Abstract
Introduction
Benign paroxysmal positional vertigo (BPPV) is one of the commonest causes of peripheral vertigo. It is treated with various canalolith repositioning manoeuvres by changing the head positions to allow the otoconial debris to fall back from the affected canal back to the utricle. The present study has compared the rate of recovery of vertigo with modified Epley’s manoeuvres as compared to Semont’s manoeuvre in patients with posterior canal BPPV.
Materials and methods
One hundred and seventy patients diagnosed by positive Dix–Hallpike test as posterior canal BPPV were included in this clinical trial. Subjective analysis of vertigo was done using visual analogue scale. 85 patients each were recruited in two arms by simple randomization using lottery method. Modified Epley’s manoeuvre was administered to one group and Semont’s manoeuvre to the other. They were recalled after 2 weeks for clinical assessment with repeat Dix–Hallpike and VAS.
Results
Repeat Dix–Hallpike manoeuvres after two weeks revealed that 95.3 and 90.6% patients improved in Modified Epley’s and Semont’s group, respectively. After the second manoeuvre, the resolution rate was significantly higher in Semont’s manoeuvre 100% (8 out of 8 patients), as compared to 25% (1 out of 4 patients) in Modified Epley’s manoeuvre. Comparison of the mean values of VAS day 0 and VAS 2 weeks has been found to be statistically significant (p value of < 0.001).
Conclusion
Both Epley’s and Semont’s manoeuvre are equally efficacious in treatment of BPPV. However, use of Semont’s manoeuvre required fewer repeat manoeuvres for complete resolution of symptoms in patients. The Semont’s manoeuvre is also comparatively easier to perform with less number of position changes, takes less time, and has no requirement of post-manoeuvre mobility restrictions. Hence, it is recommended that Semont’s manoeuvre can be routinely used for the management of PC BPPV especially in older population and patients with spinal problems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dix and Hallpike coined the term ‘Benign Paroxysmal Positional Vertigo’ (BPPV) in the year 1952. It is said to be one of the commonest causes for peripheral vestibular disorders. BPPV is marked by rotatory dizziness provoked with sudden head movements. Patients usually complain of dizziness that occurs when tossing and turning in the bed, looking up, lying down or bending over. BPPV has a lifetime prevalence of 2.4% [1].
BPPV is divided into three types on the basis of canal involvement—posterior, lateral, and superior semicircular canal BPPV. Out of which posterior canal BPPV is the commonest accounting for 80% of cases, lateral canal BPPV accounts for 20%, while anterior canal BPPV is the rarest as it is due to gravity and self-limiting [2, 3]. BPPV usually has a favourable outcome which is due to the fact that it recovers spontaneously in as many as 20% of cases by the end of 1 month and up to 50% by the end of 3 months. However, in the undiagnosed and untreated patients, the impact on the quality of life can be more than ‘benign’ as these patients may have an increased risk of falls and injuries [3].
The most common cause of BPPV is idiopathic (34–86%); other important causes are head trauma (14.5–18%) and otologic disease including infection, inflammation or dysfunction of microcirculation of inner ear (3–9%) [4, 5].
Two theories are usually quoted to explain the pathophysiology: cupulolithiasis and canalithiasis. In the theory of ‘cupulolithiasis’ the degenerated otoconia in the utricle adhere to semicircular canal’s cupula, which makes it denser than the endolymph surrounding it, therefore it becomes increasingly vulnerable to the consequences of gravity [6]. The canalithiasis theory states that the degenerated otoconia do not cohere to the cupula, but float in the endolymph of the posterior canal [7]. In both these theories, head movements make the otoconia move, which causes inappropriate stimulation of the cupula causing excitation in the ampullary nerve, leading to vertigo.
The different modalities to treat BPPV include vestibular exercises, repositioning manoeuvres, vestibular sedatives, and surgeries. Epley’s, Semont’s, Gans manoeuvre and Brandt–Daroff exercises are used to treat of PCBPPV. Most of these cases can be treated with ease in the outpatient department [8, 9].
Various modifications of Epley’s and Semont’s manoeuvres are also available in the form of restrictions of head and body movements for few days post repositioning manoeuvres or advising vestibular exercises, etc. [10,11,12].
Materials and methodology
A Randomized Clinical Trial, CTRI Reg No. CTRI/2021/04/032839 and Ref No. REF/2021/02/041186 was carried out at the ENT department of a tertiary care centre in India for period of 18 months. Study protocol was performed according to ethical guidelines of the 2002 Declaration of Helsinki, and carried out after approval by the Institutional Review Board and Ethics Committee. The inclusion criteria were all cases of posterior canal BPPV of age 18–50 years confirmed by positive Dix–Hallpike test. The exclusion criteria included patients on any vestibular sedatives, CNS depressants or any history of cervical or spinal pathology. A total of 170 individuals were enrolled in the study. Counselling of patients about the trial was done and written informed consent was taken for their participation in the study. They were diagnosed as PCBPPV by history, clinical features and positive Dix–Hallpike test.
Sample size
With α (significance level) = 5% and power of study = 80%, proportion 1 = 95% and proportion 2 = 73% [1], the minimum needed sample was 81 in each arm. Accordingly, 85 patients were included in the study in each group.
Recruitment of cases
All confirmed cases of PC BPPV reporting to the ENT OPD were taken in the study as per inclusion criteria. Institutional ethics committee clearance was obtained before the start of the trial.
Evaluation of cases
Patients who had presented with vertigo were assessed and diagnosed as a case of PCBPPV using the Dix–Hallpike test and subjective analysis of severity of vertigo was done using visual analogue scale (VAS) of 0–10, where 0 signifies no vertigo and 10 denotes severe vertigo.
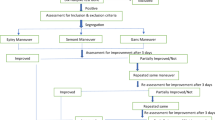
After diagnosis patients were randomized into two arms by simple randomization using the lottery method with 85 each in the treatment by Epley’s (Fig. 1) and Semont’s manoeuvres (Fig. 2) groups. As part of the various modification to the Epley’s manoeuvre, in our study after treatment with Epley’s manoeuvre, patients were advised postural restrictions and to avoid sleeping on the affected side for 48 h. No such restrictions were advised in patients treated with Semont’s manoeuvre. Patients were called after 02 weeks for evaluation by Dix–Hallpike test and VAS. Patients who did not consent and patients who were lost to follow-up were excluded from the study.
Epley’s manoeuvre. Left PCBPPV. a The patient is made to sit on the table with head turned 45° to affected side (left). b Patient is taken down rapidly with head turned 45° to left and extended to the edge of table. c The head is then turned 90° to other side (right). d It follows rotation the both head and body 90° facing downwards (135° from the supine position). e The legs are then displaced over the side of the table, in anticipation to return back to the sitting position, and f the patient is brought back to the sitting position with the head bent forwards
Semont’s manoeuvre. Left posterior canal BPPV. a Patient’s head is turned 45° to the uninvolved side (right). b He is quickly brought to the affected side (left), with his face turned upwards by 45°. c He is then swung swiftly to the opposite side (right) with face turned downwards by angle of 45°. d He is then repositioned back slowly to sitting position
Statistical analysis was done using paired ‘t’ test and Chi-square test. ‘p’ value less than 0.05 was taken as significant. Data were compiled and analysed using IBM SPSS statistics 20 software. Results so obtained were represented graphically.
Results
Participants comprised 82 males and 88 females. The ratio of males to females was 0.93:1. The mean age of study participants was 47.14 ± 14.71 years. Most of the patients were in the age group 31–50 years. Minimum and maximum ages were 20 and 89 years, respectively. 81 patients (95.2%) in Epley’s group and 77 (90.5%) patients in Semont’s group recovered after the first particle repositioning manoeuvre itself. Age-wise distribution of patients in each group is tabulated (Fig. 3). Out of total 170 patients, 7% patients were still symptomatic after the first manoeuvre (04 patients in Epley’s group and 08 patients in the Semont’s group). Repeat manoeuvres were given to the patients who were symptomatic after the first repeat manoeuvres. In the Semont’s group, all eight patients (100% recovery) had recovered after one repeat manoeuvre, whereas in the Epley’s group, out of four patients, one recovered after one repeat manoeuvre (25% recovery), two recovered after the second repeat manoeuvres and remaining one patient had to be given three repeat manoeuvres (Fig. 4). This difference was statistically significant which suggests that lesser number of repeat manoeuvres are required for complete resolution of symptoms in Semont’s group. Moreover, it was noted that all the symptomatic patients were given repeat manoeuvre between days 02–08 (Fig. 5). There was no significant difference was seen in the days of presentation with persistent vertigo between the two groups.
The mean value of VAS was compared at the time of presentation and after 2 weeks. In the Epley’s group, the comparison of the mean values of VAS at day 0 and day 14 revealed a higher mean value on day 0 with a difference of 9.03529 which was statistically significant with a p value of < 0.001 (Fig. 6).
The Semont's group had similar results. On comparison of the mean values of VAS on day 0 and day 14, the mean values of VAS on day 0 were higher with a difference of 8.65882 which is statistically significant with a p value of < 0.001 (Fig. 6). The results confirmed that both the manoeuvres are equally efficacious for treating PC BPPV even though there were no post procedural mobility restrictions in Semont’s group as compared to Epley’s group where these restrictions were advised.
Discussion
BPPV is stated to be the commonest cause in the patients with peripheral vertigo. It many involve any semicircular canal—posterior, lateral or superior. Out of three, posterior semicircular canal alone is involved in almost 80% of the cases, while superior semicircular canal is least commonly involved and otoconia whenever present, gets repositioned due to the effects of gravity [4]. BPPV is characterized by rotatory giddiness on quick changes in the head and body positions. Pathophysiology can be explained by two theories, cupulolithiasis and canalithiasis as discussed earlier. Patients of posterior canal BPPV commonly present with the typical history of vertigo, which usually lasts for few seconds typically 10–20 s, aggravated by sudden head changes, i.e. while rolling on bed, laying down or while getting up from bed, tying shoe laces, etc. It may or may not accompanied by nausea or vomiting [2].
There is no spontaneous nystagmus in patients of BPPV, rather it is induced with Dix–Hallpike test to diagnosis BPPV. In patients of posterior canal BPPV, this test results in upbeating and tortional nystagmus after a latent period of a few seconds. Various treatment options available to treat posterior semicircular canal BPPV are—Epley’s manoeuvre, Semont’s manoeuvre, Brandt–Daroff exercises, Gans manoeuvre and surgery in the form of singular neurectomy in refractory cases. Various modifications of Epley’s and Semont’s manoeuvres are also available in the form of restrictions of head and body movements for few days post repositioning manoeuvres and advising vestibular exercises, etc. [4]. Various studies have been carried out to compare the efficacy of different methods which are discussed below [4, 12, 13].
A study on 60 patients of posterior canal BPPV was undertaken in 2016 by Sen et al. In their study, Group 1 (30 patients) underwent Epley’s manoeuvre and Group 2 (30 patients) underwent the Semont’s manoeuvre. In all, 26/30 patients in Group 1 (87%) and 17/30 patients in Group 2 (57%) demonstrated improvement. When the two groups' post-manoeuvre improvements were compared, Group 1 exhibited a bigger improvement (54%) than Group 2 (46%) [13]. In another study done by Ajayan et al. in 2017, comprised 200 patients. Amongst these out of the 100 cases treated with Epley’s manoeuvre, 95 cases showed complete resolution at the end of 3 months. In 100 cases managed by Semont’s manoeuvre, 94 showed complete resolution of symptoms after 3 months. They concluded that both Epley’s and Semont’s manoeuvre are equally effective in treating the patients of PCBPPV [14]. In the study by Ashok Kumar Gupta et al. in 2019, 90 patients with unilateral PCBPPV were recruited on the basis of positive Dix–Hallpike test. 3 groups were formed—Epley’s, Semont’s, and Brandt–Daroff, 30 patients selected in each group randomly. Results showed that 90%, 73.33% and 50% patients improved in Epley's, Semont’s, and Brandt–Daroff group, respectively. They concluded Epley’s to be better for resolution of symptoms than Semont’s manoeuvre [3]. According to F Salvinelli et al., in 2003, 40 patients affected by PCBPPV were managed with Semont's manoeuvre. In the month following the procedure, 92.5% of patients of Semont's group showed resolution of symptoms [15]. Nadagoud et al., carried out a prospective randomized study in which they have compared the efficacy of Epley, Semont, and Gans manoeuvres in the treatment of posterior canal BPPV. The patients were uniformly randomized into three arms in equal numbers. All three manoeuvres showed equal efficacy in reducing vertigo [16]. Mishra et al., carried out a prospective randomized study on 200 patients using Epley’s and the Semont’s manoeuvre in the treatment of posterior canal benign paroxysmal positional vertigo in terms of subjective and objective improvement. Objective assessment was done using Dix–Hallpike positivity and subjective improvement was assessed using Dizziness Handicap Index (DHI). It concluded that both Epley’s and Semont’s are equally effective objectively. However, the subjective improvement was better in patients on whom Semont’s manoeuvre was performed [17]. Celis et al., conducted a single blinded RCT on 34 patients. Patients were randomly divided in four groups—Brandt–Daroff, “sham”, Semont and Epley. They concluded that Epley manoeuvre was superior to Brandt–Daroff, “sham” and Semont manoeuvres on nystagmus resolution and DHI improvement in patients with BPPV [18]. Kesimli MC et al., conducted a prospective randomized comparative study on sixty patients with posterior semicircular canal benign paroxysmal positional vertigo. Participants were randomly selected after the diagnostic tests for the Epley manoeuvre and the Semont manoeuvre treatment groups. They found that statistically significant difference was found between Epley and Semont groups regarding visual analogue scores at the one-week, two-week, and one-month follow-ups (p = 0.002, p < 0.001, p = 0.001, respectively). Hence, they concluded that Epley manoeuvre was significantly more effective than the Semont manoeuvre in resolving vertigo in the short-term treatment of posterior semicircular canal benign paroxysmal positional vertigo [19]. Michael Strupp et al. compared the effectiveness of the Semont manoeuvre and the Epley manoeuvre for treatment of posterior canal benign paroxysmal positional vertigo canalithiasis. They concluded that the Semont’s manoeuvre is superior to the Epley’s manoeuvre in terms of the number of days until recovery in posterior canal BPPV [20].
All the studies suggests that both Semont’s and Epley’s manoeuvre are almost equally efficacious in treating PC BPPV. The results of the earlier published studies are comparable to our results. There is an ongoing debate in the treatment methodology of cupulolithiasis with the belief that using mechanical vibration and repositioning together shows greater effect than repositioning alone. However, in our study there was no usage of mechanical vibration and results are comparable with previous studies. Dix–Hallpike test was done again after 02 weeks, and negative test suggests that the dislodged otoconia were repositioned back into the utricle from the semicircular canal.
Additionally, it was found that in older age group, patients were more comfortable while receiving the Semont’s manoeuvre as compared to the Epley’s due to sudden and greater degree of movement involved in the Epley’s manoeuvre. There was no such difference observed in the younger patients.
Dix–Hallpike result revealed that 95.3 and 90.6% patients improved in modified Epley’s and Semont’s group, respectively. p value is not significant, which concluded that there is no significant difference between the two tested manoeuvres. However, lack of post procedure postural restriction may increase patient satisfaction with Semont’s manoeuvre. Semont’s manoeuvre is easy to perform and equally effective in treating posterior canal BPPV as compared to modified Epley’s.
It has been observed that recovery rates were higher in the modified Epley’s group after the first manoeuvre, but it was significantly higher in the Semont’s group after the first repeat manoeuvre. There were 4 and 8 patients in the Modified Epley’s and Semont’s group, respectively, who were still symptomatic after the first manoeuvre. All patients of the Semont’s group recovered with only one repeat Semont’s manoeuvre. However, in Modified Epley’s group out of four patients, one recovered with 01 repeat manoeuvre, two recovered with 02, and one needed three repeat manoeuvres to recover.
Strengths of this study
-
1.
It is a randomized clinical trial.
-
2.
Large population size.
Limitations of this study
-
1.
Short follow-up of 2 weeks.
Conclusion
Our study found that both modified Epley’s and Semont’s manoeuvres are almost equally effective in treating cases of PC BPPV. However, in the group of patients who were still symptomatic after the first Semont’s manoeuvre, only one repeat manoeuvre was required for complete resolution of symptoms, whereas multiple repeat manoeuvres were needed in the modified Epley’s group. Semont’s manoeuvre is also comparatively easier to perform, require less number of repetitions, takes less time as there are less number of position changes, without any requirement of post-manoeuvre mobility restrictions. Hence, it is recommended that Semont’s manoeuvre can be routinely used for all patients of PC BPPV and can specifically be more useful in the older population and patients with spinal problems in whom sudden jerky movements are contraindicated.
Availability of data and materials
Original data are available on demand.
References
Dix R, Hallpike CS (1952) The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol 6:987–1016
von Brevern M (2013) Benign paroxysmal positional vertigo. Semin Neurol 33(03):204–211
Gupta AK, Sharma KG, Sharma P (2019) Effect of Epley’s, Semont’s Maneuvers and Brandt–Daroff exercise on quality of life in patients with posterior semicircular canal benign paroxysmal positional vertigo (PSCBPPV). Indian J Otolaryngol Head Neck Surg 71(1):99–103
Burton MJ, Eby TL, Rosenfeld RM (2012) Extracts from the Cochrane Library: modifications of the Epley (canalith repositioning) maneuver for posterior canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg 147:407–411
Baloh RW, Honrubia V, Jacobson K (1987) Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology 37(3):371
Hughes CA, Proctor L (1997) Benign paroxysmal positional vertigo. Laryngoscope 107(5):607–613
Schuknecht HF (1969) Cupulolithiasis. Arch Otolaryngol 90(6):765–778
Hall SF, Ruby RR, McClure JA (1979) The mechanics of benign paroxysmal vertigo. J Otolaryngol 8(2):151–158
Fife TD, Iverson DJ, Lempert T, Furman JM, Baloh RW, Tusa RJ, Hain TC, Herdman S, Morrow MJ, Gronseth GS (2008) Practice parameter: therapies for benign paroxysmal positional vertigo (an evidence-based review): [RETIRED] Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 70(22):2067–2074
Herdman SJ, Tusa RJ, Zee DS, Proctor LR, Mattox DE (1993) Single treatment approaches to benign paroxysmal positional vertigo. Arch Otolaryngol Head Neck Surg 119(4):450–454
Ramakrishna J, Goebel JA, Parnes LS (2012) Efficacy and safety of bilateral posterior canal occlusion in patients with refractory benign paroxysmal positional vertigo: case report series. Otol Neurotol 33(4):640–642
Joshi D, Gyanpuri V, Pathak A, Chaurasia RN, Singh V, Dhiman NR (2021) Epley Maneuver versus Gans repositioning maneuver in treating posterior canal BPPV and familial incidence of BPPV: protocol for a randomized controlled trial. Indian J Otolaryngol Head Neck Surg 20:1–6
Sen K, Sarkar A, Raghavan A (2016) Comparative efficacy of epley and semont maneuver in benign paroxysmal positional vertigo: a prospective randomized double-blind study. Astrocyte 3(2):96
Ajayan PV, Aleena PF, Jacob AM (2017) Epley’s maneuver versus Semont’s maneuver in treatment of posterior canal benign positional paroxysmal vertigo. Int J Res Med Sci 5:2854–2860
Salvinelli F, Casale M, Trivelli M et al (2003) Benign paroxysmal positional vertigo: a comparative prospective study on the efficacy of Semont’s maneuver and no treatment strategy. La ClinicaTerapeutica. 154(1):7–11
Nadagoud SV, Bhat VS, Pragathi BS (2023) Comparative efficacy of Epley, Semont and Gans Maneuver in treating posterior canal benign paroxysmal positional vertigo. Indian J Otolaryngol Head Neck Surg 25:1–7
Mishra P, Sindhu KL, Chethana R, Kaushik M (2023) Epleys versus semont’s manoeuvre in posterior canal benign paroxysmal positional vertigo. Indian J Otolaryngol Head Neck Surg 75(Suppl 1):523–527
Celis-Aguilar E, Mayoral-Flores HO, Torrontegui-Zazueta LA, Medina-Cabrera CA, León-Leyva IC, Dehesa-López E (2022) Effectiveness of Brandt Daroff, Semont and Epley maneuvers in the treatment of Benign Paroxysmal Positional Vertigo: a randomized controlled clinical trial. Indian J Otolaryngol Head Neck Surg 1:1–8
Kesimli MC, Kaya D, Ceylan S, Ceylan A, Ünal M. The efficacy of Epley and Semont maneuvers in posterior semicircular canal benign paroxysmal positional vertigo treatment: a short-term comparative study
Strupp M, Mandala M, Vinck AS, Van Breda L, Salerni L, Gerb J, Bayer O, Mavrodiev V, Goldschagg N (2023) The Semont-Plus Maneuver or the Epley maneuver in posterior canal benign paroxysmal positional vertigo: a randomized clinical study. JAMA Neurol 80(8):798–804
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Ethical approval
Study protocol was performed according to ethical guidelines of the 2002 Declaration of Helsinki, and carried out after approval by the Institutional Review Board and Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thakur, B., Raj, P., Singh, K. et al. To compare the recovery rates of modified Epley’s against Semont’s manoeuvres in patients with posterior canal benign paroxysmal positional vertigo: a randomized clinical trial. Eur Arch Otorhinolaryngol 281, 4641–4648 (2024). https://doi.org/10.1007/s00405-024-08657-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-024-08657-2