Abstract
Depression affects 7% of the elderly population, and it often remains misdiagnosed or untreated. Peripheral biomarkers might aid clinicians by allowing more accurate and well-timed recognition of the disease. We sought to determine if plasma protein levels predict the severity of depressive symptomatology or distinguish patients from healthy individuals. The severity of depressive symptoms and global cognitive functioning were assessed by the Geriatric Depression Scale (GDS) and Mini-Mental State Examination (MMSE) in 152 elderly subjects, 76 of which with major depressive disorder (MDD). Plasma levels of 24 proteins were measured by multiplexing and analyzed as continuous predictors or dichotomized using the median value. The association between individual plasma proteins and MDD risk or depressive symptoms severity was investigated using multiple logistic and linear regressions including relevant covariates. Sensitivity analyses were performed excluding cognitively impaired individuals or non-acute patients with MDD. After adjusting for possible confounders and false discovery rate (FDR) correction, we found lower Fetuin-A levels in MDD patients vs. controls (pFDR = 1.95 × 10–6). This result was confirmed by the sensitivity and dichotomized analyses. Lower prolactin (PRL) levels predicted more severe depressive symptoms in acute MDD patients (pFDR = 0.024). Fetuin-A is a promising biomarker of MDD in the elderly as this protein was negatively associated with the disorder in our sample, regardless of the global cognitive functioning. Lower PRL levels may be a peripheral signature of impaired neuroprotective processes and serotoninergic neurotransmission in more severely depressed patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The world population aged over 60 is rapidly growing, and it is expected to more than double within the next 30 years [1]. Greater attention to the mental health of elderly people will be necessary, as psychiatric morbidity is bidirectionally linked with worse physical health and with higher mortality rates [2, 3].
Depression affects 7% of the general elderly population, and two-thirds of elderly depressed patients remain untreated [4,5,6]. Among the existing aetiopathogenic hypotheses, some authors have suggested a contribution of vascular pathology and aging-related neurodegeneration, as well as metabolic and immune-inflammatory mechanisms to late-life depression [7].
The diagnosis of major depressive disorder (MDD) is currently based on standardized clinical criteria, and no objective biomarker is available to assist diagnosis, prognosis formulation, or disease monitoring. Discovery and validation of peripheral biomarkers for depression would reduce the misdiagnosis rate and the time before an adequate treatment is prescribed. It could also enhance precision medicine, providing criteria to monitor antidepressant response. Proteomics studies might also confirm the existing pathogenetic hypotheses, suggest new pathogenetic pathways, or lead to the discovery of new pharmacologic targets.
Peripheral blood is a more accessible tissue to derive useful information for clinical practice compared to other tissues such as cerebrospinal fluid. Altered levels of circulating proteins may not directly reflect pathogenic processes within the CNS, but they may be the result of bidirectional cross-talks between the brain and the periphery through the neuroendocrine and immune system [8]. This interaction may be facilitated by blood–brain barrier dysfunction, which results in increased permeability to inflammatory mediators in MDD [9]. Proteins may be good biomarkers, also because they are biologically more proximal to the disease phenotype, and they allow to study the ultimate product deriving from the stratification of environmental variables, as well as genetic, epigenetic, and post-transcriptional/translational modifications. To date, however, the identification of cost-effective biomarker panels with good diagnostic performance is still an arduous and ambitious challenge, mostly due to the heterogeneous nature of depression and its complex etiology [7, 10].
Over the years, a broad range of circulating polypeptides has been collectively tested as peripheral biomarkers of MDD [11,12,13]. Proteomics studies identified analytes belonging to cellular communication and signal transduction processes, immune response, and coagulation cascade as associated with MDD [11, 12], while analytes involved in endocrine function, synaptic plasticity, or angiogenesis were associated with late-life depression [13].
These results and the known biologically dysfunctions involved in MDD pathogenesis may serve as starting point for further studies. Among the strongest findings in the literature, immune-inflammatory mechanisms were repeatedly associated with MDD and may partially mediate the link between cardiovascular disease (CVD) and depression [7, 14]. Among others, CTNF (ciliary neurotrophic factor) and Fetuin-A are biomarkers of processes related to inflammation [15], such as macrophage chemoattraction and polarization to a pro-inflammatory M1 subtype [16], and they have been associated with depression [17,18,19,20,21]. Other potential biomarkers have endocrine activity, such as adipokines, produced by the adipose tissue, or adenohypophyseal hormones. For example, prolactin (PRL) is a pituitary hormone which participates in neurogenesis and neuroprotection within the CNS [22], and its secretion is modulated by the serotoninergic system which is notoriously impaired in depression [23]. The hypothalamic–pituitary–adrenal axis (HPA) was demonstrated to be hyperactive in MDD, and gonadotropins may influence monoamine release and consequently mood and behavior [24, 25]. The gonadotropin FSH (follicle-stimulating hormone) was repeatedly associated with depression, especially in women [26, 27]. Adipokines also impact on neurotransmission pathways, and they may modulate the HPA axis function, resulting in anti-depressive effects [14, 28, 29]. Other polypeptides may be investigated as they act as neurotrophic factors [e.g., brain-derived neurotrophic factor (BDNF)] or have a role in neurodevelopment or synaptic plasticity, processes which have previously been implicated in MDD [14, 30, 31]. Multiple evidence also suggests a role of the fibrinolytic system in depression, which takes part in the proteolytic activation of pro-BDNF [32]. Plasminogen activator inhibitor-1 (PAI-1) is the primary regulator of fibrinolysis in humans, and genetic polymorphisms in PAI-1 gene were associated with MDD susceptibility, as well as with antidepressant response [33].
Given the potential role of the described groups of proteins in MDD, this study aimed to determine if individual plasma protein levels were associated with: (1) MDD diagnosis in an elderly sample; (2) the severity of depressive symptoms in elderly patients with MDD.
Methods
Study population
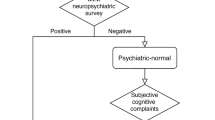
All the subjects included in our analyses were part of the Ansan Geriatric (AGE) study. AGE was a prospective population-based cohort study aiming to collect wide-ranging information on the global health status of non-institutionalized civilians aged 60–84 years in Ansan-si (metropolitan area of Seoul), South Korea. The study protocol has been described elsewhere [34, 35]. The baseline sample was constituted by 2767 subjects, after the exclusion of individuals who supplied incomplete information or were not eligible for a probability sample proportional to the gender- and age-specific structure of the target population. From September 2004 to March 2006, 1391 individuals were randomly selected to take part in the first wave of the study. Of the 1391 participants, 777 were assessed for psychiatric disorders by the Korean version of the Mini-International Neuropsychiatric Interview (MINI) [36]. A consensus meeting of a psychologist, a psychiatrist, and a neurologist derived the final diagnosis of MDD. As a result, 124 depressed and 653 non-depressed individuals were identified. Among them, 76 patients with MDD and 76 healthy controls (HCs) were selected by random sampling to be included in the present study. This sample size was considered to have enough power (0.80) to detect a Cohen’s d = 0.46 at α level = 0.05 for testing between-group differences of continuous plasma protein concentrations.
In our sample, all the patients with MDD had a symptom onset after 60 years of age, and only 6 out of 76 MDD patients were on antidepressant treatment at the time of blood sampling. Indeed, subjects were not collected in a clinical trial setting but based on a community-based cohort study design [34]. Socio-demographic and clinically relevant data, including any history of medical diseases as well as the current use of antidepressant and anti-inflammatory drugs, were collected at the baseline.
All participants provided written informed consent. The study protocol was approved by the institutional review boards of the Catholic University of Korea Bucheon St. Mary's Hospital (HC14EISI0040) and Korea University Ansan Hospital (2017AS0182).
Evaluation of depressive symptom severity and global cognition
Depressive symptom severity was assessed by the Korean version of the 30-item Geriatric Depression Scale (GDS-K), a self-rating scale which has shown optimal psychometric performances in older adults. GDS items explore the cognitive and affective domains of depression, excluding any somatic symptom, which might be misleading in the elderly [37, 38].
The Korean version of the Mini-Mental State Examination (MMSE-KC) was used to evaluate the overall cognitive functioning, and scores were adjusted for education and age [39, 40]. MMSE-KC is composed of 20 items, which evaluate orientation, registration, attention/calculation, language/praxis, and recall. Lower scores (ranging from 0 to 30) indicate worse performance [40]. An adjusted score of 25 (indicating normal) showed a sensitivity of 0.97 (95% CI 0.83–1.00) for the detection of dementia in community-dwelling elderly individuals [41].
Plasma protein level measurement
Plasma samples were analyzed using a multiplex Luminex®-based technology. Additional details about the measurement techniques are available in the Supplementary information—paragraph 1. The full list of the measured plasma proteins and the corresponding acronyms are reported in Table S1, along with references related to the previous evidence supporting their involvement in the etiopathogenetic mechanisms of MDD or depressive phenotypes. All the concentration values were log10 transformed to make them fit a Gaussian distribution.
The measured analytes were chosen based on the previous literature evidence of a biological relationship with processes or pathways known to be directly or indirectly implicated in MDD pathogenesis.
Statistical analysis
As a primary outcome, continuous protein concentration values were used to test any difference between MDD patients and HCs and to predict the severity of depressive symptoms in MDD.
As a secondary outcome, dichotomised protein concentrations were used to perform the same analyses. We used a median split procedure to divide the distribution of data into two categories (i.e., low and high concentration) of equal size. Given our sample size, this allowed us to avoid skewness problems, as well as the creation of very small subgroups that would reduce power. Although dichotomized regressors may provide lower power than continuous ones, it is possible that biological effects do not follow a linear variation and differences may be seen only for those having the highest values.
Outliers were manually detected and removed by deleting plasma protein values that fell outside 3 SD (standard deviations) from the mean and at least 1 SD from the distribution tails. This led to the exclusion of just 0.3% of the measured protein concentrations.
At first, between-group differences were evaluated by Student’s t test, Chi-square test, and Fisher's exact test as appropriate. Linear and logistic regressions were applied afterwards to test the previously described hypotheses. For each tested linear regression model, scatter diagrams of observed residuals and normal probability plots were inspected to avoid violations of the assumptions. The significance of logistic regression models was assessed by the Z statistics, and the case/control (MDD/healthy) status was included as the binary dependent variable. Age, gender, BMI, smoking attitude, alcohol consumption, use of antidepressants, and NSAIDs (non-steroidal anti-inflammatory drugs) were included as covariates in the linear and logistic regressions according to the previous literature evidence [11, 12, 42,43,44,45]. We also included MMSE scores among the covariates, because it was significantly different between HCs and MDD patients in our sample, but we did not include hypertension and cardiac diseases, because they did not differ between MDD patients and HCs, as well as they were not associated with plasma proteins in our sample. Nonetheless, use of antidepressants was included as a confounder in the linear but not in the logistic regression models because of a complete separation issue, which arises when a response variable is perfectly predicted by an independent variable. It was precisely due to the presence of only six individuals treated with antidepressants in our sample, all of whom belonged to the MDD patient subgroup, as expected.
We also performed two sensitivity analyses: (1) cognitively impaired subjects (MMSE-KC adjusted scores < 25) were excluded; (2) non-acute or sub-threshold MDD patients (GDS-K scores < 11) were excluded from the MDD subsample. Indeed, these subjects might represent a source of bias when the associations of plasma protein concentrations with MDD risk or depressive symptom severity were tested. Indeed, GDS may perform worse in individuals with impaired cognitive function [46], and plasma protein concentrations may vary depending on the acute or non-acute phase of depression [47].
All the analyses were performed using STATISTICA version 12 (StatSoft Inc., 2014—www.statsoft.com). The adaptive linear step-up procedures were applied to correct for multiple testing the levels of significance at the maximum acceptable false discovery rate (FDR) set at (q = 0.05 [48].
Results
Socio-demographic and clinical characteristics of the sample
A total of 152 participants were included in the study, 76 in the control group and 76 in the depressed group. The detailed socio-demographic and clinical characteristics of the study sample are reported in the Supplementary information—paragraph 2 and Table S2.
Comparison between patients with MDD and healthy individuals
All the 24 measured plasma proteins had > 80% of detected values in our sample (details are in Table S3). In univariate analyses, several plasma proteins showed higher mean values in MDD: FSH, NCAM (neural cell adhesion molecule), NGAL (neutrophil gelatinase-associated lipocalin), and sICAM-1 (soluble intercellular adhesion molecule-1), but only FSH remained significant after FDR correction. Conversely, BDNF (Brain-derived neurotrophic factor), Fetuin-A, and PAI-1 (Plasminogen activator inhibitor-1) showed lower mean values in MDD patients; only Fetuin-A and PAI-1 remained significant after FDR correction (Table S4a). For BDNF, FSH, NCAM, and NGAL, the significance was exclusively driven by differences between HCs and patients in the acute phase of MDD, whereas for Fetuin-A, PAI-1, and sICAM-1, there was also a minor contribution of ten non-acute patients to the overall significance (data are not shown). No significant between-group differences were found for the other plasma protein concentrations.
Multiple logistic regression, including the relevant covariates, showed negative associations between Fetuin-A, PAI-1, and MDD, while higher FSH levels were associated with MDD risk, after FDR correction. At a nominal significance level, higher sICAM-1 was associated with MDD, whereas subjects with higher levels of BDNF had a lower risk of MDD (Table 1).
The removal of 27 subjects with MMSE-KC adjusted scores < 25 (indicating cognitive impairment) caused FSH and PAI-1 associations to lose the statistical significance, while the effect of Fetuin-A was still observed (data are not shown). FSH was not associated with MDD risk after the exclusion of ten patients with GDS-K scores < 11 (non-acute MDD) from the analyses, while PAI-1 and Fetuin-A were still significantly associated with MDD.
After the dichotomization of the plasma protein levels (secondary analyses) and FDR correction, high Fetuin-A levels were associated with reduced MDD risk, while PAI-1 showed only nominal significance. High CNTF levels were associated with higher MDD risk. At a nominal significance level, NGAL and sICAM-1 levels were positively associated with MDD risk. Detailed results are shown in Table S5 and Fig. 1.
Distribution of the mean values (± SD, standard deviations) of plasma Fetuin-A (in ng/mL), FSH (in mIU/mL), and PAI-1 levels (in pg/mL) in healthy individuals and patients with MDD (major depressive disorder). MDD major depressive disorder, SD standard deviation. **Significant results at Student’s t test after false discovery rate (FDR) correction for multiple comparisons
Association between protein plasma levels and depressive symptom severity in MDD patients
Taking into account the effect of possible confounders and after FDR correction, none of the tested biomarkers predicted depressive symptom severity (GDS-K scores) in patients with MDD regardless of the acute or non-acute phase of the disease. At the nominal significance level, multiple regression analyses showed that plasma PRL (prolactin) levels and sVCAM-1 (soluble vascular cell adhesion molecule-1) were negatively associated with GDS-K scores in patients with MDD (Table S6).
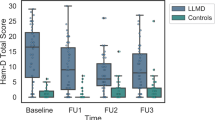
The removal of 27 subjects with MMSE-KC adjusted scores < 25 from the analyses had no substantial effect on the results (data are not shown). A negative association between PRL levels and depression severity was statistically significant after the removal of ten non-acute MDD patients (Fig. 2). Results are shown in Table S7.
After the dichotomization of the plasma protein levels (secondary analyses), we did not find any association with depression symptom severity (Table S8).
Discussion
In the present study, we investigated differences in plasma protein levels between MDD patients and HCs in a cohort of community-dwelling elderly individuals. We also studied whether plasma protein levels might predict the severity of depressive symptomatology in MDD patients.
After FDR correction and considering potential confounders, we found lower Fetuin-A and PAI-1, as well as higher FSH levels in patients with MDD vs. HCs. After the exclusion of cognitively impaired subjects, only the effect of Fetuin-A was still observed, while after the exclusion of ten non-acute MDD patients, both the effects of Fetuin-A and PAI-1 survived. The effect of Fetuin-A on MDD risk was also confirmed after the dichotomization of protein levels. Using the dichotomization approach, CNTF levels were positively associated with MDD risk.
Fetuin-A is a negative acute phase glycoprotein, primarily secreted by the liver, with a role in neuroprotection and neurodevelopment [49, 50]. In human post-mortem mature brain, Fetuin-A is predominantly expressed in neurons and astrocytes, while in the developing brain, it is also found in CD68-positive microglia [51]. Fetuin-A levels have been inversely correlated with atherosclerosis severity and vascular calcifications [52], as well as with cognitive performance in the elderly and Alzheimer disease [53, 54], supporting a link with MDD in the elderly [7, 55]. Of note, the exclusion of cognitively impaired patients from the analysis did not change the significance of our result. A previous study also found higher levels of Fetuin-A in MDD vs. controls, but only in males [21]. We did not perform any analysis stratified by gender because of a power issue (our sample mostly included females).
PAI-1 levels had a negative association with MDD risk, although it was not confirmed after the exclusion of subjects with cognitive impairment and dichotomization of the data. PAI-1 is mainly involved in the inhibition of fibrinolysis in humans. However, specific actions have been described for PAI-1 within the CNS. In the CNS, PAI-1 has an indirect effect on synaptic plasticity by reducing the production of active BDNF from its precursor and modulating the activity of N-methyl-d-aspartate (NMDA) receptors through the inhibition of the tPA-plasmin pathway [56]. Both neurotoxic and neurotrophic effects have been described for PAI-1 [56, 57]. Our result is not consistent with a study showing an opposite effect in a sample of elderly depressed patients with comorbid type 2 diabetes [58]. The reduction of plasma PAI-1 in our MDD subsample also contrasts with the previous evidence of a prothrombotic state in MDD and inverse association between PAI-1 levels and CVD [59]. This may be partly due to a reduction of TNF-⍺ in our MDD subsample, as we pointed out in our previous work [60]. Indeed, pro-inflammatory cytokines may upregulate PAI-1 expression [61], as it was demonstrated in vivo in both microglia and astrocytes during neuroinflammation [62]. Ethnicity might also explain some differences, since South Asian individuals have shown increased risk of CVD compared to Caucasians [63].
FSH levels were inversely associated with MDD, although this association was not confirmed after excluding non-acute MDD patients or cognitively impaired individuals. FSH is a pituitary gonadotropin with a key role in reproductive physiology in both men and women [64], and it was previously implicated in depression risk in peri- and post-menopausal women [27], despite negative results were also reported [65,66,67]. In longitudinal studies considering the menopausal transition or the post-menopausal phase, a higher change in the FSH levels over time was associated with depression [68, 69]. Given the relevant fluctuations of FSH during distinct phases of life, it is reasonable to hypothesize that the entity of fluctuations rather than the absolute value may be associated with depression. Our sample was mostly represented by elderly women, and this may explain the higher FSH levels in MDD compared to HCs; indeed, gonadotropins did not show alterations in depressed males [70].
The analyses of dichotomized biomarker levels showed that higher CNTF was associated with MDD. CNTF is a cytokine expressed by both neuronal and glial cells, belonging to the interleukin-6 (IL-6) family [71]. It exerts pro-inflammatory actions in the brain, by activating microglia in vitro and in vivo [72, 73]. CTNF-induced neuroinflammation results in a significant decrease in neuronal metabolism [74]. At the behavioral level, it leads to the development of sickness behavior by causing fever, anorexia, and reduced locomotor activity, which parallel the increase of IBA-1 (ionized calcium-binding adaptor molecule 1) positive microglia and inflammatory cytokines, such as IL-1β and TNF-α, into the brain [71]. A previous study found elevated CNTF levels in MDD vs. HCs [17], and animal models suggested that CNTF promotes depressive-like behaviors in a sex-specific manner in mice [18], although contrasting findings were reported [75].
Altogether, our novel findings of lower plasma Fetuin-A, higher CNTF, and, possibly, lower PAI-1 in patients with MDD are in agreement with evidence that microglia-mediated processes are implicated in the pathophysiology of the disorder [76]. Reduced Fetuin-A may result in the impaired anti-inflammatory activity of the polyamine spermine, whose mechanism depends on the availability of Fetuin-A, as well as in increased microglial activation [77]. CNTF was shown to stimulate microglial phagocytosis through a calcium-mediated upregulation of integrin ⍺v, and to determine a shift toward amoeboid-shape activated microglia [73, 78]. Although lower PAI-1 levels may be the consequence of blunted pro-inflammatory stimuli on microglia, reduced PAI-1 may also promote microglial phagocytic activity through the disinhibition of the vitronectin/integrin beta-2 (ITGβ2)/Toll-like receptor 2 (TLR2) complex [62]. The neuroinflammation associated with depression has been confirmed by in vivo PET studies of microglial activation in patients [79]. The interpretation of this finding is still under debate, and several different mechanisms have been proposed, including an inborn dysregulation of the immune system leading to auto-inflammatory reactivity, psychological stress, and exposure to infectious agents [80]. To date, it is still difficult to disentangle how peripheral circulating proteins, which often have a contrasting effect, can together influence the functionality of brain networks and behaviour. They could act in a region-specific manner within the CNS, and their effect may depend on their sequential exposure to target cells [81]. Region-specific functions of microglia have also been reported, which could determine the divergent results in terms of neuroplasticity found in models of stress-induced depression [82, 83]. Therefore, the interpretation of the present results has to be considered with caution.
Other results did not survive after multiple-testing correction; among them, one of the most investigated biomarkers is BDNF that was only nominally lower in MDD cases vs. HCs. Previous evidence suggested a reduction in peripheral BDNF levels in MDD compared to HCs, also in late-onset depression [84, 85], although contrasting results have also been reported [86, 87]. An important observation is that there is very high discrepancy in BDNF levels between serum and plasma [88], and plasma BDNF levels are also less reproducible than in serum [89], possibly explaining the observed discrepancies in the results.
The only biomarker associated with depressive symptom severity, after FDR correction, was PRL, which showed a negative association with symptom severity in acute MDD. PRL is an endocrine hypophyseal peptide with a key role in maternal behavior, as well as in adaptation to stress and resilience. It also participates in neurogenesis and neuroprotection within the CNS [22] and its secretion is modulated by the serotoninergic system, which is impaired in depression [23]. Our result is consistent with the previous findings in a large male sample [90]. However, it is necessary to consider that plasma PRL measurements may be subjected to unreliability due to pulsatile secretion and circadian changes [23]. Its levels may also be affected by the presence of concomitant physical diseases or mild acute stress as well, including venepuncture [91]. We could not exclude that unknown concomitant medications or confounders might be a potential source of bias for this result. Antidepressants themselves were associated with increase in prolactin levels [92], but this is unlikely to have affected our results, since only 6 out of 76 patients with MDD were taking antidepressants and we included antidepressant use among covariates.
Our findings should be interpreted in light of some limitations. First of all, our cross-sectional approach was not able to evaluate the temporal variations of the considered plasma proteins. Indeed, MDD is associated with a higher fluctuation of symptoms [93], and this may correspond to a dynamic fluctuation of peripheral protein levels. On the other hand, not all our MDD patients were during an acute phase of illness, but this did not affect our main findings as demonstrated by excluding patients with sub-thresholds GDS-K scores. We can not rule out that other unobserved factors may have affected our measurements, such as physical activity, other physical comorbidities, and concomitant pharmacotherapies. GDS may not maintain its validity in people with severe cognitive impairment and this was addressed by doing a sensitivity analysis. It is worth noting that the used MMSE cut-off score of 25 was demonstrated a very high sensitivity in identifying individuals with dementia, although it may have relatively low specificity [94]. However, the use of a less conservative threshold of 18 did not substantially change the results of the corresponding sensitivity analysis. Finally, we did not perform an independent replication of our findings, which would have allowed us to validate our findings.
In conclusion, lower Fetuin-A and PAI-1, as well as higher CNTF and FSH levels may be predictors of MDD risk in elderly subjects. PRL levels were negatively associated with depression symptom severity in acute MDD patients. If confirmed in larger independent samples and post-mortem studies, our present observations suggest that pathways involving CNTF, Fetuin-A, and possibly PAI-1 might play a role in microglia dysregulation associated with MDD. Measurement of peripheral biomarkers could be a viable alternative to more unwieldy brain imaging techniques for the assessment of neuroinflammation associated with depression in clinical settings, helping to identify patients at risk for the neuroprogression of the disease. Future studies will help to investigate longitudinally the association between these promising biomarkers and MDD diagnosis and symptoms severity.
References
UN, World Population Prospects (2017) The 2017 Revision, Key Findings and Advance Tables, in Working Paper No. ESA/P/WP/248. United Nations, Department of Economic and Social Affairs, Population Division
Lyness JM et al (2006) The relationship of medical comorbidity and depression in older, primary care patients. Psychosomatics 47(5):435–439
Laursen TM et al (2016) Mortality and life expectancy in persons with severe unipolar depression. J Affect Disord 193:203–207
Briggs R et al (2018) What is the prevalence of untreated depression and death ideation in older people? Data from the Irish Longitudinal Study on Aging. Int Psychogeriatr 30(9):1393–1401
WHO (2017) Mental health of older adults. https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults
Gottfries CG (2001) Late life depression. Eur Arch Psychiatry Clin Neurosci 251(Suppl 2):II57–II61
Taylor WD, Aizenstein HJ, Alexopoulos GS (2013) The vascular depression hypothesis: mechanisms linking vascular disease with depression. Mol Psychiatry 18(9):963–974
Sunday L et al (2007) Age alters cerebrovascular inflammation and effects of estrogen. Am J Physiol Heart Circ Physiol 292(5):H2333–H2340
Kealy J, Greene C, Campbell M (2018) Blood-brain barrier regulation in psychiatric disorders. Neurosci Lett. https://doi.org/10.1016/j.neulet.2018.06.033
Rothermundt M et al (2001) Different immune patterns in melancholic and non-melancholic major depression. Eur Arch Psychiatry Clin Neurosci 251(2):90–97
Lamers F et al (2016) Serum proteomic profiles of depressive subtypes. Transl Psychiatry 6(7):e851
Bot M et al (2015) Serum proteomic profiling of major depressive disorder. Transl Psychiatry 5:e599
Arnold SE et al (2012) Plasma biomarkers of depressive symptoms in older adults. Transl Psychiatry 2:e65
Schmidt HD, Shelton RC, Duman RS (2011) Functional biomarkers of depression: diagnosis, treatment, and pathophysiology. Neuropsychopharmacology 36(12):2375–2394
Harris VK et al (2013) Cerebrospinal fluid fetuin-A is a biomarker of active multiple sclerosis. Mult Scler 19(11):1462–1472
Chatterjee P et al (2013) Adipocyte fetuin-A contributes to macrophage migration into adipose tissue and polarization of macrophages. J Biol Chem 288(39):28324–28330
Druzhkova T et al (2019) Acute stress response to a cognitive task in patients with major depressive disorder: potential metabolic and proinflammatory biomarkers. Metab Brain Dis 34(2):621–629
Jia C et al (2019) Ciliary neurotrophic factor is a key sex-specific regulator of depressive-like behavior in mice. Psychoneuroendocrinology 100:96–105
Brambilla P et al (2014) Increased M1/decreased M2 signature and signs of Th1/Th2 shift in chronic patients with bipolar disorder, but not in those with schizophrenia. Transl Psychiatry 4:e406
Benedetti F et al (2017) Higher baseline proinflammatory cytokines mark poor antidepressant response in bipolar disorder. J Clin Psychiatry 78(8):e986–e993
Ramsey JM et al (2016) Sex differences in serum markers of major depressive disorder in the netherlands study of depression and anxiety (NESDA). PLoS ONE 11(5):e0156624
Torner L (2016) Actions of prolactin in the brain: from physiological adaptations to stress and neurogenesis to psychopathology. Front Endocrinol (Lausanne) 7:25
Nicholas L, Dawkins K, Golden RN (1998) Psychoneuroendocrinology of depression: prolactin. Psychiatr Clin N Am 21(2):341–358
Gu S et al (2018) Stress induced hormone and neuromodulator changes in menopausal depressive rats. Front Psychiatry 9:253
Ramachandran Pillai R et al (2017) Luteinizing hormone-follicle stimulating hormone ratio as biological predictor of post-partum depression. Compr Psychiatry 72:25–33
Huerta R et al (1995) Symptoms at perimenopausal period: its association with attitudes toward sexuality, life-style, family function, and FSH levels. Psychoneuroendocrinology 20(2):135–148
Harlow BL et al (2003) Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause: the Harvard Study of Moods and Cycles. Arch Gen Psychiatry 60(1):29–36
Carvalho AF et al (2014) Adipokines as emerging depression biomarkers: a systematic review and meta-analysis. J Psychiatr Res 59:28–37
Lu XY (2007) The leptin hypothesis of depression: a potential link between mood disorders and obesity? Curr Opin Pharmacol 7(6):648–652
Dean J, Keshavan M (2017) The neurobiology of depression: an integrated view. Asian J Psychiatr 27:101–111
Pasquali MA et al (2018) A longitudinal study of neurotrophic, oxidative, and inflammatory markers in first-onset depression in midlife women. Eur Arch Psychiatry Clin Neurosci 268(8):771–781
Tsai SJ (2017) Role of tissue-type plasminogen activator and plasminogen activator inhibitor-1 in psychological stress and depression. Oncotarget 8(68):113258–113268
Tsai SJ et al (2008) Plasminogen activator inhibitor-1 gene is associated with major depression and antidepressant treatment response. Pharmacogenet Genom 18(10):869–875
Han C et al (2009) Study design and methods of the Ansan Geriatric Study (AGE study). BMC Neurol 9:10
Park MH et al (2006) No difference in stroke knowledge between Korean adherents to traditional and western medicine—the AGE study: an epidemiological study. BMC Public Health 6:153
Yoo S-W et al (2006) Validity of Korean version of the mini-international neuropsychiatric interview. Anxiety Mood 2:50–55
McGivney SA, Mulvihill M, Taylor B (1994) Validating the GDS depression screen in the nursing home. J Am Geriatr Soc 42(5):490–492
Smarr KL, Keefer AL (2011) Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken) 63(Suppl 11):S454–S466
Mungas D et al (1996) Age and education correction of Mini-Mental State Examination for English and Spanish-speaking elderly. Neurology 46(3):700–706
Lee JH et al (2002) Development of the Korean version of the Consortium to Establish a Registry for Alzheimer's Disease Assessment Packet (CERAD-K): clinical and neuropsychological assessment batteries. J Gerontol B Psychol Sci Soc Sci 57(1):P47–53
Creavin ST et al (2016) Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev (1):CD011145
Dols A et al (2015) BDNF serum levels are not related to cognitive functioning in older depressed patients and controls. Int Psychogeriatr 27(4):649–656
Shin C et al (2019) Increased plasma complement factor H is associated with geriatric depression. Int Psychogeriatr 31(1):101–108
Pan A et al (2008) The association of depressive symptoms with inflammatory factors and adipokines in middle-aged and older Chinese. PLoS ONE 3(1):e1392
Bremmer MA et al (2008) Inflammatory markers in late-life depression: results from a population-based study. J Affect Disord 106(3):249–255
Montorio I, Izal M (1996) The Geriatric Depression Scale: a review of its development and utility. Int Psychogeriatr 8(1):103–112
Eyre HA, Stuart MJ, Baune BT (2014) A phase-specific neuroimmune model of clinical depression. Prog Neuropsychopharmacol Biol Psychiatry 54:265–274
Benjamini Y, Krieger AM, Yekutieli DJB (2006) Adaptive linear step-up procedures that control the false discovery rate. Biometrika 93(3):491–507
Lebreton JP et al (1979) Serum concentration of human alpha 2 HS glycoprotein during the inflammatory process: evidence that alpha 2 HS glycoprotein is a negative acute-phase reactant. J Clin Invest 64(4):1118–1129
Mori K, Emoto M, Inaba M (2011) Fetuin-A: a multifunctional protein. Recent Pat Endocr Metab Immune Drug Discov 5(2):124–146
Heinen MC et al (2018) Fetuin-A protein distribution in mature inflamed and ischemic brain tissue. PLoS ONE 13(11):e0206597
Dabrowska AM et al (2015) Fetuin-A (AHSG) and its usefulness in clinical practice. Review of the literature. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 159(3):352–359
Laughlin GA et al (2014) Fetuin-A, a new vascular biomarker of cognitive decline in older adults. Clin Endocrinol (Oxf) 81(1):134–140
Smith ER et al (2011) Plasma fetuin-A is associated with the severity of cognitive impairment in mild-to-moderate Alzheimer's disease. J Alzheimers Dis 24(2):327–333
Herrmann LL, Goodwin GM, Ebmeier KP (2007) The cognitive neuropsychology of depression in the elderly. Psychol Med 37(12):1693–1702
Melchor JP, Strickland S (2005) Tissue plasminogen activator in central nervous system physiology and pathology. Thromb Haemost 93(4):655–660
Chevilley A et al (2015) Impacts of tissue-type plasminogen activator (tPA) on neuronal survival. Front Cell Neurosci 9:415
Gorska-Ciebiada M et al (2016) Plasma levels of thrombomodulin, plasminogen activator inhibitor-1 and fibrinogen in elderly, diabetic patients with depressive symptoms. Aging Clin Exp Res 28(5):843–851
von Känel R et al (2001) Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease? Psychosom Med 63(4):531–544
Fanelli G et al (2019) Reduced CXCL1/GRO chemokine plasma levels are a possible biomarker of elderly depression. J Affect Disord 249:410–417
Swiatkowska M, Szemraj J, Cierniewski CS (2005) Induction of PAI-1 expression by tumor necrosis factor alpha in endothelial cells is mediated by its responsive element located in the 4G/5G site. FEBS J 272(22):5821–5831
Jeon H et al (2012) Plasminogen activator inhibitor type 1 regulates microglial motility and phagocytic activity. J Neuroinflamm 9:149
Ajjan R et al (2007) Ethnic differences in cardiovascular risk factors in healthy Caucasian and South Asian individuals with the metabolic syndrome. J Thromb Haemost 5(4):754–760
McCartney CR, Marshall JC (2019) Neuroendocrinology of reproduction. In: Barbieri RL, Strauss III JF (eds) Yen & Jaffe’s reproductive endocrinology: physiology, pathophysiology, and clinical management. Elsevier
Saletu B et al (1995) Double-blind, placebo-controlled, hormonal, syndromal and EEG mapping studies with transdermal oestradiol therapy in menopausal depression. Psychopharmacology 122(4):321–329
Schmidt PJ et al (2002) Basal plasma hormone levels in depressed perimenopausal women. Psychoneuroendocrinology 27(8):907–920
Young EA et al (2000) Alteration in the hypothalamic-pituitary-ovarian axis in depressed women. Arch Gen Psychiatry 57(12):1157–1162
Freeman EW et al (2006) Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry 63(4):375–382
Ryan J et al (2009) A prospective study of the association between endogenous hormones and depressive symptoms in postmenopausal women. Menopause 16(3):509–517
Rubin RT, Poland RE, Lesser IM (1989) Neuroendocrine aspects of primary endogenous depression VIII. Pituitary-gonadal axis activity in male patients and matched control subjects. Psychoneuroendocrinology 14(3):217–229
Andre C et al (2018) mTORC1 pathway disruption abrogates the effects of the ciliary neurotrophic factor on energy balance and hypothalamic neuroinflammation. Brain Behav Immun 70:325–334
Lin HW et al (2009) Ciliary neurotrophic factor (CNTF) plus soluble CNTF receptor alpha increases cyclooxygenase-2 expression, PGE2 release and interferon-gamma-induced CD40 in murine microglia. J Neuroinflamm 6:7
Lee TI et al (2009) Role of ciliary neurotrophic factor in microglial phagocytosis. Neurochem Res 34(1):109–117
Carrillo-de Sauvage MA et al (2015) The neuroprotective agent CNTF decreases neuronal metabolites in the rat striatum: an in vivo multimodal magnetic resonance imaging study. J Cereb Blood Flow Metab 35(6):917–921
Peruga I et al (2012) Endogenous ciliary neurotrophic factor modulates anxiety and depressive-like behavior. Behav Brain Res 229(2):325–332
Beumer W et al (2012) The immune theory of psychiatric diseases: a key role for activated microglia and circulating monocytes. J Leukoc Biol 92(5):959–975
Wang H et al (2010) Peripheral administration of fetuin-A attenuates early cerebral ischemic injury in rats. J Cereb Blood Flow Metab 30(3):493–504
Kahn MA et al (1995) CNTF regulation of astrogliosis and the activation of microglia in the developing rat central nervous system. Brain Res 685(1–2):55–67
Setiawan E et al (2015) Role of translocator protein density, a marker of neuroinflammation, in the brain during major depressive episodes. JAMA Psychiatry 72(3):268–275
Mechawar N, Savitz J (2016) Neuropathology of mood disorders: do we see the stigmata of inflammation? Transl Psychiatry 6(11):e946
Cavaillon JM (2001) Pro- versus anti-inflammatory cytokines: myth or reality. Cell Mol Biol (Noisy-le-grand) 47(4):695–702
Wohleb ES (2016) Neuron–microglia interactions in mental health disorders: “for better, and for worse”. Front Immunol 7:544
Busse M et al (2015) Decreased quinolinic acid in the hippocampus of depressive patients: evidence for local anti-inflammatory and neuroprotective responses? Eur Arch Psychiatry Clin Neurosci 265(4):321–329
Diniz BS et al (2010) Serum brain-derived neurotrophic factor level is reduced in antidepressant-free patients with late-life depression. World J Biol Psychiatry 11(3):550–555
Shi Y et al (2010) Plasma BDNF and tPA are associated with late-onset geriatric depression. Psychiatry Clin Neurosci 64(3):249–254
Ziegenhorn AA et al (2007) Serum neurotrophins—a study on the time course and influencing factors in a large old age sample. Neurobiol Aging 28(9):1436–1445
Bocchio-Chiavetto L et al (2010) Serum and plasma BDNF levels in major depression: a replication study and meta-analyses. World J Biol Psychiatry 11(6):763–773
Rosenfeld RD et al (1995) Purification and identification of brain-derived neurotrophic factor from human serum. Protein Expr Purif 6(4):465–471
Tsuchimine S et al (2014) Preanalysis storage conditions influence the measurement of brain-derived neurotrophic factor levels in peripheral blood. Neuropsychobiology 69(2):83–88
Corona G et al (2014) Low prolactin is associated with sexual dysfunction and psychological or metabolic disturbances in middle-aged and elderly men: the European Male Aging Study (EMAS). J Sex Med 11(1):240–253
Prabhakar VK, Davis JR (2008) Hyperprolactinaemia. Best Pract Res Clin Obstet Gynaecol 22(2):341–353
Urban RJ, Veldhuis JD (1991) A selective serotonin reuptake inhibitor, fluoxetine hydrochloride, modulates the pulsatile release of prolactin in postmenopausal women. Am J Obstet Gynecol 164(1 Pt 1):147–152
Peeters F et al (2006) Diurnal mood variation in major depressive disorder. Emotion 6(3):383–391
Leyhe T et al (2017) A common challenge in older adults: Classification, overlap, and therapy of depression and dementia. Alzheimers Dement 13(1):59–71
Acknowledgements
This study was supported by a grant from the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (Grant Number: HC15C1405).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Prof. Alessandro Serretti is/has been consultant/speaker for Abbott, Abbvie, Angelini, Astra Zeneca, Clinical Data, Boheringer, Bristol Myers Squibb, Eli Lilly, GlaxoSmithKline, Innovapharma, Italfarmaco, Janssen, Lundbeck, Naurex, Pfizer, Polifarma, Sanofi, and Servier. The other authors declare no potential conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fanelli, G., Benedetti, F., Wang, SM. et al. Reduced plasma Fetuin-A is a promising biomarker of depression in the elderly. Eur Arch Psychiatry Clin Neurosci 270, 901–910 (2020). https://doi.org/10.1007/s00406-019-01090-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-019-01090-1