Abstract
Relapses may represent a critical hazard in schizophrenia spectrum disorders as they are associated with an increased risk of a clinical and functional deterioration. Preventing relapse after recovering from a first psychotic episode has become a major challenge due to its critical impact on lifelong functionality. This study explored the rate of first and second relapses and the predictors associated with these relapses in a large cohort of non-affective psychosis patients during a period of 3 years after the first break of the illness. From February 2001 to May 2014, sociodemographic and clinical data from an epidemiological cohort of 341 non-affective first-episode psychosis patients at risk of relapse were analysed at a specialized early intervention service. Logistic regression, Cox regression, and Kaplan–Meier survival analyses were performed to compare non-relapsed and relapsed patients. One hundred and sixty-six (48.7%) individuals relapsed at least once. Median time to relapse was 17.0 months in non-adherent patients and 40.0 months in adherent patients (log-rankχ 2: 51.36; p < 0.001). Non-adherence to medication (odds ratio-OR 2.979; p < 0.001), schizophrenia diagnosis (OR 2.173; p = 0.002), and age of onset (OR 1.020; p = 0.033) were the main predictors of the first relapse. Fifty-six subjects experienced a second relapse (33.73%) predicted by diagnosis (OR 1.975; p = 0.074), age of onset (OR 1.078; p = 0.003), and positive symptoms (OR 0.863; p = 0.03), but not adherence. Non-adherence is the main predictive factor of first relapse after a first episode of psychosis. Second relapses were not often and not related to modifiable factors, suggesting that multiple relapsed patients may comprise a subgroup with a higher biological risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Relapses may represent a critical hazard in schizophrenia spectrum disorders as they are associated with an increased risk of a clinical and functional deterioration [1, 2]. The number of relapses has been associated with a greater risk of hospitalizations, chronicity and lack of clinical response [3, 4], brain tissue loss [5], suicide, or violence [6, 7], and it has suggested that they may lead to losses in clinical, social, and vocational recovery [8]. Even though this relationship has not been proven to be causal, it has been shown that relapses increase the economic cost, an enhanced burden for families and a higher stigma for patients [9, 10]. Despite early intensive interventions, as far as 82% of patients with a first episode of psychosis (FEP) may relapse during their first 5-years follow-up [11]. A recent systematic review revealed a rate of relapse of 77% in remitted first-episode patients during the first-year following antipsychotic discontinuation [12]. Likewise, in a previous report analysing a subsample of 140 individuals enrolled in PAFIP, we have described a relapse rate of the 65% at 3 years after the first break of the illness and the only significant predictor for relapse was non-adherence to antipsychotic medication [13].
Preventing relapses in the early phases of the illness has been suggested to be crucial to achieve a better outcome [14, 15]. Therefore, the identification and, in turns, the modification of factors determining clinical relapses are timely and relevant topics of investigation. Clinical variables and general demographic variables appear to have little impact on relapse rates, whereas non-adherence to medication, persistent substance use disorder, carers criticism, and poorer premorbid adjustment significantly increase the risk of relapse in FEP [16]. Interestingly, the highest risk factor was the lack of treatment adherence (a fourfold risk). With regard to multiple relapses, there is a lack of information in the prevalence of subsequent relapses after a first relapse in the follow-up of patients experiencing a first episode of psychosis. Earlier studies suggest a similar rate of first and second relapses [11], but a lower rate of subsequent relapses may be expected by the implementation of preventive approaches within an early intervention service in selected patients after their first relapse [16]. Confirming this main association is important in order to develop effective preventive approaches that make an effort in improving modifiable factors such as non-adherence that may contribute to reduce relapses and associated costs. Mayoral and colleagues (2016) described that the rate of symptom recurrence over the 3-year period in functionally recovered FEP patients following the self-elected discontinuation of antipsychotic treatment is extremely high (67.4%). Remarkably, relapsed individuals had a greater severity of symptoms and lower functionality after 3 years compared to those patients who did not relapse during the follow-up [15].
Our hypotheses were that adherence to medication is the main predictor factor of having a relapse after a FEP and that the specific intervention programs may reduce the incidence of second relapses. In the present study, with an extended sample of 393 first-episode patients followed up in the longitudinal intervention program of first-episode psychosis, Programa Asistencial de Fases Iniciales de Psicosis (PAFIP), at the Marques de Valdecilla University Hospital (Santander, Spain) and using the previous definition for relapse [13], we investigated the rate of first and second relapses and the predictors of an increasing risk of relapse during the 3-year period after a first episode of psychosis.
Methods
Study setting
The participants in this study were drawn from an ongoing longitudinal intervention program of first-episode psychosis, PAFIP, University Hospital Marques de Valdecilla, Spain [17]. In conformance with international standards for research ethics, the local institutional review board approved this program. PAFIP is an early intervention service aimed to early detect and treat patients with a first episode of psychosis in the autonomous region of Cantabria. Patients meeting inclusion criteria, and their families provided written informed consent to be included in the PAFIP. As a clinical program, PAFIP includes inpatient and outpatient care, and provides specific and personalized clinical attention, cognitive behavioural psychotherapeutic interventions and psychopharmacological treatment of patients, and also family interventions, during the first 3 years after program intake. A more detailed description of the PAFIP program has been previously presented elsewhere [18].
Study design
The present study was a prospective observational study. Patients from the PAFIP study who had a good response to antipsychotic treatment and achieved clinical stability according to inclusion criteria were followed up for 3 years.
During the follow-up period, trained psychiatrists assessed clinical status of the patients and data on antipsychotic treatment (doses, concomitant medications and dropouts); the appearance of relapses (according to previous definition) was regularly recorded.
Subjects
From February 2001 to May 2014, all referrals to PAFIP meeting the inclusion criteria: (1) 15–60 years; (2) living in the catchment area; (3) experiencing their first episode of psychosis; (4) no prior treatment with antipsychotic medication or if previously treated, a total lifetime of adequate antipsychotic treatment of less than 6 weeks; and (5) DSM-IV criteria for brief psychotic disorder, schizophreniform disorder, schizophrenia, or schizoaffective disorder, were eligible. Referrals were excluded because of any of the following reasons: (1) meeting DSM-IV criteria for drug dependence excluding nicotine and caffeine, (2) meeting DSM-IV criteria for mental retardation (premorbid intelligence quotient scores were estimated from the Wechsler Adult Intelligent Scale-III vocabulary subtest), (3) having a history of neurological disease or head injury. Patients meeting these criteria and their families provided written informed consent to be included in the PAFIP. The diagnoses were confirmed using the Structured Clinical Interview for DSM-IV (SCID–I) [19], carried out at 6 months after the baseline visit.
Only PAFIP patients who achieved clinical improvement (CGI rating ≤4 and a decrease of at least 30% on BPRS total score and all BPRS key symptom items, by being rated ≤3) for more than four consecutive weeks at some point during the first six months following program entry were included in the current investigation.
Clinical assessments
The severity scale of the Clinical Global Impression (CGI) Scale [20] was used to measure the overall severity of illness. Clinical symptoms were rated using the Brief Psychiatric Rating Scale (BPRS) [21], the Scale for the Assessment of Positive symptoms (SAPS) [22], the Scale for the Assessment of Negative symptoms (SANS) [23], the Calgary Depression Scale for Schizophrenia (CDSS) [24], and the Young Mania Rating Scale (YMRS) [25].
Complete clinical evaluations (all clinical and side effect scales were used) were conducted at baseline, 6 weeks, 12 and 36 months. In addition, clinical visits were carried out approximately every month during the follow-up, with regular CGI assessments. Patients were followed in our outpatient clinic with rapid and easy access to a clinical appointment at any time, for any possible signs/symptoms of clinical exacerbation that might appear. If this would be the case, a thorough clinical assessment was performed to evaluate the severity of clinical symptomatology or criteria of relapse.
Definitions of predictor variables
The analysed variables included sociodemographic, clinical, and premorbid variables. Sociodemographic variables were recorded from patients, family members, and medical records: gender, marital status (1. Single or never married/conjugal; 2. Other status); living arrangements at psychosis onset (1. Living with relatives; 2. Living alone and other status); occupational status during the 2 years prior to the initial interview (1. Employment/student; 2. Unemployed); socio-economic status assessed by the Hollingshead and Redlich Scale [27] (1—high ≤ 3; 2—low ≥ 4); educational level (1—primary education; 2—10 years of education or higher); urbanicity (growing up and living most of the life in a city with more than 10,000 inhabitants). Clinical variables included: duration of untreated illness (DUI) defined as the time in months from the first unspecific symptoms related to psychosis (for such a symptom to be considered, there should be no return to the previous stable level of functioning) to the initiation of adequate antipsychotic drug treatment. The duration of untreated psychosis (DUP) is defined as the time from the first continuous (present most of the time) psychotic symptom to the initiation of adequate antipsychotic drug treatment. Initial symptom severity was assessed by total score of BPRS, SAPS, and SANS, and the psychotic, disorganized, and negative dimensions. Insight was assessed by the three dimensions of the abbreviated Scale to Assess Unawareness of Mental Disorder (SUMD) [28], and the dimensions were dichotomized into scores greater than 1 (good insight) or 1 (poor insight). Premorbid variables included the evaluation of history of cannabis use at baseline and three years with a semi-structured interview (1- sporadic or frequent use of cannabis, defined as 1 or more times a week for at least the last year; 2- non-cannabis use) and history of drug use at baseline (1- sporadic or frequent use of cocaine or other illicit drugs, defined as 1 or more times a week for at least the last year; 2- non-drug use). The first-degree family history of psychosis was based on the subject and family reports. Current family support was assessed with a 3-point rating (insufficient, fair and sufficient), based on material and emotional support, and scores of fair and insufficient were classified as poor family support. Finally, the premorbid functioning in childhood (up to 11 years), early adolescence (12–15 years), late adolescence (16–18 years), and adulthood was measured by the Premorbid Adjustment Scale (PAS) [29] with the recommended modifications for first-episode psychosis patients [30]. A more detailed description of our predictor variables has been previously reported [13].
Adherence to antipsychotic drugs was assessed by gathering information about medication compliance from patients and close relatives putting together the information collected by different professionals involved in clinical follow-up (social workers, nurses, psychologists, and psychiatrists). For the present investigation, patients were dichotomized into having good (defined as patients regularly taking at least 90% of prescribed medication) and a poor adherence to medication during the observation period. This definition of adherence has been successfully used in previous reports from the PAFIP Cohort [13, 26]
Definition of relapse
Main outcome variables were relapse rates and time up to first relapse. According to our previous definition published elsewhere [13, 26], patients who achieved clinical improvement and stability (see above) were considered at risk of relapse over the 3-year period.
Relapse was defined as any of the following criteria that occurred during follow-up: (1) a rating of either 5 or above on any key BPRS symptom items, (2) CGI rating of ≥6 and a change score of CGI of “much worse” or “very much worse”, (3) hospitalization for psychotic psychopathology, or (4) completed suicide. The key BPRS symptoms were unusual thought content, hallucinations, suspiciousness, conceptual disorganization, and bizarre behaviour. Patients were considered to have a relapse if the re-emerged symptoms lasted for at least one week.
Data analysis
Data were analysed using SPSS (SPSS Inc., Chicago, IL, USA) version 17.0. The main objective of the analysis was to identify predictors of the first and second relapses after a first episode of non-affective psychosis.
A dichotomous variable was created which assigned a value of 1 once a patient experienced a relapse, 2 if the patient finished the follow-up without a relapse and 3 if the patient dropped out during follow-up (censored subjects). The included predictors were initially analysed with the univariate t-tests and Chi-square tests, depending on the nature of the variable, in order to compare characteristics of patients who relapsed with those who did not relapse after their first episode of psychosis.
Following univariate analyses, a backward logistic regression analysis was performed to predict relapse, including those predictor variables that were significantly associated with relapse (or a trend to significance with a p < 0.075) in the univariate analysis. Multiple Cox proportional hazards regression analysis was performed to confirm the robustness of the model and its association with time up to first relapse. Kaplan–Meier survival curves and a log-rank test were used to assess time to relapse and to compare median time to relapse between adherent and non-adherent patients. Patients who dropped out of the study or initiated an antipsychotic discontinuation strategy [15] were categorized as censored observations at the time of the occurring event.
Additionally, a second logistic regression model to predict second relapses in those patients who had a first relapse was performed with the same methodology.
Results
Description of study cohort
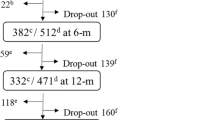
From 393 patients initially included in the PAFIP program, 341 achieved clinical improvement and stability accordingly to our previous definition. Clinical and sociodemographic characteristics of the sample, compared by relapse status at the end of the study are shown in Table 1. The overall dropout rate at three years was low (N = 48; 14.08%). Dropout reasons included the following: 21 patients due to own decision; 12 patients changed living catchment area; four died during follow-up and 11 dropouts were due to other reasons. Eight of these dropouts were after the first relapse (two patients died, four patients changed their living area and two more dropouts were due to other reasons). Figure 1 shows the trial profile.
From the 341 initial subjects, 243 (71.26%) were classified as adherent patients according to our definition, and 95 (27.86%) were non-adherent. In three subjects (0.88%), there was not enough information available to assess adherence.
Rates of relapse
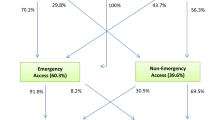
Of the 341 patients, 166 (48.68%) experienced a relapse at least once over the 3-year period. The relapse rates along the three years were: 21.60% in the first year (70 relapses from 324 subject at risk); 14.84% in the second year (46 subjects relapsed from 310 subjects at risk; cumulative risk of first relapse: 36.02%); and 16.89% in the third year (40 relapsed from 296 subjects at risk; cumulative risk of first relapse: 48.68%). It must be noticed that the maximum follow-up was 1200 days: 3 years and 4 months.
Of the first 166 relapsed patients, 56 patients suffered a second relapsed (33.73% of the 166 patients at risk). Of these, 15 experienced a third relapse (26.79% of the 56 patients at risk of third relapse). Only six of these 15 patients had a fourth relapse, and just one of these subjects experienced a fifth relapse over the period.
Predictors of first and subsequent relapses
Differences in predictor variables between subjects with and without relapses during follow-up are analysed in Table 1. The only significant factors associated with relapse were non-adherence to medication, schizophrenia diagnosis, a younger age, and age of onset, and there was a trend in the association with a longer DUP. Given the high correlation between age at admission and age of onset, only this last variable was included in further analysis in order to avoid collinearity between variables. Differences between patients with one relapse and more than one relapse during follow-up are analysed in Table 1. The significant factors associated with more than one relapse were a younger age of illness onset and at study entry, a lower initial severity of positive symptoms (total score of SAPS) and a trend in the association with schizophrenia diagnosis.
The logistic regression analysis for the first relapse included adherence, diagnosis and duration of untreated psychosis, and none of them were excluded in the backward analysis. DUP was transformed into years in order to better understand the relationship between DUP and relapse. The model was statistically significant (Nagelkerke’s R 2 = 0.147; χ 2 = 39.487; p < 0.001). Odds ratio (OR) values and confidence intervals for the predictor variables are shown in Table 2.
Similarly, the Cox regression analysis with relapse by observation time as the dependant variable did not exclude any of the predictors in the backward analysis and was a statistically significant model (χ 2 = 64.060; p < 0.001). Hazard ratios (HR) values and confidence intervals for the predictor variables are shown in Table 2. It is of note that the main predictor for both relapse in the logistic regression analysis and relapse by time to relapse in the cox regression analysis was adherence to medication (OR 2.979 for relapses; HR 2.812 for relapses by observation time; both p < 0.001). None of the variables included in the models were significantly correlated.
The median time to relapse was 28.0 months (95% CI 25.7–33.0) (Fig. 2). It is of note that median time to relapse in non-adherent patients (17.0 months, 95% CI 12.96–21.04) was significantly lower than in the adherent patients (40.0 months; No CI given due to a high number of extreme values: 52% of the adherent patients survived 40 months). The Kaplan–Meier survival analysis showed that these differences in the median time to relapse between non-adherent and adherent patients were statistically significant (log-rankχ 2 = 51.356; p < 0.001) (Fig. 3). This result was not significantly different when the sample was stratified by schizophrenia (log-rankχ 2 = 45.002; p < 0.001) and other diagnoses (log-rankχ 2 = 6.659; p = 0.010; comparison in the total sample, pooled results over the strata: log-rankχ 2 = 48.355; p < 0.001).
The logistic regression analysis for second relapses included diagnosis, age of onset, and SAPS total initial score. The model was statistically significant (Nagelkerke’s R 2 = 0.151; log-rankχ 2 = 18.956; p < 0.001). Values and confidence intervals for the predictor variables are shown in Table 3. The forced addition of the variable “adherence” in a second block did not improve this model (p = 0.925), and it was not included as a significant independent predictor for second relapses (OR 0.967; p = 0.924).
Discussion
The most relevant results that arose from our study were: (1) The rate of first relapse after a first episode of psychosis was 48.68% and out of them only 34% experienced a second relapse during the three-year follow-up (2) non-adherence to medication was the main relevant predictor of clinical relapses after a first episode of psychosis; and (3) only non-modifiable factors such as diagnosis and age of onset increased the risk of having a second relapse.
Almost half of the sample relapsed in the first 3 years after the break of the illness. Our current relapse rates are slightly lower than in our previous report of 65% over the period 2001–2005 [13] and other reported relapse rates after a first episode of psychosis [31]. Although a lower relapse rate could be expected in the context of an early intervention (EI) programme, similar rates have been reported in the context of EI, such as a 29.7% relapse rate at two years in the PEPP Canadian programme [32] or 30% relapse rate at 18 months in the LEO Lambeth programme [33]. Differences between reports might be explained by differences in definitions of relapse, lengths of follow-up, and diagnosis and characteristics of the setting (for instance, distribution of associated implied predictors). Thus, a recent meta-analysis revealed lower rates of relapses in EI services versus standard care settings and established mean relapse rates of 20 and 34% at 1- and 2-year follow-up for EI services [16]. With regard to second relapses, we found a much lower relapse rate compared to the first relapse. Our cumulative rate of second relapses (33.9%) is also in contrast with much higher rates such as the 56% reported by Robinson et al. [11]. The main independent predictor of first relapse and time to relapse in our sample was non-adherence to medication. Non-adherence to medication conferred an odds ratio of relapse near to 3 over the period. This result was concordant with our previous results and with other studies [31, 34, 35] including recent revisions and meta-analyses [16, 36] that showed non-adherence as the most important predictor for relapse in psychosis. Accordingly, when patients were included in a treatment discontinuation strategy, twice as many relapses occurred compared to those patients who maintained antipsychotic treatment [15, 37].
The only additional predictors associated with relapse in our study were schizophrenia diagnosis and age of onset. With regard to diagnosis, only a few previous studies analysed this variable, some of them comparing affective versus non-affective diagnosis [16]. Our results here are in agreement with those studies that found that patient with schizophrenia and a younger age of onset tends to have more and earlier relapses [38]. In this regard, these patients may comprise a subgroup of individuals with a higher biological risk to relapse.
A key strength of this study has been to analyse second and subsequence relapses and their associated predictors. As expected in an early intervention programme, second and following relapses cumulative incidence were relatively low. As a difference with factors increasing the risk of having a first relapse, only non-modifiable factors such as diagnosis, age of onset, and initial positive symptom severity were significantly associated with these second relapses. Thus, first-episode subjects who achieve clinical improvement and stability with low adherence to antipsychotic treatment are in a higher risk of relapse, and therefore, preventive and intensive interventions are highly recommended to avoid this modifiable risk factor. In contrast, non-modifiable predictors (i.e. diagnosis or age of onset) seem to be significantly influencing the risk of having subsequent relapses. Additionally, as an unexpected finding, we observed that a lower initial severity of positive symptoms was associated with a higher risk of having a second relapse. We do not have an explanation for this finding, but it might be speculated that a lower initial psychotic severity could be associated with a more insidious course that might lead a higher risk of relapse.
Our results emphasize the potential relevance of two kinds of factors that may increase the risk of relapse: (1) intrinsic established risk factors such as diagnosis or age of illness onset and (2) modifiable factors such as adherence to medication. Subjects with a first relapse and low adherence to antipsychotic treatment appear as a group of high risk of relapse in which a clinical effort in preventive and intensive interventions is highly recommended to avoid changeable risk factors and therefore to diminish the rate of second relapses.
Some limitations must be taken into account in the interpretation of the current investigation. First, in our study, assessors were not blinded to the patient’s adherence status. The assessment of adherence and relapse by independent raters may have reduced this potential caveat. However, it has a high epidemiological and clinical validity in terms of representativeness, including usual clinical practice. A second limitation is the lack of an objective assessment for the adherence to treatment. We are fully aware that plasma levels and urine assays of the antipsychotic medication or its metabolite can provide the strongest evidence of medication usage, but they are expensive and invasive for the patient. Additionally, biological assays are not capable to tell us the real dosage of medication patients regularly take, given individual differences in the metabolism of medication. In our study, we followed a previous definition used for research, where adherence to medication was assessed gathering information from psychiatrists, nurses, and social workers involved in the treatment and follow-up of the patient and by taking into consideration information from patients and close relatives. Third, the lack of a control group is an additional limitation. Finally, although a large number of predictors have been included in the analysis, it is possible that other predictors could have been included with different results.
In conclusion, the recurrence of psychotic symptoms after having achieved clinical improvement and stability is a frequent event during early phases of the illness, being non-adherence to medication the best predictor of relapse after a first episode of psychosis. Clinicians should be fully aware of this risk and provide accurate information to patients about the risk of relapse if antipsychotics are discontinued. Therefore, systematic interventions to ensure proper understanding should be established in first-episode programs to enhance treatment compliance and to prevent uncontrolled treatment disengagement. The rate of subsequence relapses in an early intervention service is, as expected, less common than the rate of first relapse and do not seem to be related to adherence or other modifiable factors, suggesting that patients with multiple relapses may comprise a subgroup with a higher biological risk.
References
Kane JM (2007) Treatment strategies to prevent relapse and encourage remission. J Clin Psychiatry 68(Suppl 1):27–30
Wyatt RJ (1997) Research in schizophrenia and the discontinuation of antipsychotic medications. Schizophr Bull 23:3–9
Wiersma D, Nienhuis FJ, Slooff CJ, Giel R (1998) Natural course of schizophrenic disorders: a 15-year followup of a Dutch incidence cohort. Schizophr Bull 24:75–85
Lieberman J, Jody D, Geisler S et al (1993) Time course and biologic correlates of treatment response in first-episode schizophrenia. Arch Gen Psychiatry 50:369–376
Andreasen NC, Liu D, Ziebell S et al (2013) Relapse duration, treatment intensity, and brain tissue loss in schizophrenia: a prospective longitudinal MRI study. Am J Psychiatry 170:609–615. doi:10.1176/appi.ajp.2013.12050674
Amore M, Menchetti M, Tonti C et al (2008) Predictors of violent behavior among acute psychiatric patients: clinical study. Psychiatry Clin Neurosci 62:247–255. doi:10.1111/j.1440-1819.2008.01790.x
Hor K, Taylor M (2010) Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol 24:81–90. doi:10.1177/1359786810385490
Masand PS, Roca M, Turner MS, Kane JM (2009) Partial adherence to antipsychotic medication impacts the course of illness in patients with schizophrenia: a review. Prim Care Companion J Clin Psychiatry 11:147–154. doi:10.4088/PCC.08r00612
Kane JM (2007) Treatment adherence and long-term outcomes. CNS Spectr 12:21–26
Hong J, Windmeijer F, Novick D et al (2009) The cost of relapse in patients with schizophrenia in the European SOHO (Schizophrenia Outpatient Health Outcomes) study. Prog Neuropsychopharmacol Biol Psychiatry 33:835–841. doi:10.1016/j.pnpbp.2009.03.034
Robinson D, Woerner MG, Alvir JMJ et al (1999) Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry 56:241. doi:10.1001/archpsyc.56.3.241
Zipursky RB, Menezes NM, Streiner DL (2014) Risk of symptom recurrence with medication discontinuation in first-episode psychosis: a systematic review. Schizophr Res 152:408–414. doi:10.1016/j.schres.2013.08.001
Caseiro O, Pérez-Iglesias R, Mata I et al (2012) Predicting relapse after a first episode of non-affective psychosis: a three-year follow-up study. J Psychiatr Res 46:1099–1105. doi:10.1016/j.jpsychires.2012.05.001
Birchwood M, Todd P, Jackson C (1998) Early intervention in psychosis. The critical period hypothesis. Br J Psychiatry Suppl 172:53–59
Mayoral-van Son J, de la Foz VO-G, Martinez-Garcia O et al (2015) Clinical outcome after antipsychotic treatment discontinuation in functionally recovered first-episode nonaffective psychosis individuals. J Clin Psychiatry. doi:10.4088/JCP.14m09540
Alvarez-Jimenez M, Priede A, Hetrick SE et al (2012) Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res 139:116–128. doi:10.1016/j.schres.2012.05.007
Pelayo-Terán JM, Pérez-Iglesias R, Ramírez-Bonilla M et al (2008) Epidemiological factors associated with treated incidence of first-episode non-affective psychosis in Cantabria: insights from the Clinical Programme on Early Phases of Psychosis. Early Interv Psychiatry 2:178–187. doi:10.1111/j.1751-7893.2008.00074.x
Crespo-Facorro B, Pérez-Iglesias R, Ramirez-Bonilla M et al (2006) A practical clinical trial comparing haloperidol, risperidone, and olanzapine for the acute treatment of first-episode nonaffective psychosis. J Clin Psychiatry 67:1511–1521. doi:10.4088/JCP.v67n1004
First MB, Spitzer RL, Gibbon M, Williams JBW (2001) Structured Clinical Interview for DSM-IV Axis I disorders (clinician version). New York State Psychiatric Institute Biometrics Department, New York
Guy W (1976) CGI. Clinical global impression. In: Guy W (ed) ECDEU assess. Man. Psychopharmacol. Revis, pp 217–222
Overall JE, Gorham DR (1962) The brief psychiatric rating scale. Psychol Rep 10:799–812. doi:10.2466/pr0.1962.10.3.799
Andreasen NC (1984) Scale for the Assessment of Positive Symptoms (SAPS). University of Iowa, Iowa City
Andreasen NC (1983) Scale for the Assessment of Negative Symptoms (SANS). University of Iowa, Iowa
Addington D, Addington J, Maticka-Tyndale E (1993) Assessing depression in schizophrenia: The Calgary depression scale. Br J Psychiatry 22:39–44
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133:429–435
Crespo-Facorro B, Pérez-Iglesias R, Mata I et al (2011) Relapse prevention and remission attainment in first-episode non-affective psychosis. A randomized, controlled 1-year follow-up comparison of haloperidol, risperidone and olanzapine. J Psychiatr Res 45:763–769. doi:10.1016/j.jpsychires.2010.11.002
Hollingshead A, Redlich F (1958) Social class and mental illness: a community study. Wiley, New York
Amador XF, Flaum M, Andreasen NC et al (1994) Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry 51:826–836
Cannon-Spoor HE, Potkin SG, Wyatt RJ (1982) Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull 8:470–484
van Mastrigt S, Addington J (2002) Assessment of premorbid function in first-episode schizophrenia: modifications to the Premorbid Adjustment Scale. J Psychiatry Neurosci 27:92–101
Robinson DG, Woerner MG, Alvir JM et al (1999) Predictors of treatment response from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry 156:544–549
Malla A, Norman R, Bechard-Evans L et al (2008) Factors influencing relapse during a 2-year follow-up of first-episode psychosis in a specialized early intervention service. Psychol Med 38:1585–1593. doi:10.1017/S0033291707002656
Craig TKJ, Garety P, Power P et al (2004) The Lambeth Early Onset (LEO) team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ 329:1067. doi:10.1136/bmj.38246.594873.7C
Coldham EL, Addington J, Addington D (2002) Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand 106:286–290
Addington DE, Patten SB, McKenzie E, Addington J (2013) Relationship between relapse and hospitalization in first-episode psychosis. Psychiatr Serv 64:796–799. doi:10.1176/appi.ps.201200440
Emsley R, Chiliza B, Asmal L, Harvey BH (2013) The nature of relapse in schizophrenia. BMC Psychiatry 13:50. doi:10.1186/1471-244X-13-50
Wunderink L, Nienhuis FJ, Sytema S et al (2007) Guided discontinuation versus maintenance treatment in remitted first-episode psychosis: relapse rates and functional outcome. J Clin Psychiatry 68:654–656. doi:10.4088/JCP.v68n0502
Hui CL-M, Tang JY-M, Leung C-M et al (2013) A 3-year retrospective cohort study of predictors of relapse in first-episode psychosis in Hong Kong. Aust NZ J Psychiatry 47:746–753. doi:10.1177/0004867413487229
Acknowledgements
The present study was carried out at the Hospital Marqués de Valdecilla, University of Cantabria, Santander, Spain, under the following grant support: Instituto de Salud Carlos III PI020499, PI050427, PI060507, Plan Nacional de DROGAS Research Grant 2005- Orden sco/3246/2004, SENY Fundació Research Grant CI 2005-0308007, Fundación Marqués de Valdecilla API07/011 and CIBERSAM. Unrestricted educational and research grants from AstraZeneca, Pfizer, Bristol-Myers Squibb, and Johnson & Johnson provided support to PAFIP activities. No pharmaceutical industry has participated in the study concept and design, data collection, analysis and interpretation of the results, and drafting the manuscript. PAFIP II is registered as a clinical trial (NCT02305823) in Clinicaltrials.gov: “Comparative Study of Aripiprazole, Quetiapine and Ziprasidone in the Treatment of First-Episode Non-affective Psychosis” (AZQ2005). The study, designed and directed by B C-F and JL V-B, conformed to international standards for research ethics and was approved by the local institutional review board. We wish to thank the PAFIP researchers who helped with data collection. In addition, we acknowledge the participants and their families for enrolling in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. José María Pelayo-Terán has received lecture honoraria and travel support form Janssen Johnson & Johnson, Lundbeck, Otsuka Pharmaceuticals, GlaxoSmithkline and EiLilly. Prof. Benedicto Crespo-Facorro has received honoraria for consulting/advisory boards from Otsuka Pharmaceuticals and lecture honoraria from Janssen Johnson & Johnson, Lundbeck, Roche and Otsuka Pharmaceuticals. Prof. Rafael Tabarés-Seisdedos has received grants from or acted as a consultant for the following companies: AstraZeneca, Janssen, Eli- Lilly, Lundbeck, Novartis, Pfizer, Sanofi-Aventis, and Wyeth that were deposited into research accounts at the University of Valencia. Dr.Virginia Gajardo Gajardo Galán, Víctor de la Ortiz-García de la Foz, Obdulia Martín-García and Dr. Rosa Ayesa-Arriola report no additional financial support or other relationship relevant to the subject of this article.
Additional information
José María Pelayo-Terán and Virginia Gajardo Gajardo Galán have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Pelayo-Terán, J.M., Gajardo Galán, V.G., de la Ortiz-García de la Foz, V. et al. Rates and predictors of relapse in first-episode non-affective psychosis: a 3-year longitudinal study in a specialized intervention program (PAFIP). Eur Arch Psychiatry Clin Neurosci 267, 315–323 (2017). https://doi.org/10.1007/s00406-016-0740-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-016-0740-3