Abstract
Little is known about guideline adherence of naturalistic antidepressant drug therapy in outpatients with major depressive disorder (MDD). The aim of the study was to analyze guideline adherence, especially regarding treatment length, treatment evaluation and medication change strategies. We investigated 889 patients with MDD who had been admitted for inpatient treatment and were enrolled in the early medication change trial (ClinicalTrials.gov NCT00974155). We investigated all patients at screening visit regarding previous outpatient drug treatment in the index episode, which was assessed by structured interviews. Demographic variables were obtained from patients and patients’ records. 51.0% of the patients had received previous drug treatment in the index episode, 56.6% were females, and their mean age was 40.0 years. In the 153 patients who were pharmacologically treated at least 8 weeks, medication was not changed in 129 (84.3%) patients. Patients who had a medication change in their index episode (n = 24, 15.7%) waited 71.1 weeks (±110.4) for their treatment optimization. Only 5 of those 153 patients (3.3%) had a dose increase, whereas 132 patients (86.3%) had no dose adaption at all. Antidepressant blood levels were measured in 46 patients (30.1%). We conclude that a large proportion of patients with MDD is not treated in adherence to treatment guidelines recommending treatment evaluation (e.g. therapeutic drug monitoring) and treatment change after 4 to 8 weeks in non-responders. Earlier treatment optimization may prevent long-term suffering of patients and may avoid inpatient treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is a severe, prevalent, and highly important mental illness [1–3]. It is the most abundant mental disorder affecting around 350 million people worldwide and the World Health Organization considers it being a leading cause of disability worldwide [4]. In addition, it is the most costly brain disorder in total Europe [2].
Standard MDD treatment includes pharmacological therapy using antidepressant drugs and psychotherapy [5–7]. Treatment guidelines formulate clear recommendations for MDD therapy. Clinicians are recommended to act according to these documents, such as the ‘German National Clinical Practice Guideline for Unipolar Depression’ [6] which is recommended for German physicians, the American Psychiatric Association ‘Practice Guideline for the Treatment of Patients With Major Depressive Disorder’ [7], or the National Institute for Health and Care Excellence guideline ‘Depression in Adults’ [5], to name three important current guidelines.
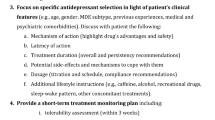
Although these guidelines vary in several aspects, the recommendations regarding antidepressant dose, treatment duration until treatment evaluation and change, and treatment change strategies are quite comparable (Table 1) [5–7]: all guidelines recommend after a certain time period (3–8 weeks) and dissatisfying response a first treatment evaluation which includes several aspects: Assurance of patient’s adherence, performance of therapeutic drug monitoring, and reevaluation of the diagnosis. If all these steps fail, guidelines recommend performing treatment change strategies, which includes consideration of dose increases, augmentation strategies, combination strategies, and medication switch strategies. The detailed recommendations of the three guidelines can be seen in Table 1.
Studies in the field of guideline adherence and implementation can treat with either provider performance or patients’ outcomes or both. As guideline adherence strongly depends on the treating physicians’ actions, it was our rationale to exclusively focus on provider performance in the present study. Previous studies [8–15] assessing MDD treatment quality and guideline adherence of treatment focused on MDD diagnosis and recognition, outpatient under-treatment, differences between general practitioners (GPs) and specialists’ treatment, relapse prevention, and adherence to continuous antidepressant treatment. In a study with more than 4000 participants, 52% of the patients were adherent to antidepressant treatment in the acute phase, and 42% in the continuation phase [8]. In a Spanish sample of 133 patients, similar proportions for minimally adequate antidepressant treatment was achieved in ~31% of the patients treated by GPs and specialists as well [9]. Using the IMS LifeLink Health Plan Database with 134,287 antidepressant-prescribed patients, 23.2% of them reported a treatment change, most commonly an antidepressant switch (9.5%) or combination (9.1%) [10]. Nevertheless, this study analyzed the median overall treatment duration (111 days), but did not reveal information focusing on treatment duration until treatment change. Radisch et al. analyzed problems concerning the routine treatment of outpatients with MDD in Germany [11]. They showed that primary care treatment lacked knowledge of National Practice guidelines and that many patients fear taking antidepressants due to social and society’s prejudices. GPs rather prescribed old and known antidepressants, in contrast to new, but guideline-recommended drugs. A previous study of Schneider et al. showed that approximately half of the 488 patients reported a stagnation or even a progression of depressive symptoms during outpatient treatment [13]. In contrast, inpatient treatment is known to achieve a clearly higher quality level and guideline adherence [12]. In primary care, as well as in inpatient settings, antidepressant drug dose is reported to be mainly guideline-adherent [8–10, 14, 15]. Pharmacological treatment duration was nearly exclusively analyzed in terms of continuous antidepressant treatment after remission. Little is known, however, about guideline adherence of outpatient treatment in a naturalistic setting. At least to our knowledge, there are no studies regarding length of pharmacological treatment and pharmacological treatment change in case of non-response. This lack of information prompted us to analyze these factors in a large sample of patients with MDD who were admitted for inpatient treatment and participated in the Early Medication Change (EMC) trial [16].
Methods
Participants
The herein presented study was designed as an additional, secondary analysis to the “Randomized clinical trial comparing an early medication change (EMC) strategy with treatment as usual (TAU) in patients with MDD—The EMC Trial (ClinicalTrials.gov identifier No: NCT00974155)”. Details of the protocol for this study including in-/exclusion criteria and study procedures [16] have been described previously. In brief, the EMC trial was a multi-center, randomized, observer-blinded, controlled clinical trial investigating whether non-improvers after 14 days of an escitalopram treatment are more likely to attain remission (HAMD-17 ≤7) on treatment day 56 with an early medication change (EMC: immediate switch to venlafaxine and later lithium augmentation in case of further non-improvement) compared to patients treated according to current guideline recommendations (TAU: continued escitalopram treatment and later switch to venlafaxine in case of non-response). Results of the EMC trial have already been published previously [17–19]. We confirmed data from post hoc analyses of clinical trials, showing that early non-improvement identifies patients, who likely need alternate interventions. In the EMC group, most of the clinically relevant secondary outcomes like remission rate, time to remission, and time to response showed consistently advantageous results. However, the herein used two-step switch/augmentation strategy for this risk group was statistically not more effective than the control intervention [18].
Key inclusion criteria of the EMC trial were: (1) MDD, first episode or recurrent, according to DSM-IV; (2) a HAMD-17 score of ≥18 points at screening; (3) age 18–65 years and ≤60 years at the time of the first depressive episode. Patients were treated as outpatients by their general practitioner or specialist in a naturalistic setting before admission to inpatient care and before study inclusion in one of the psychiatric hospitals participating in the EMC trial. Key exclusion criteria regarding previous drug treatment in the index episode were an adequate trial of escitalopram, venlafaxine, or lithium for at least 4 weeks and in an adequate dose.
Study procedures
At screening visit directly before patients were enrolled into the trial (for study protocol see [16]), the diagnosis was verified using the “Mini-International Neuropsychiatric Interview” [20] according to DSM-IV [21]. Demographic parameters (age, sex, migrant background), psychiatric history (number of preceding depressive episodes, length of index episode, age at onset, clinical course), and prescription patterns (previous medication in index episode with detailed information regarding substance, start and end date, and dose) were assessed relying on patients’ self-reports. The severity of depressive symptomatology was assessed by the Hamilton Depression Rating Scale with 17 questions (HAMD-17) [22] and the Inventory of Depressive Symptoms (rated by clinicians (IDS-C) and patients (IDS-SR) [23]). The HAMD-17 and IDS were assessed by blinded and specially trained [24] raters.
For the present study, adherence of treatment with antidepressant drugs within the period of the index episode that preceded inclusion into the EMC trial was checked against current guidelines published in Germany, the US, and UK [5–7]. There are minor differences in the three guidelines (Table 1). The EMC trial was conducted exclusively in Germany and, therefore, we mainly focus on the guideline recommendations for German physicians, the German National Clinical Practice guideline [6], if recommendations were contradictory. The German guideline contains some of the most recent studies and meta-analyses. Five main aspects of guideline-recommended antidepressant treatment were assessed in detail: (1) whether an antidepressant was started depending on the severity level of the MDD, (2) whether the antidepressant was prescribed in the recommended therapeutic dose, (3) how long the patients were treated with the same antidepressant, (4) whether there were blood level measurements—as example for ‘treatment evaluation’—conducted, and (5) whether there was a treatment change, and if so, whether the treatment change strategy was guideline-adherent. Consequently, medication switch was only rated as guideline-adherent, if the dose of the new drug was within the therapeutic range and the new drug was part of the recommended ones in one of the guidelines. Dose adaption was only rated guideline-adherent, if there was a dose increase within the recommended prescription range. Start of a combination of antidepressants was rated guideline-adherent, if the dose of the new, second drug was within the therapeutic range and the combination pattern was either SSRI plus alpha 2 antagonist (α2A), or selective serotonin norepinephrine reuptake inhibitor (SSNRI) plus α2A, or tricyclic antidepressant (TCA) plus α2A. A combination or augmentation therapy of three or more antidepressant drugs was not considered guideline-adherent based on all three guidelines. The German National Clinical Practice guideline [6] recommends antidepressant drug augmentation with lithium or an antipsychotic (second or third generation) prior to medication switch as a treatment change strategy. However, as patients receiving lithium had been excluded from our study population due to the study design [16], we focused on dose adaptation, antidepressant medication switch, and combination as main parameters of our study.
Statistical analyses
Descriptive statistics were performed on the whole study population and on different subgroups. To analyze in detail the previous pharmacological treatment, we split the study population by a categorical variable “any previous psychopharmacological medication” in the two subgroups “any previous drug treatment” and “no previous drug treatment”. To address guideline adherence in our study population, we first took the subgroup with “no previous drug treatment” for comparison with current guideline recommendations. Secondarily, since many patients with antidepressant prescription had taken their medication for less than 8 weeks (56 days) before inclusion in the EMC trial, we created an additional subgroup using the categorical variables “continuous treatment of at least 56 days” and “any previous antidepressant medication”. Thirdly, to decipher the guideline adherence in terms of antidepressant dose, we added up all prescribed antidepressants cumulatively.
Data were collected, processed, and analyzed using the SPSS© software, version 23 (IBM©) and Excel 2013© software (Microsoft©). Descriptive statistics were presented with frequency and percentage distributions for categorical data and mean and standard deviations for continuous data. Chi-squared and sample t tests were conducted for between-group comparisons. At first, alpha was set at 5% (* p values <0.05 were considered significant) and statistically significant differences could be observed. To deal with spurious findings, in a second step alpha was set at 0.5% (** p values <0.005 were considered significant) using Bonferroni correction (10 tested parameters).
Results
Characterization of study population
In total, 889 patients were enrolled in the EMC trial and served as a study population (see also [18]). Demographic and clinical characteristics of the patients are presented in Table 2. In short, patients were 40.0 ± 11.8-years-old, were more often females (56.6%), suffered in 65.4% of the cases from a recurrent MDD, and were nearly all Caucasians (96.4%). The average index episode lasted for 215.7 ± 358.7 days with a minimum of 14 days and a maximum of 3276 days (median 119 days). As reflected by HAMD-17 and IDS-scores, all patients suffered from MDD with at least moderate severity (Table 2).
Previous drug treatment in the index episode
453 patients (51.0%) reported that they had been treated with any psychopharmacological drug during the index episode and before being enrolled in the EMC trial. Previous physicians had treated 414 of those patients (91.4%) with antidepressants, 39 patients (8.6%) had received other psychopharmacological drugs. 436 patients (49.0%) had not been treated with any psychopharmacological drug during the index episode.
A detailed look at the previous drug treatment in the index episode showed that most of the patients reported prescription of only one antidepressant drug during the index episode: 319 patients (70.4%) had received one antidepressant, 76 (16.8%) two, 16 (3.5%) three, 2 (0.4%) four, and 1 (0.2%) six antidepressants. The most commonly prescribed antidepressants were selective serotonin reuptake inhibitors (SSRI; 246 patients, 54.3%), followed by alpha 2 antagonists (α2A; 111 patients, 24.5%), tricyclic antidepressants (TCA; 80 patients, 17.7%), selective serotonin norepinephrine reuptake inhibitors (SSNRI; 57 patients, 12.6%), monoaminooxidase inhibitors (MOI; 7 patients, 1.5%), and other antidepressants such as opipramol, reboxetine, agomelatine, or bupropion (OAD; 73 patients, 16.1%). Benzodiazepines were prescribed in 17 patients (3.8%), antipsychotics in 17 patients (3.8%), and anticonvulsants in 5 patients (1.1%).
In a further analysis, we looked at clinical parameters that might distinguish the group of patients previously treated or not treated pharmacologically in the index episode. As shown in Table 2, patients with any previous drug treatment in the index episode were older, had a later onset of disease, were more severely ill as reflected by higher IDS-C-, HAMD-17-, and IDS-SR-scores, and more often showed a recurrent course of the MDD.
Guideline adherence regarding severity level of depression as indication for pharmacotherapy
Current guidelines recommend offering antidepressant drug treatment to patients suffering from an at least moderate degree of depression [5–7]. We, therefore, looked at the severity level of depression in all patients who were not treated pharmacologically during the index episode. All 436 of them suffered from a MDD of at least moderate severity (defined as HAMD-17: ≥17 as reported by [25]) at the time point of inclusion into the EMC trial. 241 of the untreated patients (55.3% of the untreated patients and 27.1% of all 889 patients) suffered from a moderate MDD (HAMD-17: 17–23 as reported by [25]) and 195 of the untreated patients (44.7% of the untreated patients and 21.9% of all 889 patients) suffered from a severe MDD (HAMD-17: ≥24 as reported by [25]). The untreated patients’ mean length of the index episode was 32.0 weeks (moderate MDD) and 24.8 weeks (severe MDD).
Guideline adherence of therapeutic drug monitoring
After 3–8 weeks of non-response, current guidelines recommend treatment evaluation steps (Table 1). Since the total number of treated patients also includes patients treated for less than 8 weeks with an antidepressant before inclusion in the EMC trial, we analyzed 153 patients in our sample who were continuously treated for at least 56 days. Antidepressant blood level concentrations were measured in 30.1% of the patients before inclusion in the EMC trial (Table 3).
Guideline adherence of length of antidepressant treatment
Current guidelines recommend an optimization of antidepressant treatment after 3–8 weeks of unsuccessful antidepressant treatment and unsuccessful treatment evaluation steps (Table 1). To check guideline adherence with regard to length of treatment in our sample of patients, we first analyzed in the total sample of patients who had been treated with one or more antidepressant drugs, how long patients were on average on the same drug. We found that 344 patients received the same antidepressant drug on average for 143.8 (±333.5) days. In a second step, we looked at the treatment length in the 153 patients in our sample who were continuously treated for at least 56 days. Here we found that 129 of the 153 patients (84.3%) had no medication change in their index episode. These patients were on average treated for 256.3 ± 346.2 days (36.6 ± 49.5 weeks) with the same antidepressant drug. The 24 (15.7%) patients who had reported of a medication change had to wait 497.8 ± 773 days (71.1 ± 110.4 weeks) until medication was adjusted. In addition, 74 (48.3%) patients with at least moderate MDD were not treated by an antidepressant and 68 (44.4%) patients with a severe depression. Very similar results were found for the 177 patients who were treated at least 42 days/6 weeks (results not shown).
Guideline adherence of dosage and change strategies of antidepressant treatment
We looked at the dosages of all 527 antidepressants, which were given to our 344 patients, for which sufficient information on exact dosages was available. We found that in 292 patients (84.9%) the dosage was always within the recommended dose, whereas in 52 patients (15.1%) the dose was lower and in 12 patients (3.5%) the dose was higher than recommended. In 153 patients in our sample who were continuously treated for at least 56 days, drug dosages were within the recommended range in 130 patients (85.0%), whereas in 15 patients (9.8%) the dose was too low and in 6 patients (3.9%) too high.
Tables 3 and 4 give an overview of the detailed strategies and treatment changes in the 153 patients, who were continuously treated for at least 56 days. To summarize, 129 patients (84.3%) did not receive any medication change despite treatment of at least 8 weeks. SSRIs were most often prescribed followed by α2As and TCAs. 13 patients who had no treatment change were treated by a combination therapy of two antidepressants from the very beginning of the index episode (see Table 4) which was rated as not guideline-adherent.
Dose increase is recommended as one of the first treatment change strategy in case of non-response [6]. The majority of the patients (n = 132, 86.3%) did not have any dose adaptation. Additionally, more patients had a dose decrease than a dose increase (Table 3). In the end, only 5 patients (3.3%) received guideline-adherent dose adaptation strategies. Medication was adjusted in only 24 patients (15.7%). Medication changes were switches within class (3 patients, 2.0%), switch between classes (13 patients, 8.5%), or combination treatment (8 patients, 5.2%). For more details of the exact treatment changes see Table 4. Medication change strategies were rated as guideline-adherent (see “Methods”) in 21 patients (87.5%) and not guideline-adherent in 3 patients (12.5%). The strategies not adherent to guidelines were switch between classes (n = 1; SSRI → TCA with incorrect dose) and combination (n = 2; SSRI → SSRI + OAD, TCA → TCA + TCA). The dose of the first antidepressant drug in the patients’ index episode was mostly within the recommended therapeutic ranges (85.0%) before medication was adjusted.
Discussion
In the present study, we show that a large proportion of outpatients with MDD are not treated according to current guideline recommendations. All patients who were not treated pharmacologically as outpatients suffered from a MDD of at least moderate severity, and approximately half of them from a severe depression—both typical indications for drug treatment. Psychotherapy alone is equally recommended for patients with a MDD of moderate severity, whereas drug treatment must be part of the treatment in case of severe depression [6]. Furthermore, 85% of patients being treated pharmacologically for at least 8 weeks did not experience any treatment change, although—after unsuccessful treatment evaluation steps—treatment change is recommended after 8 weeks in non-responders at the latest according to current guidelines. In contrast, treatment change strategies—if done—and dosages of antidepressants were in most cases guideline-adherent.
Current guidelines recommend antidepressant drug therapy as one option in cases of at least moderate severity, whereas drugs are not considered first-line treatment in cases of mild depression [5–7]. Assessments of MDD severity in our study took part directly before inclusion into the EMC trial and we, therefore, cannot exclude different severity levels in the weeks before inclusion. Nevertheless, we are confident that the indication of antidepressant drug therapy was given at least to some point during the index episode in most of the untreated patients: Approximately half of the untreated patients suffered from a moderate MDD with a mean length of the index episode of 32.0 weeks and approximately half of the untreated patients suffered from a severe MDD with a mean length of 24.7 weeks. It also appears unlikely that patients decided against a drug therapy although offered by the outpatient physician, since all patients agreed to participate in the EMC trial, which tested a new treatment algorithm of different antidepressant drugs. To further exclude the possibility that patients were too shortly ill before drug therapy could be started, we also calculated drug treatment rates in all patients being ill for at least 8 weeks. Here we found that approximately half of patients with at least moderate MDD were not treated by an antidepressant, and around four in ten patients with a severe depression.
It is unclear, why such a large group of patients did not receive antidepressant drug therapy although it was obviously indicated. Since depressed outpatients are mainly treated by general practitioners (GPs) [13], explanations for the low number of treated patients found in our study may be that GP treatment often suffers from poor MDD recognition and under-treatment [13]. GPs may have the problem to correctly diagnose MDD and to assess severity levels [11, 13, 26]. They often doubt the effectiveness of antidepressants [11, 26] and prescribe antidepressants more seldom than specialists [11]. Furthermore, many GPs have been shown to be unfamiliar with current guidelines [11]. In addition, patients often rate MDD as a result of adverse life events and, therefore, prefer counseling or psychotherapy and fear getting addicted to antidepressants [11, 26]. In accordance to these difficulties in outpatient drug treatment, Schneider and colleagues showed that after 6–8 weeks one half of the outpatients treated by their GP reported stagnation or even a progression of depressive symptoms [13].
After 3–8 weeks of non-response, guidelines recommend treatment evaluation steps before treatment change strategies [5–7]. Examples for these strategies are therapeutic drug monitoring, diagnostic reevaluation, and assurance of patient’s adherence. We analyzed antidepressant blood level measurements in 153 patients, who had been continuously treated for at least 8 weeks. Only around 30% of the patients reported that they had their antidepressant blood levels measured. Almost 40% of the performed blood level measurements were conducted in case of citalopram prescription. In contrast, only one patient treated with amitriptyline had a blood level measurement, although the German guideline clearly states that TCAs benefit from therapeutic drug monitoring and potential dose increase in case of non-response [6].
Current guidelines also recommend treatment change in case of insufficient response and already performed treatment evaluation steps (e.g., therapeutic drug monitoring). They give recommendations regarding treatment length until change which; however, differ from each other: The US guideline recommends 4–8 weeks [7], the UK guideline recommends 3–8 weeks [5], and the German guideline 4 weeks [6]. Since the patients in our study, who were treated pharmacologically, were depressed during their index episode for a mean of 225 days and were treated by antidepressants for 154.5 days (±340.9), we were able to assess in detail the length of treatment until a medication change was applied. We found that of the 153 patients who were treated for at least 8 weeks, 84.3% had no medication change, and the patients with medication change had to wait up to 490 days (71 weeks) until medication was finally adapted. This finding is comparable to a previous study by Milea et al. who reported that only 23.2% out of 134,287 depressed patients indicated treatment change, despite insufficient treatment effects [10].
Regarding the first choice of medication to treat MDD, a meta-analysis by Cipriani et al. [27] showed that the SSRI citalopram and sertraline have the best risk–benefit ratio and can, therefore, be recommended as first choice drugs in the treatment of MDD. The NICE guideline [5] adopted this and was the first to recommend SSRI as first-line drugs, whereas APA guideline [7] and German guideline [6] preferred to state that each antidepressant drug (except reserve antidepressants like MOI) could be considered equally. In our study, 48.0% of the patients had been treated with a SSRI as first choice, whereas 18.6% had been treated firstly by a α2A and 10.2% by a TCA. Since a treatment with escitalopram or venlafaxine in the index episode for at least 4 weeks and in an adequate dose was an exclusion criterion for participation in the EMC trial, all statements regarding previous use of specific antidepressants or classes of antidepressants in our study have to be made very cautiously. The recommendation of SSRIs as first-line drugs also ignores the fact that many patients and treating physicians prefer drugs, which have sedative effects and help them to find sleep. This explains why many patients preferred α2A over SSRIs.
Current guidelines recommend different non-responder strategies. These include treatment evaluation steps (e.g., adherence assurance or therapeutic drug monitoring) and treatment change—more precise augmentation, medication switch (replacement of the previous antidepressant by another one), dose increase or combination. Dose increase was only performed in five out of 153 analyzed patients. In addition, dose increase was performed five times with an SSRI, whereas the German guideline clearly states that dose increase is not recommended for SSRIs [6]. In contrast, only three out of the other 24 applied optimization strategies were not guideline-adherent. The German guideline [6] recommends to change the antidepressant substance class in cases of applying medication switch strategies. On the other hand, several publications and meta-analyses [28] were not able to show a statistically significant benefit either of switch between or within classes. This is in accordance with the NICE guideline [5]. It is important to keep in mind, that switching is, although it is the most commonly used treatment change strategy, not the first choice after non-response and that there is still a lack of research regarding treatment switch [6]. In addition, combination therapy is only recommended if one of the antidepressant drugs is an α2A. There is a lack of evidence for other combination schemes [6].
Regarding dosage recommendations, the US and the German guidelines refer to ranges taken from prescribing information [6, 7]. The UK guideline relies on information from the British National Formulary [5]. 84.9% of the patients, who had been prescribed an antidepressant drug, reported a dose recommended by these guidelines. In addition, in 153 patients who were continuously treated for at least 56 days, drug dosages were within the recommended range in 85.0% of the patients. In sum, the dosages were mostly guideline-adherent.
Strengths and limitations of our study
We are well aware that our study has limitations. First of all, this patient sample was not representative for depressed outpatients. We only investigated a subgroup of outpatients who were non-responder to outpatient treatment, were referred to inpatient treatment, fulfilled the inclusion criteria of the EMC trial (i.e., no successful previous treatments in the index episode with one of the study drugs like escitalopram, venlafaxine, or lithium), and were willing to participate in the EMC trial. Generalizability of results may also be limited since only patients were considered who were treated in one of the participating psychiatric institutions in the Rhine-Main metropolitan area. However, patients in our study were referred to inpatient treatment by a very large number of physicians and mainly not from the ambulatory services of the participating hospitals. Furthermore, the Rhine-Main metropolitan area has a rather high number of both GPs and psychiatric specialists, suggesting that the results might be even worse in regions with a lower number of doctors for the treatment of mental disorders. Despite those limitations, we believe that our study clearly documents that many outpatients are not treated according to guidelines—at least with respect to the use of antidepressants according to the severity level of MDD and treatment length before treatment is optimized—and that this lack of guideline adherence may contribute to unsuccessful outpatient treatment and need of inpatient care.
Secondly, relying mainly on patients’ self-reports regarding previous drug treatment might be critical. Patient reports of previous taken medication often yield an underreporting. It is, therefore, a limitation of our study that patient reports were not confirmed by assessment of reports of the treating physicians. We tried; however, to reduce possible confounding effects with very detailed and well-structured interviews and a large amount of collected parameters. In addition, patients only had to remember the present index episode, which reduced the amount of remembered drugs and treatment steps. Patient’s reports furthermore have the advantage over chart reviews that they assess true drug treatment and not only prescribed medications which very often are not taken by patients [29, 30]. In addition, it has to be taken into account that secondary analyses with multiple testing bear the risk of spurious findings. We, therefore, conducted Bonferroni correction on all statistically compared parameters and statistical significance could be confirmed as depicted in Table 1.
Thirdly, according to the EMC trial design (which was a pharmacotherapy trial), we only asked for previous drug treatment in the index episode, but not for previous psychotherapeutic treatment. It is, therefore, possible that at least some of the patients were treated psychotherapeutically during the index episode, which indicates guideline-adequate treatment for mild to severe forms of MDD. Therefore, the conclusions have to be more cautious and can be made only for previous drug treatment, but not for any treatment received.
Conclusion
We show in this sample of patients with MDD that, contrary to current guidelines, many outpatients are treated with the same antidepressant drug for very long periods of time until the treatment strategy is optimized. Outpatients’ physicians should introduce treatment evaluation and treatment changes at the latest after 8 weeks of non-response and should try dose increase, drug augmentation (e.g., with lithium), combination (e.g., with mirtazapine), or drug switches to another class as change strategies. An earlier treatment change may reduce patients’ treatment duration and suffering, may prevent hospital admissions, and may finally reduce costs. Positive effects of earlier treatment changes in naturalistic treatment settings have to be investigated in further studies.
References
Murray CJ, Vos T, Lozano R et al (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2197–2223
Sobocki P, Jonsson B, Angst J et al (2006) Cost of depression in Europe. J Mental Health Policy Econ 9:87–98
Wittchen HU, Jacobi F, Rehm J et al (2011) The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol 21:655–679
WHO (2015) Depression fact sheet No 369. World Health Organization. www.who.int/mediacentre/factsheets/fs369/en/. Accessed 16 March 2016
NICE (2016) Depression in adults: recognition and management—NICE guidelines [CG90]. National Institute for Health and Care Excellence. www.nice.org.uk/guidance/cg90. Accessed 14 March 2017
DGPPN (2016) S3-Leitlinie/Nationale VersorgungsLeitlinie Unipolare Depression—Langfassung; 2. Auflage, Version 4. Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde. http://www.awmf.org/uploads/tx_szleitlinien/nvl-005l_Unipolare_Depression_2016-11.pdf. Accessed 14 March 2017
APA (2010) Practice guidelines for the treatment of patients with major depressive disorder. American Psychiatric Association. www.psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf. Accessed 14 March 2017
Akincigil A, Bowblis JR, Levin C et al (2007) Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Med Care 45:363–369
Fernandez A, Haro JM, Codony M et al (2006) Treatment adequacy of anxiety and depressive disorders: primary versus specialised care in Spain. J Affect Disord 96:9–20
Milea D, Guelfucci F, Bent-Ennakhil N et al (2010) Antidepressant monotherapy: a claims database analysis of treatment changes and treatment duration. Clin Ther 32:2057–2072
Radisch J, Buchtemann D, Kastner D et al (2013) A literature- and expert-based analysis of the outpatient treatment of depressive ill people in Germany. Psychiatr Prax 40:252–258
Schneider F, Harter M, Brand S et al (2005) Adherence to guidelines for treatment of depression in in-patients. Br J Psychiatry J Mental Sci 187:462–469
Schneider F, Kratz S, Bermejo I et al (2004) Insufficient depression treatment in outpatient settings. German Med Sci GMS e-J 2:Doc01
Smolders M, Laurant M, Verhaak P et al (2009) Adherence to evidence-based guidelines for depression and anxiety disorders is associated with recording of the diagnosis. Gen Hosp Psychiatry 31:460–469
Wiegand HF, Sievers C, Schillinger M et al (2016) Major depression treatment in Germany-descriptive analysis of health insurance fund routine data and assessment of guideline-adherence. J Affect Disord 189:246–253
Tadic A, Gorbulev S, Dahmen N et al (2010) Rationale and design of the randomised clinical trial comparing early medication change (EMC) strategy with treatment as usual (TAU) in patients with major depressive disorder–the EMC trial. Trials 11:21
Nicod J, Wagner S, Vonberg F et al (2015) The amount of mitochondrial DNA in blood reflects the course of a depressive episode. Biol Psychiatr 80(6):e41–e42
Tadic A, Wachtlin D, Berger M et al (2016) Randomized controlled study of early medication change for non-improvers to antidepressant therapy in major depression—the EMC trial. Eur Neuropsychopharmacol 26(4):705–716
Tadic A, Wagner S, Gorbulev S et al (2011) Peripheral blood and neuropsychological markers for the onset of action of antidepressant drugs in patients with major depressive disorder. BMC Psychiatry 11:16
Sheehan DV, Lecrubier Y, Sheehan KH et al (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(Suppl 20):22–33 (quiz 34–57)
APA (2010) Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Rush AJ, Giles DE, Schlesser MA et al (1986) The Inventory for Depressive Symptomatology (IDS): preliminary findings. Psychiatry Res 18:65–87
Wagner S, Helmreich I, Lieb K et al (2011) Standardized rater training for the Hamilton Depression Rating Scale (HAMD(1)(7)) and the Inventory of Depressive Symptoms (IDS(C30)). Psychopathology 44:68–70
Zimmerman M, Martinez JH, Young D et al (2013) Severity classification on the Hamilton Depression Rating Scale. J Affect Disord 150:384–388
Kendrick T (2000) Why can’t GPs follow guidelines on depression? We must question the basis of the guidelines themselves. BMJ 320:200–201
Cipriani A, Furukawa TA, Salanti G et al (2009) Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet 373:746–758
Bschor T, Baethge C (2010) No evidence for switching the antidepressant: systematic review and meta-analysis of RCTs of a common therapeutic strategy. Acta Psychiatr Scand 121:174–179
Blaschke TF, Osterberg L, Vrijens B et al (2012) Adherence to medications: insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu Rev Pharmacol Toxicol 52:275–301
Osterberg L, Blaschke T (2005) Adherence to medication. New Engl J Med 353:487–497
Acknowledgements
The EMC trial (ClinicalTrials.gov Identifier: NCT00974155) was supported by Grant No. 01KG0906 from the German Federal Ministry for Education and Research (BMBF). The BMBF had no role in trial design, data collection, data analysis, data interpretation, or writing of the report. We are grateful to all patients who contributed to this study and to our clinical study members for their work. This includes especially Stefan Elsner, MD (Hospital for Psychiatry and Psychotherapy, Andernach), Julia Reiff, MD (Hospital for Psychiatry and Psychotherapy, Wiesbaden), Joachim Röschke, MD, PhD (Hospitals for Psychiatry and Psychotherapy, Bad Soden and Kiedrich), Ömür Baskaya, MD, Markus Lorscheider, MD, and Alexander Teml, MD (University Medical Center Mainz, Department of Psychiatry and Psychotherapy). We are also grateful to Armin Szegedi and Rolf Meinert (both formerly affiliated to University Medical Center Mainz), who participated in an early study phase of design development as well as to the members of the Data and Safety Monitoring Board (Walter Lehmacher, Institute for Medical Statistics, Informatics and Epidemiology, University of Cologne; Ulrich Hegerl, Department of Psychiatry and Psychotherapy, University of Leipzig; Ekkehard Haen, Department of Psychiatry and Psychotherapy, University of Regensburg).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
All participants gave their written informed consent to participate in the study after a complete and extensive description. All study components were approved by the local ethical committee of the Landesärztekammer Rheinland-Pfalz (study code no: 837.166.09 (6671)) and are compliant with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Conflict of interest
Dr. Tadic has received consultancy fees from Janssen and Novartis. Prof. Roll has received lecture fees by Boehringer Ingelheim, Lundbeck, and Otsuka. All other authors report no conflict of interest.
Rights and permissions
About this article
Cite this article
Herzog, D.P., Wagner, S., Ruckes, C. et al. Guideline adherence of antidepressant treatment in outpatients with major depressive disorder: a naturalistic study. Eur Arch Psychiatry Clin Neurosci 267, 711–721 (2017). https://doi.org/10.1007/s00406-017-0798-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-017-0798-6