of use of the intensive care unit [2, 13, 18, 19, 24, 35]. In addition, other factors for readmissions have been identified, which include the following: African American race, worse socioeconomic conditions, drug abuse, low body mass index, history of hospital admissions, use of steroids and nebulizers, duration of disease greater than 10 years, respiratory acidosis and abnormal levels of carbon dioxide during initial admission, clinical instability at discharge, absence of short-acting bronchodilators at discharge, lack of follow-up after discharge, difficulty in accessibility to treatments and oxygen therapy, and absence of respiratory rehabilitation programs [8, 13,14,15, 18, 19, 37, 38].
It is important to identify the group of patient with higher readmission risk in clinical practice, in order to reinforce medical monitoring and home follow-up during the immediate post-discharge period. This would reduce the risk of further exacerbation and, if it occurs, establish an early treatment so that recovery is faster and the risk of hospitalization is lower. In some studies, a number of strategies have been described to reduce readmissions following an exacerbation of COPD, including patient education, training of respiratory inhalation devices, early monitoring within 30 days after discharge by a primary care physician or pulmonologist, and respiratory rehabilitation [19]. The use of this last modality of treatment has been related to a decrease in readmissions and mortality in COPD patients, since it improves dyspnea and exercise capacity, even in elderly patients with COPD [10, 39, 40]. The identification of respiratory acidosis or chronic hypercapnia, by performing an arterial blood gas analysis, with the subsequent increase in the use of resources such as non-invasive ventilation, which increases survival in a COPD exacerbation, could help reduce readmissions [19, 37]. There are other emerging interventions that may contribute to decreasing readmissions, such as treatment of COPD exacerbation at home for certain patients, planning discharge, scheduling a follow-up appointment before discharge, dispensing all drugs and respiratory treatments such as oxygen therapy before hospital discharge, pharmacist supervision of medication management by the patient, use of drugs such as roflumilast, follow-up telephone calls, home visits after discharge, and use of telehealth/telemedicine [1, 8, 19, 38, 41].
This study has some limitations. Patients who were included in the LFR group were those who were not readmitted 30 days after discharge by COPD exacerbation, but it did not take into account the history of hospital admissions in the previous year nor the rest of hospitalizations during the year 2015. On the other hand, no distinction was made with respect to the department of hospitalization to measure the length of hospital stay during the initial admission. Additionally, the family or social status of the patients was not considered, which could have influenced the results obtained in this study. Finally, to generalize the findings, it is important to bear in mind that the results of this study are applicable to patients in our health area, where the reduced distance from the home of the patients to the hospital facilitates their access, to the detriment of the request for assistance by the Primary Assistance.
In conclusion, the only variables that maintained statistical significance in our study in the association with the risk of readmission were sex, phenotype, appearance of complications during admission, length of hospital stay, and the decompensation or the appearance of heart failure. It is important to take these results into account in order to recognize patients who would benefit most from strategies to reduce readmissions.
References
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J et al (2017) Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med 195:557–582
Miravitlles M, Soler-Cataluña JJ, Calle M, Molina J, Almagro P, Quintano JA et al (2017) Spanish guidelines for management of chronic obstructive pulmonary disease (GesEPOC) 2017. Pharmacological treatment of stable phase. Arch Bronconeumol 53:324–335
Escarrabill J, Torrente E, Esquinas C, Hernández C, Monsó E, Freixas M et al (2015) Clinical audit of patients hospitalized due to COPD exacerbation. MAG-1 study. Arch Bronconeumol 51:483–489
Llauger Roselló MA, Pou MA, Domínguez L, Freixas M, Valverde P, Valero C (2011) Treating COPD in chronic patients in a primary-care setting. Arch Bronconeumol 47:561–570
Atención integral al paciente con enfermedad pulmonar crónica (EPOC) desde la atención primaria hasta la especializada. Guía de práctica clínica 2010: semFYC/ SEPAR. http://www.guiasalud.es/GPC/GPC_468_EPOC_AP_AE.pdf
Calle Rubio M, Morales Chacón B, Rodríguez Hermosa JL (2010) Exacerbation of chronic obstructive pulmonary disease. Arch Bronconeumol 46(Suppl 7):21–25
Lindenauer PK, Dharmarajan K, Qin L, Lin Z, Gershon AS, Krumholz HM (2017) Risk trajectories of readmission and death in the first year following hospitalization for COPD. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.201709-1852OC
Nasser R, Epstein D, Azzam R, Gofman I, Saliba W, Hardak E et al (2017) The effect of clinical and physiological instability at discharge following hospitalization for acute exacerbation of COPD on early readmission: a cohort study. Chest 151:1192–1194
Goto T, Faridi MK, Gibo K, Toh S, Hanania NA, Camargo CA Jr et al (2017) Trends in 30-day readmission rates after COPD hospitalization, 2006–2012. Respir Med 130:92–97
De Granda-Orive JI, Solano-Reina S (2016) Chronic obstructive pulmonary disease mortality. SEPAR COPD-Smoking year. Arch Bronconeumol 52:407–408
McGhan R, Radcliff T, Fish R, Sutherland ER, Welsh C, Make B (2007) Predictors of rehospitalization and death after a severe exacerbation of COPD. Chest 132:1748–1755
Vidal García I, Calvo Álvarez U, Lijó Carballeda C, Souto Alonso A, Diego Roza C, Mejuto Martí MJ et al (2012) Características de pacientes con EPOC ingresados por exacerbación en el área sanitaria de Ferrol. Pneuma 8:4–7
Sharif R, Parekh TM, Pierson KS, Kuo YF, Sharma G (2014) Predictors of early readmission among patients 40 to 64 years of age hospitalized for chronic obstructive pulmonary disease. Ann Am Thorac Soc 11:685–694
Lau CS, Siracuse BL, Chamberlain RS (2017) Readmission after COPD exacerbation scale: determining 30-day readmission risk for COPD patients. Int J Chron Obstruct Pulmon Dis 12:1891–1902
Roberts MH, Clerisme-Beaty E, Kozma CM, Paris A, Slaton T, Mapel DW (2016) A retrospective analysis to identify predictors of COPD-related rehospitalization. BMC Pulm Med 16:68
Nishimura K, Izumi T, Tsukino M, Oga T (2002) Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 121:1434–1440
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA (1999) Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 54:581–586
Gaude GS, Rajesh BP, Chaudhury A, Hattiholi J (2015) Outcomes associated with acute exacerbations of chronic obstructive pulmonary disorder requiring hospitalization. Lung India 32:465–472
Shah T, Press VG, Huisingh-Scheetz M, White SR (2016) COPD readmissions: addressing COPD in the era of value-based healthcare. Chest 150:916–926
Tsoumakidou M, Tzanakis N, Voulgaraki O, Mitrouska I, Chrysofakis G, Samiou M et al (2004) Is there any correlation between the ATS, BTS, ERS and GOLD COPD’s severity scales and the frequency of hospital admissions? Respir Med 98:178–183
Castillo A, Edriss H, Selvan K, Nugent K (2017) Characteristics of patients with congestive heart failure or chronic obstructive pulmonary disease readmissions within 30 days following an acute exacerbation. Qual Manag Health Care 26:152–159
Almagro P, Cabrera FJ, Díez J, Boixeda R, Alonso Ortiz MB, Murio C et al (2012) Comorbidities and short-term prognosis in patients hospitalized for acute exacerbation of COPD: the EPOC en Servicios de medicina interna (ESMI) study. Chest 142:1126–1133
De Miguel Díez J, Gómez García T, Puente Maestu L (2010) Comorbidities in COPD. Arch Bronconeumol 46(Suppl 11):20–25
González G, Servera E, Ferris G, Blasco ML, Marín J (2004) Risk factors of readmission in acute exacerbation of moderate-to-severe chronic obstructive pulmonary disease. Arch Bronconeumol 40:502–507
Simmering JE, Polgreen LA, Comellas AP, Cavanaugh JE, Polgreen PM (2016) Identifying patients with COPD at high risk of readmission. Chronic Obstr Pulm Dis 3:729–738
Echevarria C, Steer J, Heslop-Marshall K, Stenton SC, Hickey PM, Hughes R et al (2017) The PEARL score predicts 90-day readmission or death after hospitalisation for acute exacerbation of COPD. Thorax 72:686–693
Alfageme I, Vázquez R, Reyes N, Muñóz J, Fernández A, Hernández M et al (2006) Clinical efficacy of anti-pneumococcal vaccination in patients with COPD. Thorax 61:189–195
Lee TA, Weaver FM, Weiss KB (2007) Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med 22:62–67
Schembri S, Morant S, Winter JH, MacDonald TM (2009) Influenza but not pneumococcal vaccination protects against all-cause mortality in patients with COPD. Thorax 64:567–572
Schenkein JG, Nahm MH, Dransfield MT (2008) Pneumococcal vaccination for patients with COPD: current practice and future directions. Chest 133:767–774
Jurado Gámez B, Feu Collado N, Jurado García JC, García Gil F, Muñoz Gomariz E, Jiménez Murillo L et al (2013) Intervención domiciliaria y variables predictoras para reingreso hospitalario en la enfermedad pulmonar obstructiva crónica agudizada. Arch Bronconeumol 49:10–14
Groenewegen KH, Schols AM, Wouters EF (2003) Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest 124:459–467
Almagro P, Barreiro B, Ochoa de Echaguen A, Quintana S, Rodriguez Carballeira M, Heredia JL (2006) Risk factors for hospital readmission in patients with chronic obstructive pulmonary disease. Respiration 73:311–317
Villar Álvarez F, Méndez Bailón M, De Miguel Díez J (2009) Chronic obstructive pulmonary disease and heart failure. Arch Bronconeumol 45:387–393
Echave-Sustaeta J, Comeche Casanova L, García Luján R, Sayas Catalan J, de la Cámara AG, Encuentra AL (2010) Prognosis following acute exacerbation of COPD treated with non-invasive mechanical ventilation. Arch Bronconeumol 46:405–410
Chu CM, Chan VL, Lin AWN, Wong IWY, Leung WS, Lai CKW (2004) Readmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failure. Thorax 59:1020–1025
Hartl S, Lopez-Campos JL, Pozo-Rodriguez F, Castro-Acosta A, Studnicka M, Kaiser B et al (2016) Risk of death and readmission of hospital-admitted COPD exacerbations: European COPD Audit. Eur Respir J 47:113–121
Maciá Soler L, Latour Pérez J, Moncho Vasallo J, Mariscal Crespo MI, Orts Cortés MI (2011) Modelo de hospitalización y frecuencia de reingreso en pacientes con exacerbación de EPOC. Enferm Glob 10:1–10
Sundararajan L, Balami J, Packham S (2010) Effectiveness of outpatient pulmonary rehabilitation in elderly patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev 30:121–125
Williams V, Bruton A, Ellis-Hill C, McPherson K (2010) The effect of pulmonary rehabilitation on perceptions of breathlessness and activity in COPD patients: a qualitative study. Prim Care Respir J 19:45–51
Hansen LO, Young RS, Hinami K, Leung A, Williams MV (2011) Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med 155:520–528
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cerezo Lajas, A., Gutiérrez González, E., Llorente Parrado, C. et al. Readmission Due to Exacerbation of COPD: Associated Factors. Lung 196, 185–193 (2018). https://doi.org/10.1007/s00408-018-0093-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-018-0093-y