Abstract
Cognitive deficits are increasingly recognized as a core dimension rather than a consequence of schizophrenia (SCZ). The previous evidence supports the hypothesis of shared genetic factors between SCZ and cognitive ability. The objective of this study was to test whether and to what extent the variation of disease-relevant neurocognitive function in a sample of SCZ patients from the previous clinical interventional studies can be explained by SCZ polygenic risk scores (PRSs) or by hypothesis-driven and biomedical PRSs. The previous studies have described associations of the SNAP25 gene with cognition in SCZ. Likewise, the enrichment of several calcium signaling-related gene sets has been reported by genome-wide association studies (GWAS) in SCZ. Hypothesis-driven PRSs were calculated on the basis of the SNAP-25 interactome and also for genes regulated by phorbol myristate acetate (PMA), an activator of the signal transduction of protein kinase C (PKC) enzymes. In a cohort of 127 SCZ patients who had completed a comprehensive neurocognitive test battery as part of the previous antipsychotic intervention studies, we investigated the association between neurocognitive dimensions and PRSs. The PRS for SCZ and SNAP-25-associated genes could not explain the variance of neurocognition in this cohort. At a p value threshold of 0.05, the PRS for PMA was able to explain 2% of the variance in executive function (p = 0.05, uncorrected). The correlation between the PRS for PMA-regulated genes and cognition can give hints for further patient-derived cellular assays. In conclusion, incorporating biological information into PRSs and other en masse genetic analyses may help to close the gap between genetic vulnerability and the biological processes underlying neuropsychiatric diseases such as SCZ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia (SCZ) is a severe psychiatric disease that affects up to 1% of the worldwide population [1] and has a high heritability, estimated to be between 60 and 80% [2, 3]. Although the full picture of genetic risk is still unknown, genome-wide association studies (GWAS) based on ever larger samples of patients have currently identified 108 loci that very likely contribute to SCZ risk [4]. One of the main conclusions of this study was that the genetic architecture of SCZ is rather polygenic and involves the combined contribution of hundreds to thousands of genetic variants [4, 5]. Polygenic risk scores (PRSs) summarize the weighted effect of genetic risk variants discovered by GWAS in a single individual score [6]. SCZ PRSs have been shown to explain a considerable amount of variation in case/control status, and they are characterized by a remarkable replicability in independent samples [4]. These results raised high hopes for a breakthrough in understanding the connection between genetic burden, key symptoms, and potential biological mechanisms underlying the SCZ phenotype.
Even though the classification of SCZ has changed over the years, including in the diagnostic manuals for psychiatric disorders, the following are consistent key symptoms: positive symptoms, e.g., delusions and hallucinations; negative symptoms, e.g., avolition, alogia, and anhedonia; and cognitive deficits. Cognitive deficits often occur before the onset of the first psychotic episode and seem to remain stable over the course of the disease and to be refractory to antipsychotic treatment [7]. They can be measured and assessed objectively by systematic neuropsychological panels. Deficits in cognition are strong predictors for the functionality of patients in everyday life and can lead to severe impairments [8]. However, the causal relationship between symptoms of SCZ and cognitive impairment remains unclear [9]. Family-based studies have raised the question of genetic overlap and covariance between cognitive functions and SCZ [10]. Several studies have examined the influence of SCZ PRSs on cognition [11]. The first reports found that SCZ PRSs were associated with a lower general cognitive ability in SCZ patients [12]. The relationship between SCZ PRSs and childhood cognitive abilities was also investigated in population-based samples: in this population, SCZ PRS was associated with lower performance IQ and lower full IQ. In addition, vice versa, the PRS for performance IQ was associated with increased risk for SCZ [13]. Likewise, another study reported an association of SCZ polygenic risk with reduced speed of emotion identification and verbal reasoning by age 9 years in a healthy population aged 8–21 years [14]. A higher PRS for SCZ was also associated with decreased cognitive function in healthy older adults [15]. More recently, in a sample that included SCZ patients, relatives, and healthy controls, a higher PRS was associated with poorer performance on the block design task [16]. Some studies have already explored the influence of biologically informed PRSs on cognition. Nicodemus et al. [17] investigated the variation of neuropsychological function explained by PRSs for SCZ and pathway-informed risk scores in a patient cohort: In a sample of 424 patients, they found an association between higher PRSs for SCZ and poorer performance on IQ, memory, and social cognition, explaining 1%-3% of variation. A two-single-nucleotide polymorphism (SNP) epistatic component of the ZNF804A pathway increased the explained variation up to 4.8% [17]. A more recent study generated an MiR-137–derived PRS that was associated with significantly lower performance on IQ, working memory, and episodic memory in a combined sample of SCZ patients and healthy controls [18].
Many aspects of the strategy of analyzing pathway-dependent risk scores are interesting. Compared with the mere SCZ PRSs or PRSs driven by clinical symptoms, pathway-dependent risk scores can include and test knowledge derived from molecular biology research results, give valuable hints about a molecular or cellular follow-up model, and focus on specific pathways of interest. Especially, in neuropsychiatric research, cellular models such as human-induced pluripotent stem cell (hiPSC)-based studies have become increasingly important to test hypotheses and understand underlying mechanisms that lead to new drug discoveries [19]. Molecular stimuli are usually used to test cellular responses and the function of intra- and intercellular communication, such as signaling pathways. Phorbol myristate acetate (PMA) is a typical stimulus for testing immune response, calcium-dependent signaling, and proliferation pathways in cellular assays. All of these mechanisms have also been identified by GWAS as being affected in patients with schizophrenia. We decided to focus on PMA-regulated genes and on those genes encoding for the SNAP-25 first-order interactome. PMA is a diester of phorbol and often used as an activator of the signal transduction of protein kinase C (PKC) enzymes in biomedical research. PMA models the effect of intracellular calcium-mediated activation of PKC. In addition, it is commonly used as an immune modulator for lymphocyte activation and proliferation and cytokine production [20]. Further downstream, it signals through the mitogen-activated protein kinase (MAPK) and extracellular signal-regulated kinase (ERK) pathways, which involves the activation of immediate early genes [21]. An increasing body of evidence indicates the involvement of calcium signaling and immune regulation in the development of SCZ [4, 22].
The previous work from our group has shown the involvement of genetic variability in the SNAP25 gene (20p12.2) in determining the cognitive profile of the sample included in this study [23]. In this cohort, we observed a significant relation between the DdeI polymorphism of the SNAP25 gene and cognitive dysfunctions. Specifically, rs1051312 SNP, located in the 3′UTR region of this gene, was found to be associated with performance in verbal memory and executive functions [23]. SNAP-25 plays a key role in neurotransmitter release from the presynapses into the synaptic cleft through its involvement in the docking of vesicles and their subsequent fusion with the presynaptic membrane [24, 25]. The previous studies have also shown the role of this gene in the cognitive performance observed in psychiatric patients and the healthy population [26]. To our knowledge, however, so far, no joint analysis of all those genes that constitute the first-order interactome of SNAP-25 has been performed as regards the cognitive performance of SCZ patients.
Here, we tested whether the global SCZ PRS or the hypothesis-driven PRSs based on either PMA-regulated genes or the SNAP-25 interactome are associated with the performance of SCZ patients in cognitive tasks. The main objective was to test whether and to what extent the variation of disease-relevant neurocognitive function in SCZ patients of a clinical interventional study cohort can be explained by a global estimate of SCZ risk or by hypothesis-driven estimates of risk potentially closer to SCZ pathophysiology and cognitive dysfunction.
Materials and methods
Participants
The recruited cohort consisted of 127 SCZ patients from antipsychotic intervention studies [mean (SD) age: 32.98 (10.88) years; mean (SD) age of onset: 28.13 (9.73); female: 40.5%] [27,28,29]. Outpatients and hospitalized patients with a DSM-IV diagnosis of schizophrenia, schizoaffective disorder, or psychotic disorder not otherwise specified were eligible for the study. Participants were assessed by the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), and the diagnosis was established by two independent psychiatrists. Only patients with a Clinical Global Impression Severity Scale (CGI-S) score ≥ 4 [30] and a Positive and Negative Symptom Scale (PANSS) score ≥ 60 were included [31]. The patients were participants in different randomized, double-blind, parallel-group or open-label studies and assigned to monotherapy with an antipsychotic [27, 28]. The neurocognitive tests and genotyping were conducted after a 2- to 7-day wash-out period and before inclusion in the interventional studies. Consequently, the patients’ participation in these studies did not affect the results of the present study. Exclusion criteria were substance abuse, dependence, or intoxication; suicidal tendencies; significant medical history (head trauma, epilepsy, meningoencephalitis); ECG or EEG abnormalities; severe abnormalities (≥ 20% difference from reference ranges) in laboratory blood and urine testing; pregnancy or lactation; treatment with clozapine within 4 weeks before enrollment. All patients gave written informed consent according to the procedures of the ethics committee of the medical faculty of the Ludwig Maximilian University, Munich that approved the study. The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its latest amendment in 2008 (WMA General Assembly, Seoul, Korea, October 2008).
Neurocognitive tests
The neurocognitive tests performed in the antipsychotic intervention studies covered working memory, verbal memory, reaction time and quality, executive functions, and visual memory (Table 1). The entire test battery took between 90 and 120 min to complete. The global cognitive index was calculated by first summing the individual neurocognitive results and then transforming them into z scores. The neurocognitive test battery was administered before the study intervention. Premorbid intelligence was tested by the multiple choice word test-B (MWT-B) [32]. The results of this vocabulary test correlate with “crystallized intelligence” and are thought to remain stable during adulthood and to be independent of current psychopathological alterations. Working memory was assessed with the Rey Auditory Verbal Learning Test (RAVLT) [33] lists 1 and 2, the Letter–Number Span, and the Self-Ordered Pointing Task (SOPT) [34], and verbal memory with the RAVLT lists 1–5, 6, and 7. Reaction time was measured by Neurobat-S (part for reaction time) [35] and the Trail Making Test [36], and reaction quality by Neurobat-S (sensorimotor function) and duration of attention. Executive functions were evaluated by testing verbal fluency and using the Trail Making Test-B. Visual memory was assessed with the Wechsler Memory Scale-Revised [37] and the Spatial Working Memory test.
Genotyping and quality control
Genomic DNA was isolated from whole blood by the following standard procedures. The patient samples were genotyped with the Infinium PsychArray Bead-Chip (Illumina®). Quality control steps (SNP call rate > 97%, subject call rate > 95%, Hardy–Weinberg equilibrium > 10− 6, and heterozygosity rate within 3 standard deviations) were carried out with PLINK 1.9. After quality control, ~ 300,000 SNPs covering the whole genome were ready for analyses. We calculated an identity-by-state (IBS) matrix to estimate the relationship between all the samples, which turned out to be non-related (all PI-HAT < 0.2). With the EIGENSOFT package (SmartPCA), we modeled ancestry differences between the study participants using a principal component analysis based on a pruned subset of ~ 50,000 autosomal SNPs, after excluding high-LD regions [38]. All participants clustered to HapMap3 Caucasian reference populations, so none of them was excluded in subsequent analyses. We extracted the first 4 ancestry principal components to correct for the potential effects of population substructure in all analyses.
Imputation
Genotype imputation in these samples was performed with IMPUTE2/SHAPEIT using its pre-phasing and imputation pipeline [39, 40]. The 1000 Genomes Project data set (Phase 3 integrated variant set) was used as the reference panel. Those genetic variants with a poor imputation quality (INFO < 0.7) were excluded in downstream analyses.
Scoring
Using the most recent summary statistics on SCZ GWAS from the Psychiatric Genomics Consortium as the discovery sample, we calculated PRSs in our study samples. PRSs were calculated at 5 different p value cut-offs (5 × 10− 8, 1 × 10− 5, 0.05, 0.1, 0.5). Secondary high-resolution scoring involved the calculation of PRSs at additional p value cut-offs (5 × 10− 8 to 0.6). PRSs were calculated by multiplying the imputation dosage for each risk allele by the log(OR) for each genetic variant. The resulting values were summed to obtain an individual estimate of the SCZ genetic burden in each individual across the different p value thresholds.
The aforementioned scoring was based on three different approaches: (1) whole-genome schizophrenia risk scores, (2) scores based only on those genes (n = 484) regulated by PMA, and (3) scores based only on those genes that constitute the first-order interactome of SNAP-25 (n = 21). As a result, three different sets of polygenic scores (whole genome-, PMA-, and SNAP25-based) were available for each patient in the study.
Definition of PMA-regulated and SNAP-25 interactome gene sets
PMA-induced genes were extracted from the drug signatures database (DSigDB), a collection of drug and small molecule-related gene sets based on quantitative inhibition and/or drug-induced gene expression changes from various databases and evidence in the literature [41].
Protein–protein interactions were queried with the NetworkAnalyst Software from the STRING protein–protein interaction database with a confidence score cut-off of 900 and filtered for experimental data evidence [42]. The final list of genes included in both gene sets is provided in Supplementary Data 1.
Statistical analyses
Analyses were based on the six phenotypes mentioned above, namely working memory, verbal memory, reaction time and quality, executive functions, and visual memory. Standardized values of these cognitive variables were used as dependent variables in a linear regression model. Age, age2, sex, and four population ancestry principal components were used as covariates. R2 values derived from a model including all of these covariates were subtracted from R2 values from a model including covariates plus the respective PRS. The difference between the adjusted R2 values represented the increase in the variance explained attributable to the PRS.
Results
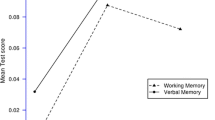
The association of three different PRSs with neurocognitive items was evaluated in the sample of patients included in this study. The total SCZ PRS was not associated with any of the cognitive items measured in these patients (p > 0.05, Supplementary Fig. 1, and Supplementary Table 1). Likewise, the association analysis between the PRS calculated on the basis of SNAP-25–interacting proteins and cognitive functions did not yield any significant results (p > 0.05, Supplementary Fig. 2 and Supplementary Table 2). However, the PRS based on PMA-regulated genes showed a borderline association with executive function: At a p value threshold of 0.05, the PRS for PMA could explain 2% of the variance of the executive function [p = 0.05 (uncorrected), Table 1, Supplementary Fig. 3]. High-resolution analysis at additional p value cut-offs (from 5 × 10− 8 to 0.06) yielded a stable profile and significant correlation between the PRS based on PMA-regulated genes and executive function across several p value thresholds (0.02 through 0.05, Supplementary Fig. 4). It should be noted, however, that including premorbid intelligence as a covariate eliminated these significant effects. The other cognitive domains, i.e., verbal memory, reaction time, reaction quality, working memory, and visual memory, were not explained by the PRS for PMA-regulated genes.
Discussion
We used three different PRSs to investigate whether neurocognitive function could be explained by genetic risk variants or functionally relevant groups of genes in a cohort of 127 SCZ patients who had completed a comprehensive neurocognitive test battery as part of antipsychotic intervention studies. Our hypothesis was that using a selected list of genes for the construction of biologically informed PRSs could increase the chance of finding an association between genetic risk variants and neurocognitive function. Even though a correlation between SCZ PRSs and neurocognition has been previously described in several cohorts [11], however, in our cohort, the SCZ PRSs could not explain the variance in any of the cognitive items tested.
First, we tested those genes that constitute the first-order interactome of SNAP-25, because, in a previous publication of our group, a Ddel polymorphism at SNAP-25 was associated with the cognitive performance of the SCZ patients in our cohort. However, this biologically informed SNAP-25 PRS could not explain the variance in cognitive function in our cohort of patients. In addition, we ascertained the influence of a PRS based on the genes regulated by PMA on the cognitive performance in our cohort. Such a PRS based on PMA-regulated genes adds a “biological focus” to the polygenic risk estimate. PMA is frequently used in in vitro assays to activate the immune response, immediate early genes, and calcium signaling [43]. All these mechanisms involve pathways that have been discussed as highly relevant for the development of schizophrenia. Our results suggest that, in our cohort, the PRS for PMA-regulated genes can explain a certain proportion of the variance in executive function (2%). This result was specific for executive function, while the other cognitive domains were not correlated with this PRS. Studies have not yet determined whether executive dysfunction in SCZ is specifically related to immune pathways, immediate early gene regulation, or calcium signaling. The polygenic effects of the PMA PRS focus on those genetic variants with a p value of about 0.05 in the large SCZ GWAS. The fact that polygenic scores based on a genome-wide threshold did not yield significant associations with cognition suggests that those genetic variants associated with cognition in SCZ are not necessarily those with a major contribution to SCZ risk.
Our study in 127 patients might be underpowered to identify the further effects of polygenic risk on other cognitive domains. Likewise, our limited sample size requires further studies to confirm the validity of our results. Another limitation of our study is that none of the associations will hold significant after correction for multiple testings. Furthermore, it remains to be investigated whether the PRS for PMA-regulated genes is associated only with executive function or whether it might be associated with a generalized cognitive dysfunction in these patients.
The correlation between the PRS for PMA-regulated genes and cognition may be an important basis for further patient-derived cellular assays. Of great interest is whether PMA stimulation can provoke differentiated profiles in cells of SCZ patients. This could help to identify disease-relevant pathways and pathomechanisms that could be addressed by novel drugs. In conclusion, incorporating biological information into PRSs and other en masse genetic analyses may help to close the gap between genetic vulnerability and the biological processes underlying neuropsychiatric diseases such as SCZ.
References
McGrath J, Saha S, Chant D, Welham J (2008) Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 30:67–76
Sullivan PF, Kendler KS, Neale MC (2003) Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry 60:1187–1192
Lichtenstein P, Yip BH, Björk C, Pawitan Y, Cannon TD, Sullivan PF et al (2009) Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet 373:234–239
Schizophrenia Working Group of the Psychiatric Genomics Consortium (2014) Biological insights from 108 schizophrenia-associated genetic loci. Nature 511:421–427
Neale BM, Sklar P (2015) Genetic analysis of schizophrenia and bipolar disorder reveals polygenicity but also suggests new directions for molecular interrogation. Curr Opin Neurobiol 30:131–138
Maier RM, Visscher PM, Robinson MR, Wray NR (2017) Embracing polygenicity: a review of methods and tools for psychiatric genetics research. Psychol Med 2017:1–19
Albus M, Hubmann W, Mohr F, Hecht S, Hinterberger-Weber P, Seitz N-N et al (2006) Neurocognitive functioning in patients with first-episode schizophrenia: results of a prospective 5-year follow-up study. Eur Arch Psychiatry Clin Neurosci 256:442–451
Green MF (2006) Cognitive impairment and functional outcome in schizophrenia and bipolar disorder. J Clin Psychiatry 67:e12
Gottesman II, Gould TD (2003) The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160:636–645
Toulopoulou T, Picchioni M, Rijsdijk F, Hua-Hall M, Ettinger U, Sham P et al (2007) Substantial genetic overlap between neurocognition and schizophrenia: genetic modeling in twin samples. Arch Gen Psychiatry 64:1348–1355
Mistry S, Harrison JR, Smith DJ, Escott-Price V, Zammit S (2018) The use of polygenic risk scores to identify phenotypes associated with genetic risk of bipolar disorder and depression: a systematic review. J Affect Disord 234:148–155. https://doi.org/10.1016/j.jad.2018.02.005
Lencz T, Knowles E, Davies G, Guha S, Liewald DC, Starr JM et al (2014) Molecular genetic evidence for overlap between general cognitive ability and risk for schizophrenia: a report from the Cognitive Genomics consorTium (COGENT). Mol Psychiatry 19:168–174
Hubbard L, Tansey KE, Rai D, Jones P, Ripke S, Chambert KD et al (2016) Evidence of common genetic overlap between schizophrenia and cognition. Schizophr Bull 42:832–842
Germine L, Robinson EB, Smoller JW, Calkins ME, Moore TM, Hakonarson H et al (2016) Association between polygenic risk for schizophrenia, neurocognition and social cognition across development. Transl Psychiatry 6:e924
Liebers DT, Pirooznia M, Seiffudin F, Musliner KL, Zandi PP, Goes FS (2016) Polygenic risk of schizophrenia and cognition in a population-based survey of older adults. Schizophr Bull 42:984–991
Ranlund S, Calafato S, Thygesen JH, Lin K, Cahn W, Crespo-Facorro B et al (2018) A polygenic risk score analysis of psychosis endophenotypes across brain functional, structural, and cognitive domains. Am J Med Genet B Neuropsychiatr Genet 177:21–34
Nicodemus KK, Hargreaves A, Morris D, Anney R, Gill M, Corvin A et al (2014) Variability in working memory performance explained by epistasis versus polygenic scores in the ZNF804A pathway. JAMA Psychiatry 71:778–785
Cosgrove D, Harold D, Mothersill O, Anney R, Hill MJ, Bray NJ et al (2017) MiR-137-derived polygenic risk: effects on cognitive performance in patients with schizophrenia and controls. Transl Psychiatry 7:e1012
Schadt EE, Buchanan S, Brennand KJ, Merchant KM (2014) Evolving toward a human-cell based and multiscale approach to drug discovery for CNS disorders. Front Pharmacol 5:252
Hara T, Fu SM (1985) Human T cell activation. I. Monocyte-independent activation and proliferation induced by anti-T3 monoclonal antibodies in the presence of tumor promoter 12-o-tetradecanoyl phorbol-13 acetate. J Exp Med 161:641–656
Kast C, Wang M, Whiteway M (2003) The ERK/MAPK pathway regulates the activity of the human tissue factor pathway inhibitor-2 promoter. J Biol Chem 278:6787–6794
Hertzberg L, Katsel P, Roussos P, Haroutunian V, Domany E (2015) Integration of gene expression and GWAS results supports involvement of calcium signaling in Schizophrenia. Schizophr Res 164:92–99
Spellmann I, Müller N, Musil R, Zill P, Douhet A, Dehning S et al (2008) Associations of SNAP-25 polymorphisms with cognitive dysfunctions in Caucasian patients with schizophrenia during a brief trail of treatment with atypical antipsychotics. Eur Arch Psychiatry Clin Neurosci 258:335–344
Jahn R, Scheller RH (2006) SNAREs–engines for membrane fusion. Nat Rev Mol Cell Biol 7:631–643
Washbourne P, Thompson PM, Carta M, Costa ET, Mathews JR, Lopez-Benditó G et al (2002) Genetic ablation of the t-SNARE SNAP-25 distinguishes mechanisms of neuroexocytosis. Nat Neurosci 5:19–26
Braida D, Guerini FR, Ponzoni L, Corradini I, De Astis S, Pattini L et al (2015) Association between SNAP-25 gene polymorphisms and cognition in autism: functional consequences and potential therapeutic strategies. Transl Psychiatry 5:e500
Riedel M, Müller N, Spellmann I, Engel RR, Musil R, Valdevit R et al (2007) Efficacy of olanzapine versus quetiapine on cognitive dysfunctions in patients with an acute episode of schizophrenia. Eur Arch Psychiatry Clin Neurosci 257:402–412
Riedel M, Müller N, Strassnig M, Spellmann I, Engel RR, Musil R et al (2005) Quetiapine has equivalent efficacy and superior tolerability to risperidone in the treatment of schizophrenia with predominantly negative symptoms. Eur Arch Psychiatry Clin Neurosci 255:432–437
Musil R, Spellmann I, Riedel M, Dehning S, Douhet A, Maino K et al (2008) SNAP-25 gene polymorphisms and weight gain in schizophrenic patients. J Psychiatr Res 42:963–970
Busner J, Targum SD (2007) The clinical global impressions scale. Psychiatry (Edgmont) 4:28–37
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276
Lehrl S, Triebig G, Fischer B (1995) Multiple choice vocabulary test MWT as a valid and short test to estimate premorbid intelligence. Acta Neurol Scand 91:335–345
Bleecker ML, Bolla-Wilson K, Agnew J, Meyers DA (1988) Age-related sex differences in verbal memory. J Clin Psychol 44(3):403–411
Petrides M, Milner B (1982) Deficits on subject-ordered tasks after frontal- and temporal-lobe lesions in man. Neuropsychologia 20:249–262
Möller H-J, Engel RR, Hoff P (2013) Befunderhebung in der Psychiatrie: Lebensqualität, Negativsymptomatik und andere aktuelle Entwicklungen. Springer, Berlin
Corrigan JD, Hinkeldey NS (1987) Relationships between parts A and B of the trail making test. J Clin Psychol 43(4):402–409
Wechsler Adult Intelligence Scale-Fourth Edition [Internet] (2018) https://www.pearsonclinical.com/psychology/products/100000392/wechsler-adult-intelligence-scalefourth-edition-wais-iv.html?Pid=015-8980-808. Accessed 27 Aug 2018
Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D (2006) Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet 38:904–909
Howie BN, Donnelly P, Marchini J (2009) A flexible and accurate genotype imputation method for the next generation of genome-wide association studies. PLoS Genet 5:e1000529
Delaneau O, Zagury J-F, Marchini J (2013) Improved whole-chromosome phasing for disease and population genetic studies. Nat Methods 10:5–6
Yoo M, Shin J, Kim J, Ryall KA, Lee K, Lee S et al (2015) DSigDB: drug signatures database for gene set analysis. Bioinformatics 31:3069–3071
Xia J, Gill EE, Hancock REW (2015) NetworkAnalyst for statistical, visual and network-based meta-analysis of gene expression data. Nat Protocols 10:823–844
Castagna M, Takai Y, Kaibuchi K, Sano K, Kikkawa U, Nishizuka Y (1982) Direct activation of calcium-activated, phospholipid-dependent protein kinase by tumor-promoting phorbol esters. J Biol Chem 257:7847–7851
Acknowledgements
We would like to thank all patients for participating in this study and Jacquie Klesing, Board-certified Editor in the Life Sciences (ELS), for editing assistance with the manuscript. SP is supported by a 2016 NARSAD Young Investigator Grant (25015) from the Brain & Behavior Research Foundation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author(s) state that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kirchner, S.K., Ozkan, S., Musil, R. et al. Polygenic analysis suggests the involvement of calcium signaling in executive function in schizophrenia patients. Eur Arch Psychiatry Clin Neurosci 270, 425–431 (2020). https://doi.org/10.1007/s00406-018-0961-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-018-0961-8