Abstract
Purpose
The internal auditory canal (IAC) plays a key role in lateral skull base surgery. Although several approaches to the IAC have been proposed, endoscope-assisted transcanal corridors to the IAC have rarely been studied. We sought to provide a step-by-step description of the transcanal transpromontorial approach to the IAC and analyze anatomic relationships that might enhance predictability and safety of this approach.
Methods
Ten cadaveric specimens were dissected and the extended transcanal transpromontorial approach to the IAC was established. Various morphometric measurements and anatomic landmarks were reviewed and analyzed.
Results
The proposed technique proved feasible and safe in all specimens. There was no inadvertent injury to the jugular bulb or internal carotid artery. The chorda tympani, a key landmark for the mastoid segment of the facial nerve, was identified in all dissections. The spherical recess of the vestibule and middle turn of cochlea are important landmarks for identification of the labyrinthine segment of the facial nerve. Identification of all boundaries of the working area is also essential for safe access. Among various morphometric measurements, the modiolus-IAC angle (≈ 150°) proved particularly consistent; given its ease of use and low variability, we believe it could serve as a landmark for identification and subsequent dissection of the IAC.
Conclusions
The extended transcanal transpromontorial approach to the IAC is feasible and safe. Relying on anatomic landmarks to ensure preservation of the involved neurovascular structures is essential for a successful approach. The modiolus-IAC angle is a consistent, reproducible landmark for IAC identification and dissection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The internal auditory canal (IAC) is central to the practice of neurotology. Several conditions that affect the cerebellopontine angle (CPA) originate from or are in direct relation to the IAC. Accordingly, various surgical approaches to the IAC have been studied and are well documented in the literature. Among these, presigmoid (translabyrinthine, retrolabyrinthine, transcochlear), retrosigmoid, and middle fossa approaches are particularly notable [1,2,3]. In the context of surgical treatment of vestibular schwannomas, the literature has addressed the advantages and disadvantages of each approach. Factors such as tumor size, location, and hearing status are the main points taken into consideration when choosing the approach [4,5,6,7,8].
With advances in the quality of video-assisted surgery systems and related instrumentation, the use of endoscopic approaches in otologic surgery has garnered much interest in recent years [9]. Several studies have reported the use of endoscope-assisted transcanal approaches in conditions of the outer, middle, and inner ear [10,11,12].
Regarding approaches to the IAC in particular, in 2013 Marchioni et al. published an anatomic study demonstrating the possibility of reaching the IAC via the endoscope-assisted transcanal route [13]. This study suggested that diseases of the IAC and CPA could be treated through this technique, which the authors named the endoscopic transcanal transpromontorial approach [14]. Since then, further studies have addressed the relationship of anatomic structures involved in this approach, as well as its practical applications.
In a 2016 study of cadaveric temporal bone specimens, Komune et al. analyzed several anatomic relationships implicated in the endoscopic transcanal approach to the IAC. Among several findings, they proposed a triangular area formed by the cochleariform process and anterior and posterior edges of the round window niche as a landmark for access. This area would form the lateral (superficial) projection of the fundus of the IAC [15]. Marchioni et al. also mention the importance of the spherical recess of the vestibule as an anatomic landmark for the labyrinthine segment of the facial nerve [14].
Regarding clinical application of the endoscopic transcanal transpromontorial approach to the IAC, in 2018 Marchioni et al. published a study reporting their results with 49 patients who underwent vestibular schwannoma resection via this route. The study included patients with small intracanalicular tumors or those protruding only slightly into the CPA (Koos grades 1 and 2). Among their main findings, postoperative preservation of the facial nerve (House–Brackmann grade I or II) was achieved in a remarkable 95.9% of patients [16].
Although the studies carried out to date have addressed anatomical aspects of this approach and reported practical use cases for its application, little has been done to systematize the technique. Therefore, the present study aims to provide a systematic, step-by-step description of the transcanal transpromontorial approach to the internal auditory canal and analyze potential anatomic relationships that may add predictability and/or safety to this approach.
Materials and methods
Study specimens
This study was carried out through dissection of 10 previously preserved specimens (cadaver heads). All had been prepared by intravascular injection of dyed silicone.
Anatomic dissection of the specimens was based on the extended transcanal transpromontorial approach (detailed below), as proposed by Pressuti et al. [17].
All stages of the dissections were carried out with the aid of an endoscope (Karl Storz HOPKINS®, 0°, 18 × 4 mm); photographic documentation was obtained using the IMAGE 1 hub HD camera capture system (Karl Storz).
The transcanal transpromontorial approach to the internal auditory canal
All anatomic dissections were performed by the same operator (an experienced endoscopic otologic surgeon), in the following sequence of steps (Fig. 1):
-
Lempert type III endaural incision (intercartilaginous, between tragus and helix) for better exposure of EAC;
-
Total removal of all EAC skin and the tympanic membrane;
-
Drilling and widening of EAC (canalplasty). At this point, the chorda tympani was identified along the posterior surface of the medial portion of the bony EAC.
-
Epitympanectomy (atticotomy) and identification of tegmen tympani;
-
Removal of malleus and incus;
-
Drilling out of tympanic annulus for complete exposure of retrotympanum and hypotympanic structures, particularly the jugular bulb (JB) and internal carotid artery (ICA);
-
Identification and skeletonization of tympanic and mastoid segments of the facial nerve;
-
Removal of cochleariform process and tensor tympani muscle;
-
Partial exposure of middle cranial fossa dura adjacent to tegmen tympani and greater superficial petrosal nerve;
-
Identification of “working area”, delimited by the following structures: tympanic segment of the facial nerve, mastoid segment of the facial nerve, greater superficial petrosal nerve, middle cranial fossa dura, internal carotid artery, and jugular bulb;
-
Removal of stapes and widening of oval window niche, identifying the spherical and elliptical recesses of the vestibule;
-
Cochleotomy with identification of basal and middle/apical turns, as well as the modiolus; and
-
Identification and skeletonization of IAC and dura of adjacent posterior cranial fossa.
A Endaural intercartilaginous incision (between tragus and helix) and exposure of bony EAC (right ear); B Canalplasty and identification of chorda tympani (left ear); C Dissection of the hypotympanum and identification of jugular bulb and internal carotid artery (left ear); D Epitympanectomy (left ear); E Dissection of “working area” and its limits (tympanic and mastoid segments of facial nerve, dura mater of middle cranial fossa, internal carotid artery, jugular bulb) (left ear); F Cochleotomy, opening of vestibule, and identification of spherical and elliptical recesses (left ear); G Identification of modiolus and lower surface of the IAC (left ear); H 180-degree skeletonization of IAC and exposure of dura of the adjacent posterior fossa (left ear). CT: chorda tympani; JB: jugular bulb; ICA: internal carotid artery; FN-mast: mastoid segment of the facial nerve; FN-tymp: tympanic segment of the facial nerve; RW: round window; M: malleus; I: incus; St: stapes; TT: tegmen tympani; MFD: middle fossa dura; LSC: lateral semicircular canal; Pr: promontory; GG: geniculate ganglion; SPN: greater superficial petrosal nerve; BTC: basal turn of cochlea; MTC: middle turn of cochlea; ATC: apical turn of cochlea; SphR: spherical recess of vestibule; ElipR: elliptical recess of vestibule; Mod: modiolus; IAC: internal auditory canal; PFD: posterior fossa dura
Morphometric measurements
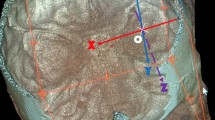
Based on the photographic documentation of the dissections, the following morphometric measurements were analyzed (Fig. 2):
-
Round window-facial nerve distance: defined as the shortest distance between the central point of the round window membrane and the anterior edge of the mastoid segment of the facial nerve;
-
Geniculate ganglion-jugular bulb distance: defined as the distance between the geniculate ganglion and a line parallel to the apex of the jugular bulb;
-
Carotid-facial nerve distance: defined as the shortest distance between the posterior vertical segment of the internal carotid artery and the mastoid segment of the facial nerve;
-
“Working area”: defined as the area delimited by the mastoid and tympanic segments of the facial nerve, greater superficial petrosal nerve, middle cranial fossa dura, internal carotid artery, and jugular bulb; and
-
Modiolus-IAC angle: defined as the angle between the lines that represent the central axis of the modiolus and the IAC.
A “Working area” (shaded yellow) and its boundaries (left ear) B Dissection of the modiolus and IAC and identification of the modiolus-IAC angle (right ear). JB: jugular bulb; ICA: internal carotid artery; FN-mast: mastoid segment of the facial nerve; FN-tymp: tympanic segment of the facial nerve; RW: round window; MFD: middle fossa dura; LSC: lateral semicircular canal; GG: geniculate ganglion; SPN: greater superficial petrosal nerve; Mod: modiolus; IAC: internal auditory canal; FCD: facial-carotid distance; FRWD: facial-round window distance; GBD: geniculate ganglion-jugular bulb distance; M-IAC: modiolus-IAC angle
All measurements were performed in the ImageJ software environment.
Statistical analysis
Means, standard deviations, and coefficients of variance were used to analyze the degree of variability (or dispersion) of the results obtained. Pearson’s coefficient was used to analyze possible correlations between the variables of interest.
Results
A total of 10 specimens were dissected (4 left ears and 6 right ears). No specimen had malformations or fractures that might have influenced the dissection and subsequent analysis of its outcome.
Following the steps described above, it was possible to access the internal auditory canal and lateral base of the skull in a feasible and safe manner. The chorda tympani was identified in all cases and served as a key landmark to protect the mastoid segment of the facial nerve during canalplasty and dissection of the hypotympanum and retrotympanum. Also in all cases, the jugular bulb and internal carotid artery were identified during dissection of the hypotympanum, and there was no inadvertent injury to these structures. The labyrinthine segment of the facial nerve was consistently located between the spherical recess of the vestibule and the middle turn of the cochlea.
Analysis of the aforementioned morphometric measurements identified high variability for most, except for the modiolus-IAC angle, which had a low coefficient of variation (1.35%); on analysis of correlation study, the most relevant findings were the positive associations between the carotid-facial distance and working area (Pearson coefficient = 0.8) and between the GG-jugular bulb distance and working area (Pearson coefficient = 0.6).
The tables below summarize the results of morphometric measurement (Table 1 and Fig. 3).
Discussion
The objectives of this study, as set out above, were to provide a detailed, step-by-step description of the extended transcanal transpromontorial approach to the IAC, analyze the anatomic relationships involved, and assess its predictability, feasibility, and safety.
Regarding safety, the most relevant aspect is preservation of the neurovascular structures involved in the approach, with particular emphasis on the internal carotid artery, jugular bulb, and facial nerve.
The ICA and JB are normally located within the hypotympanum (and, occasionally, in the mesotympanum as well). We believe the safest method for preservation of the aforementioned structures in this approach is the appropriate identification of both at the very start of the middle ear dissection. By keeping these structures clearly visible, inadvertent injury is very unlikely to occur during subsequent steps. It is worth noting that these structures, especially the JB, exhibit significant anatomic variation within the temporal bone [18, 19]. In the present study, there was no inadvertent injury to these structures.
As is well known, the facial nerve has a close relationship with the temporal bone and, due to its sinuous course, is usually divided for purely didactic purposes into four segments: meatal, labyrinthine, tympanic, and mastoid. Any transtemporal approach to the IAC relies on specific strategies and landmarks with the aim of identifying and preserving the different segments of the facial nerve. In the specific case of the extended transcanal transpromontorial approach to the IAC, some important points are worth noting. The tympanic segment is easily visualized during the approach; the main landmarks at this stage are the cochleariform process, oval window, and lateral semicircular canal [20, 21]. The mastoid segment, however, requires a specific strategy for dissection and safe identification. First, during canalplasty, we believe it is important to identify the entire course of the chorda tympani along the posterior bony wall of the EAC. We can thus infer the position of the mastoid segment of the facial nerve and then proceed safely with dissection of the retrotympanum and hypotympanum (Fig. 1B and C). Another potential landmark for the mastoid segment of the facial nerve is the distance between the round window (easily visualized during this approach) and the nerve. Our analysis showed that the average distance between these structures was 6.67 mm, with a standard deviation of 1.33 mm but a coefficient of variation of 19.92%—denoting high variability and, therefore, low applicability in practice. This variability, which has been demonstrated in previous studies, is mainly due to the position and angle of the cochlea within the temporal bone [22,23,24,25]. The labyrinthine segment, in turn, is closely related to the structures of the inner ear. The main landmarks for this segment are the spherical recess of the vestibule and the middle turn of the cochlea [26]. In the present study, in all cases the labyrinthine segment was identified between the spherical recess and the middle turn of the cochlea, corroborating the findings of Marchioni et al. (Fig. 4A).
Facial nerve anatomy. A Labyrinthine segment of the facial nerve, identified between the spherical recess of the vestibule (in yellow) and the middle turn of the cochlea (in green); B Intratemporal anatomy of the facial nerve as seen through the extended transcanal transpromontorial approach. *labyrinthine segment of the facial nerve; **meatal segment of the facial nerve. JB: jugular bulb; ICA: internal carotid artery; FN-mast: mastoid segment of the facial nerve; FN-tymp: tympanic segment of the facial nerve; VN: vestibular nerve; CN: cochlear nerve; MFD: middle fossa dura; CPA: cerebellopontine angle
Any surgical corridor to the IAC and lateral base of the skull must provide the widest and best exposure possible in order to enable removal of the target lesion (e.g., tumor) while preserving the neurovascular structures. The transcanal transpromontorial approach to the IAC has certain bottlenecks that should be discussed.
The first of these is the EAC itself, which can be easily managed by enlargement (canalplasty), a step described in the extended version of the transcanal transpromontorial approach which allows greater flexibility of subsequent actions and even use of the microscope to perform some steps of the technique [17]. In our opinion, canalplasty should be mandatory when pursuing this approach, to facilitate instrumentation and handling (including three- or four-handed manipulation) as well as better control of the cerebrospinal fluid fistula which often results from the usually necessary opening of the IAC dura.
The second bottleneck is in the middle ear; here there is no possibility of expansion, as preservation of the involved structures is mandatory. In the present study, we called this region the “working area” and it was delimited by the mastoid segment of the facial nerve posteriorly, the tympanic segment of the facial nerve and greater superficial petrosal nerve (and/or middle cranial fossa dura) superiorly, the ICA anteriorly, and the JB inferiorly (Fig. 1E). In our sample, the mean area of this region was 116.26 mm2 (standard deviation = 22.15 mm; coefficient of variation = 19.04%). Previous studies that also analyzed this specific landmark also reported great variability, probably due to anatomic variation of the structures that delimit it and to the measurement methods employed [27, 28]. When compared with other surgical corridors to the IAC, the transcanal transpromontorial approach appears relatively narrower [29,30,31]. Nevertheless, with careful, proper dissection of its limits and favorable anatomy, we believe it is possible to work on the IAC safely through this approach. Some considerations are in order. As mentioned above, the size of the “working area” is clearly influenced by anatomic variation in its delimiting structures, especially the jugular bulb and internal carotid artery. Our study found a positive correlation between the size of the working area and the GG-JB and carotid-facial distances (Pearson coefficients of 0.8 and 06 respectively). Therefore, in some cases, the position (and dehiscence) of the jugular bulb and the internal carotid artery may hinder or even contraindicate the transcanal transpromontorial approach to the IAC. Accordingly, we consider prior CT imaging essential to detect this anatomy in advance.
The third, and final, potential bottleneck is the most medial region of the approach, at the level of the porus acusticus. Although intuitively there appears to be a significant natural narrowing at this point in relation to the middle ear, this does not seem to actually occur, as suggested by Yacoub et al. in recent work. In their specific study, the lateral exposure (similar to the “working area” concept of our study) was 152 mm2 and the medial exposure area adjacent to the internal acoustic opening was 151.9 mm2 [32]. Although we did not measure this area, Fig. 1H does show the extent of exposure of this region that can be obtained. Also worth mentioning is that the transcanal transpromontorial approach to the IAC provides better exposure of the inferior surface of the IAC, unlike the presigmoid transmastoid and retrosigmoid approaches, which better expose the posterior surface of the IAC. Regarding exposure of the area of dura adjacent to the internal acoustic opening, Fig. 1H shows that this approach clearly provides better exposure of the portion anterior to the IAC. Bulky tumors that significantly distort the posterior wall of the IAC may therefore cause greater difficulty or even prevent safe removal through the transcanal transpromontorial approach.
Regarding predictability, the availability of reliable and relatively stable landmarks is a cornerstone of any surgical approach. The small sample size of this study notwithstanding, during dissections we observed that the modiolus of the cochlea may represent an important anatomic landmark for subsequent identification and skeletonization of the IAC. The angle formed between a line parallel to the major axis of the modiolus and the IAC was approximately 150°, with little variation (mean = 149.46°, standard deviation = 2.05°, coefficient of variation = 1.37%). Therefore, we suggest that, once the modiolus has been identified, a line be drawn at 150 degrees from its axis to identify the inferior surface of the IAC. The IAC can then be dissected and skeletonized down to the porus acusticus (Fig. 1F, G and H).
Although it would fall outside the scope of this work to discuss the clinical applications of this surgical approach and compare it to other more traditional corridors, we will briefly discuss our anatomic findings, the existing literature, and the authors’ perceptions. Our first point is that the extended transcanal transpromontorial approach to the IAC can be performed with the aid of an endoscope and operating microscope and, in many situations, both, taking joint advantage of the features of each instrument to perform any given step of the procedure. Second, due to the relatively narrower surgical space this corridor provides, it is essential to consider the risk–benefit ratio of this strategy as an approach to IAC and lateral skull base lesions.
In general, the transcanal transpromontorial approach appears quite appropriate for lesions confined to the inner ear (e.g., intralabyrinthine schwannomas), given its simplicity, the possibility of direct visualization of the involved structures, the fact that it obviates the need to make any significant changes to the anatomy of the middle ear and EAC, and its sparing of the IAC dura (and avoidance of resulting CSF leak).
In conditions that affect the IAC and CPA, our opinion is that the transcanal transpromontorial route can be considered for small tumors that exclusively occupy the IAC (especially its most lateral part—the fundus), as it allows predictable, safe access for removal of pathology while preserving adjacent neurovascular structures. This, however, often requires blind sac closure of the EAC, which in turn mandates modification of the anatomy of the outer ear, in addition to potentially leading to formation of a cholesterol granuloma due to entrapment of cells in the middle ear mucosa (a still-understudied phenomenon). Furthermore, as already mentioned, anatomic variation—especially of the JB and ICA—can hinder this approach or render it unsafe.
Although it can provide exposure of a substantial area of the lateral skull base for management of larger tumors, particularly those occupying the CPA, we believe this approach has more disadvantages than advantages when compared to translabyrinthine or transotic approaches, mainly due to the presence of the aforementioned bottlenecks, which increase the difficulty of removing the target lesion while preserving adjacent neurovascular structures (especially the facial nerve). Again, this is simply a reflection of the authors’ current opinion, and other studies in future may provide more precise comparisons of these different approaches.
For illustrative purposes, Fig. 5 below gives an example of clinical application of the endoscope-assisted extended transcanal transpromontorial approach for resection of an intralabyrinthine schwannoma extending slightly into the IAC (Fig. 5).
Intralabyrinthine schwannoma with extension to the IAC. Resection via endoscope-assisted extended transcanal transpromontorial approach (left ear). A Magnetic resonance imaging showing tumor in the left ear (> : intrameatal tumor; > > : intracochlear tumor); B Endaural incision (Lempert) and EAC exposure; C Canalplasty; D Identification of the chorda tympani; E Dissection of the hypotympanum with identification and skeletonization of the jugular bulb and internal carotid artery; F Epitympanectomy/atticotomy; G Exposure and delimitation of the “working area”; H Cochleotomy and identification of the intracochlear tumor component; I Complete resection of the intracochlear tumor; J-K Identification and skeletonization of the IAC; L Opening of the IAC dura with identification of the intrameatal tumor component and neurovascular contents of the IAC; M Resection of the intrameatal tumor component; N IAC after complete tumor resection, showing preserved intrameatal facial nerve; O Plugging of the IAC dural defect with abdominal fat; P Blind sac closure of the IAC. *labyrinthine segment of the facial nerve; CT: chorda tympani; JB: jugular bulb, ICA: internal carotid artery; CN: cochlear nerve; FN: facial nerve; FN-mast: mastoid segment of the facial nerve; FN-tymp: tympanic segment of the facial nerve; RW: round window; M: malleus; I: incus; MFD: middle fossa dura; Pr: promontory; GG: geniculate ganglion; OW: oval window; SphR: spherical recess of the vestibule; BTC: basal turn of cochlea; MTC: middle turn of cochlea; ATC: apical turn of cochlea; Tu-Cochlea: intracochlear tumor; Tu-IAC: intrameatal tumor; IAC: internal auditory canal; AF: abdominal fat
Conclusions
This article provided a step-by-step description of the extended transcanal transpromontorial approach to the IAC through anatomic dissection of cadaveric specimens. Our main conclusions were:
-
When following the proposed sequence of steps, the extended transcanal transpromontorial approach to the IAC proved feasible, predictable, and safe.
-
The key landmark for the mastoid segment of the facial nerve was the previously identified chorda tympani adjacent to the posterior wall of the medial third of the EAC. The tympanic segment is easily visualized, and no landmark is required for identification. The labyrinthine segment is systematically found between the spherical recess of the vestibule and the middle turn of the cochlea.
-
It is essential that all structures which delimit the “working area” be clearly identified for optimal exposure and to reduce the risk of inadvertent injury, especially the jugular bulb and internal carotid artery.
-
Based on our overall findings and the low variability of this measurement, we propose the modiolus-IAC angle (≈ 150°) as a key landmark for identification and subsequent skeletonization of the IAC.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Bennett M, Haynes DS (2007) Surgical approaches and complications in the removal of vestibular schwannomas. Otolaryngol Clin North Am 40:589–609. https://doi.org/10.1016/j.otc.2007.03.007
Bento RF, De Brito RV, Sanchez TG, Miniti A (2002) The transmastoid retrolabyrinthine approach in vestibular schwannoma surgery. Otolaryngol Head Neck Surg 127:437–441. https://doi.org/10.1067/mhn.2002.129824
Bento RF, de Brito RV, Sanchez TG (2002) A rapid and safe middle fossa approach to the geniculate ganglion and labyrinthine segment of the facial nerve. Ear Nose Throat J 81:320–326
Samii M, Matthies C (1997) Management of 1000 vestibular schwannomas (acoustic neuromas): hearing function in 1000 tumor resections. Neurosurgery 40:248–260. https://doi.org/10.1097/00006123-199702000-00005. (discussion: 260–2)
Lanman TH, Brackmann DE, Hitselberger WE, Subin B (1999) Report of 190 consecutive cases of large acoustic tumors (vestibular schwannoma) removed via the trans-labyrinthine approach. J Neurosurg 90:617–623. https://doi.org/10.3171/jns.1999.90.4.0617
García-Ibanez E, García-Ibanez JL (1980) Middle fossa vestibular neurectomy: a report of 383 cases. Arch Otolaryngol Head Neck Surg 88:486–490
Staecker H, Nadol JB Jr, Ojeman R, Ronner S, McKenna MJ (2000) Hearing preservation in acoustic neuroma surgery: middle fossa versus retrosigmoid approach. Am J Otol 21:399–404
Brackmann DE, House JR III, Hitselberger WE (1994) Technical modifications to the middle fossa craniotomy approach in removal of acoustic neuromas. Am J Otol 15:614–619
Marchioni D, Alicandri-Ciufelli M, Piccinini A, Genovese E, Presutti L (2010) Inferior retrotympanum revisited: an endoscopic anatomic study. Laryngoscope 120:1880–1886. https://doi.org/10.1002/lary.20995
Marchioni D, Alicandri-Ciufelli M, Molteni G, Artioli FL, Genovese E, Presutti L (2010) Selective epitympanic dysventilation syndrome. Laryngoscope 120:1028–1033. https://doi.org/10.1002/lary.20841
Marchioni D, Villari D, Alicandri-Ciufelli M, Piccinini A, Presutti L (2011) Endoscopic open technique in patients with middle ear cholesteatoma. Eur Arch Otorhinolaryngol 268:1557–1563. https://doi.org/10.1007/s00405-011-1533-y
Presutti L, Marchioni D, Mattioli F, Villari D, Alicandri-Ciufelli M (2008) Endoscopic management of acquired cholesteatoma: our experience. J Otolaryngol Head Neck Surg 37:481–487
Marchioni D, Alicandri-Ciufelli M, Mattioli F, Nogueira JF, Tarabichi M, Villari D, Presutti L (2013) From external to internal auditory canal: surgical anatomy by an exclusive endoscopic approach. Eur Arch Otorhinolaryngol 270:1267–1275. https://doi.org/10.1007/s00405-012-2137-x
Marchioni D, Alicandri-Ciufelli M, Rubini A, Masotto B, Pavesi G, Presutti L (2017) Exclusive endoscopic transcanal transpromontorial approach: a new perspective for internal auditory canal vestibular schwannoma treatment. J Neurosurg 126:98–105. https://doi.org/10.3171/2015.11.JNS15952
Komune N, Matsuo S, Miki K, Rhoton AL Jr (2017) The endoscopic anatomy of the middle ear approach to the fundus of the internal acoustic canal. J Neurosurg 126:1974–1983. https://doi.org/10.3171/2016.5.JNS16261
Marchioni D, Soloperto D, Masotto B, Fabbris C, De Rossi S, Villari D, Presutti L (2018) Transcanal transpromontorial acoustic neuroma surgery: results and facial nerve outcomes. Otol Neurotol 39:242–249. https://doi.org/10.1097/MAO.0000000000001658
Presutti L, Alicandri-Ciufelli M, Bonali M, Rubini A, Pavesi G, Feletti A, Masotto B, Anschuetz L, Marchioni D (2017) Expanded transcanal transpromontorial approach to the internal auditory canal: pilot clinical experience. Laryngoscope 127:2608–2614. https://doi.org/10.1002/lary.26559
Cömert E, Kiliç C, Cömert A (2018) Jugular bulb anatomy for lateral skull base approaches. J Craniofac Surg 29:1969–1972. https://doi.org/10.1097/SCS.0000000000004637
Jiang Y, Chen Y, Yao J, Tian Y, Su L, Li Y (2015) Anatomic assessment of petrous internal carotid artery, facial nerve, and cochlea through the anterior transpetrosal approach. J Craniofac Surg 26:2180–2183. https://doi.org/10.1097/SCS.0000000000000207
Wetmore SJ (1991) Surgical landmarks for the facial nerve. Otolaryngol Clin North Am 24:505–530
Pulec JL (1993) The facial nerve: how to find it. Ear Nose Throat J 72:677–685
Arístegui M, Martín-Oviedo C, Aristegui I, García-Leal R, Ruiz-Juretschke F (2019) Anatomical variations of the intrapetrous portion of the facial nerve. Anat Rec (Hoboken) 302:588–598. https://doi.org/10.1002/ar.23923
Jain S, Gaurkar S, Deshmukh PT, Khatri M, Kalambe S, Lakhotia P, Chandravanshi D, Disawal A (2019) Applied anatomy of round window and adjacent structures of tympanum related to cochlear implantation. Braz J Otorhinolaryngol 85:435–446. https://doi.org/10.1016/j.bjorl.2018.03.009
Singla A, Gupta T, Sahni D, Gupta AK, Aggarwal A (2017) Topography of neurovascular structures in relation to round window and how it relates to cochlear implantation. Surg Radiol Anat 39:1309–1316. https://doi.org/10.1007/s00276-017-1884-1
Wysocki J, Skarzyñski H (1998) Distances between the cochlea and adjacent structures related to cochlear implant surgery. Surg Radiol Anat 20:267–271. https://doi.org/10.1007/BF01628488
Presutti L, Nogueira JF, Alicandri-Ciufelli M, Marchioni D (2013) Beyond the middle ear: endoscopic surgical anatomy and approaches to inner ear and lateral skull base. Otolaryngol Clin North Am 46:189–200. https://doi.org/10.1016/j.otc.2012.12.001
Alicandri-Ciufelli M, Federici G, Anschuetz L, Pavesi G, Todeschini A, Presutti L, Marchioni D (2017) Transcanal surgery for vestibular schwannomas: a pictorial review of radiological findings, surgical anatomy and comparison to the traditional translabyrinthine approach. Eur Arch Otorhinolaryngol 274:3295–3302. https://doi.org/10.1007/s00405-017-4630-8
Anschuetz L, Presutti L, Schneider D, Yacoub A, Wimmer W, Beck J, Weber S, Caversaccio M (2018) Quantitative analysis of surgical freedom and area of exposure in minimal-invasive transcanal approaches to the lateral skull base. Otol Neurotol 39:785–790. https://doi.org/10.1097/MAO.0000000000001827
Zador Z, de Carpentier J (2015) Comparative analysis of transpetrosal approaches to the internal acoustic meatus using three-dimensional radio-anatomical models. J Neurol Surg B Skull Base 76:310–315. https://doi.org/10.1055/s-0035-1549000
Hsu FP, Anderson GJ, Dogan A, Finizio J, Noguchi A, Liu KC, McMenomey SO, Delashaw JB Jr (2004) Extended middle fossa approach: quantitative analysis of petroclival exposure and surgical freedom as a function of successive temporal bone removal by using frameless stereotaxy. J Neurosurg 100:695–659. https://doi.org/10.3171/jns.2004.100.4.0695
Tang CT, Kurozumi K, Pillai P, Filipce V, Chiocca EA, Ammirati M (2013) Quantitative analysis of surgical exposure and maneuverability associated with the endoscope and the microscope in the retrosigmoid and various posterior petrosectomy approaches to the petroclival region using computer tomograpy-based frameless stereotaxy. A cadaveric study. Clin Neurol Neurosurg 115:1058–1062. https://doi.org/10.1016/j.clineuro.2012.10.023
Yacoub A, Wimmer W, Molinari G, Alicandri-Ciufelli M, Presutti L, Caversaccio M, Anschuetz L (2020) Transcanal transpromontorial approach to lateral skull base: maximal area of exposure and surgical extensions. World Neurosurg 135:e181–e186. https://doi.org/10.1016/j.wneu.2019.11.102
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by João Paulo Valente, Ricardo Ferreira Bento and Rubens Brito. The first draft of the manuscript was written by João Paulo Valente and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the local ethics committee of.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Valente, J.P., Bento, R.F. & Brito, R. The endoscopic transcanal approach to the internal auditory canal: an anatomic study. Eur Arch Otorhinolaryngol 281, 5179–5187 (2024). https://doi.org/10.1007/s00405-024-08739-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-024-08739-1