Abstract
Purpose
The aim of this prospective study was to examine the characteristics of a clinical test for the assessment of nasal trigeminal sensitivity to mechanical stimuli and its association with the perception of nasal patency.
Methods
Thirty-two normosmic healthy subjects participated (17 women and 15 men; age = 26 ± 3 years). Precisely defined air puffs were used with a flow rate of 2L/min for mechanical stimulation. They were presented to the nasal vestibule, nasal septum, and inferior turbinate with various stimulus durations. Thresholds were measured by single-staircase stimuli with changes in stimulus duration in steps of 10 ms. Trigeminal suprathreshold intensity was rated by subjects for stimulus durations of 200, 300, 400, and 500 ms. Test–retest reliability was examined by intraclass correlations (ICCs) and Bland–Altman plot with limits of agreement. Pearson’s correlations were calculated between self-rated nasal patency and nasal trigeminal sensitivity.
Results
As indicated by trigeminal threshold and suprathreshold intensities, the nasal vestibule is the most sensitive area among the three locations, followed by the nasal septum and the inferior turbinate (p < 0.001). Coefficients of correlations between test and retest were 0.76 for thresholds, and 0.56 suprathreshold intensities (p < 0.001). The Bland–Altman analysis showed a good agreement between test–retest values. In addition, significant positive associations between trigeminal suprathreshold intensities and self-rated nasal obstruction were found at the inferior turbinate (r = 0.4, p < 0.05).
Conclusion
Reliable assessment of nasal trigeminal sensitivity for air puffs appears to be possible. Nasal trigeminal suprathreshold sensitivity to mechanical stimuli is associated with the perception of nasal patency at the inferior turbinate. This opens a window into the assessment of the perception of nasal airflow in various clinical purposes, especially for patients with sinonasal diseases.
Level of evidence
3.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasal obstruction, the sensation of reduced nasal airflow or nasal patency, is one of the most common symptoms associated with upper airway diseases. Approximately one-third of the general adult population complain of nasal obstruction [1]. Nasal obstructions could lead to worse sleep, daytime sleepiness as a result and increased fatigue, which limits the quality of life, could be related to symptoms of depression and negatively affects productivity [2, 3].
Nasal airflow is conditioned by an open nasal passage, intact mucociliary function, functioning airflow receptors, and intact mucosa without inflammation. From the complex conditions, it follows that nasal obstruction often is multifactorial due to anatomic, physiologic, pathophysiologic, and iatrogenic factors [4].
Various methods can be used to measure nasal obstruction. Regarding more objective measurements, current methods attempt to determine how much nasal obstruction can be attributed to anatomical features, including rhinomanometry to measure nasal airway resistance, acoustic rhinometry to measure the volume of the nasal cavity, or peak nasal flow measurements (PNIF) to measure inspiratory airflow. These methods evaluate different aspects of nasal obstruction, are correlated with each other, and can be used in both research and clinical settings; for example, when measuring nasal resistance, cross-sectional diameter, and airflow before and after application of a nasal decongestant, the comparative analyses allow to assess whether symptoms are attributable to functional or structural obstruction. PNIF can also be used for testing nasal hyper-reactivity and assessing the effects of environmental factors on nasal patency [5, 6]. Patient-reported measures for nasal obstruction include the Nasal Obstruction Symptom Evaluation score (NOSE) or ratings on visual analog scales (VAS). The patient-reported measures have been considered as a reliable and consistent tool for the evaluation of nasal obstruction and are recommended to assess for the scoring of the severity of nasal obstruction [7]. As the primary consideration in diagnosing the condition is the patient’s perception of the severity of congested symptoms, the patients’ reports are important in estimating the success of surgical interventions. However, patient dissatisfaction rates after surgery for nasal obstruction are as high as 30%, while long-term studies report an even higher failure over time [8, 9]. It has been tried to correlate these objective and patient-reported measures in several studies; however, a few studies indicate strong statistical correlations [10, 11]. Given such discrepancy between subjective perception and clinical examination, it appears that otolaryngologists are not in agreement on the standard methods of assessing nasal obstruction, and that this calls for the development of better methods.
Physiologically, the nasal airflow is changed from laminar to nonlaminar mainly due to the turbinates which leads to a change of the temperature [12]. Increasing evidence suggests that perceived nasal obstruction is not always determined by airflow resistance or objectively measured nasal patency but rather the affected nasal trigeminal activation [13,14,15]. Nasal trigeminal nerves mediate the presence of thermal, mechanical, and chemical stimuli, for example, menthol or eucalyptol. Thus, exposure to menthol, via activation of transient receptor potential melastatin family member 8 (‘TRPM8’) receptors, causes the sensation of coolness and better nasal patency, although nasal structures are not changed significantly [16]. To the contrary, one interesting observation is that topical anesthesia of the nasal vestibule resulted in a sensation of the congested nose, presumably caused by the blocked afferent trigeminal nerve [17]. Additionally, patients with deviated septum who complain nasal obstruction are traditionally considered to result directly from obstruction; however, these patients have been shown to have a decreased trigeminal sensitivity [14, 18]. Trigeminal sensation plays a role in the sensation of nasal obstruction in chronic rhinosinusitis, as well [19]. Also, empty nose syndrome patients with the feeling of congestion expressed a lower nasal trigeminal receptor and exhibited decreased trigeminal functionality [20, 21].
Several tools for evaluating the nasal trigeminal function in humans have been proposed, asking the subjects to rate, differentiate, or localize trigeminal chemosensory stimulus, such as ethanol, propanediol, menthol, butanol, and cinnamaldehyde [22, 23]. However, due to close relationship between the olfactory and the trigeminal systems, the challenge with these tools is that the stimuli also produce olfactory mediated sensations which contaminates the precision of the ratings of trigeminal sensations [24]. One solution for this issue is to activate trigeminal afferents using gaseous CO2, which has little or no smell [25]. Another more “natural” stimuli way in research is the use of air puffs, which appears to be close to “real life” situations. In Clark and Jones' study of nasal sensitivity to air jets, they found that sensitivity was greatest in the nasal vestibules [26]. After measuring the sensitivity threshold to air jets in nine locations throughout 141 nasal cavities, Wrobel et al. emphasized decreased mechano-sensitivity with increasing age [27]. However, clinically, it is not clear how nasal mechanoreception contributes to subjective nasal patency. Currently, while there are several instruments available to measure nasal trigeminal function, none have been widely adopted in routine clinical practice.
In this study, we aimed to examine the characteristics of a clinical test for the assessment of nasal trigeminal sensitivity to mechanical stimuli and association with perception of nasal patency. Accordingly, we constructed a device with precisely defined air puffs, which were presented to several intranasal sites in a group of healthy volunteers. To characterize the model, we assessed the trigeminal threshold and intensity ratings of trigeminal suprathreshold stimuli. We also investigated the test–retest reliability, as well as the perception of nasal patency. In doing so, we tried to develop and validate an easy-to-use tool to evaluate intranasal trigeminal sensitivity to mechanical stimuli with precisely defined air puffs. This should allow to characterize how nasal trigeminal sensitivity to mechanical stimuli contributes to an individual’s perception of nasal patency. We hypothesized that different nasal sites have different nasal trigeminal sensitivity, and nasal trigeminal sensitivity will be associated with the perception of nasal patency. To quantify nasal obstruction may help to develop a clinical assessment, applying for surgical planning or identification of patients at high risk for treatment failure.
Methods
This prospective study was conducted at the Smell & Taste Clinic, Department of Otorhinolaryngology of the TU Dresden. It was approved by the University of Dresden Medical Faculty Ethics Review Board (application number EK-74022022). Informed written consent was obtained from all the participants. The study was performed in accordance with the Declaration of Helsinki on Biomedical Studies Involving Human Subjects.
Subjects
Eligible participants were aged 18–65 years. All were in good health and only those declaring a normal sense of smell were included. Participants were excluded if they: (1) had neurological or psychiatric diseases; (2) had any rhinological conditions such as major septal deviations, as assessed using nasal endoscopy; (3) had any medicine intranasally applied prior to screening; (4) had undergone any nasal surgery during the 6 months preceding the screening; (5) pregnant women, or those with an upper respiratory tract infection at the time of testing. Subjects were instructed not to have smoking, eating, or drinking anything but water for at least 1 h leading up to the test.
Measures
Both demographic and clinical data were collected from all subjects using a standardized questionnaire.
Trigeminal stimulus device
The device gave precisely defined air puffs. It consisted of five modules (Fig. 1): (1) stimuli were delivered by a portable air compressor (1.0 Gallon Air Tank, VIAIR, California); (2) pressure reducer and pressure regulator; (3) airflow sensor (SFC5400, Sensirion AG, Stäfa) with valve controlled by computer, which allowed the release of air stimulus with desired scenario (in terms of various volumes or durations); (4) long transport tube; (5) stimuli were presented through a standard plastic nasal cannula (20 gauge, Vasofix® Safety, Germany).
A Schematic diagram shows the general layout of the air-puffs’ delivery device; B stimuli were delivered by a portable air compressor (1.0 Gallon Air Tank, VIAIR, California); C pressure reducer and pressure regulator; D airflow sensor (SFC5400, Sensirion AG, Stäfa) with valve controlled by computer; E standard plastic nasal cannula (20 gauge, Vasofix® Safety, Germany) held with the fixed frame presents the stimuli and the nasal cannula points to the inferior turbinate; IT inferior turbinate, NS nasal septum
Trigeminal stimulus procedure
An important aim of the design of this study was to allow for the comparison of trigeminal sensitivity on different locations of nasal cavity. For this purpose, different sites were tested, including (1) the lateral wall of the nasal vestibule, proximate to the epithelial–mucosal junction, (2) the anterior aspect of the inferior turbinate, and (3) the nasal septum, directly opposite the anterior aspect of the inferior turbinate.. The sequence of stimulations of the various locations was randomly distributed across participants. To avoid nasal respiratory airflow during tests, participants were asked to breathe through their mouth. To avoid visual distraction, participants were asked to close eyes. To avoid auditory distraction, noise canceling headphones were used with continuous white noise to mask any noise generated by the air control system and the sound when air puff passing through the nozzle. Under endoscopic control, the needle cannula was presented toward the predetermined sites above the mucosal surface with approximately 2 mm under direct vision with a 0-degree rigid nasal endoscope (0°, KARL STORZ, Tuttlingen, Germany). Groups of stimuli were presented to the right nostril using different stimulus durations which were perceived with different intensities. The total flow rate was set at 2 l/min with an interval of 10 s between stimuli to avoid adaptation. The procedure lasted around 30 min for each subject. The test was repeated on another day within a fortnight with ten subjects.
Trigeminal thresholds
The stimuli were presented in a single-staircase method [28]: The first stimulus was delivered in ascending order, starting at the subthreshold levels (for example, lowest duration 5 s), in 10 ms increments, until the participant detected the target twice in a row. This correct detection triggered a reversal of stimulus presentation with reduced duration—until detection failed, and then, the stimulus duration increased again (1 up 2 down stopping rule). The procedure stopped when seven reversals were obtained. The average score of the last four reversal points represented the participant’s air puff threshold.
Trigeminal suprathreshold intensity rating
Suprathreshold air flow stimuli were applied to each predetermined nasal site. Sequences of four air puffs with different durations of 200, 300, 400, and 500 ms in a pseudo-randomized order at intervals of 10 s were delivered. Subjects verbally rated the intensity of each air puff on a numerical rating scale ranging from 1 (very weak) to 10 (extremely strong). The “mean intensity ratings” for each site were obtained by the average of four ratings as this reflected a baseline stage of intensity perception. The “Temporal Summation (TS) rating” was the 500 ms intensity minus the 200 ms intensity rating, which was considered to represent the slope or the amount of temporal summation.
Self-rated nasal patency
The visual analog scale score (VAS) for self-rated nasal patency of the right nostril was obtained. It consisted of ten points, where “1” indicated very poor nasal patency and “10” indicated very good nasal patency.
Statistical analysis
Data analysis was performed in SPSS 26.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were calculated for all variables. Normality of data was tested using Shapiro–Wilk test. Homogeneity of variances was tested using the Levene’s test. For trigeminal threshold, a one-way analysis of variance (ANOVA) with repeated measures was used to identify the effects of each site on threshold. To determine the effect of different site over duration on trigeminal suprathreshold intensity in study subjects, a two-way ANOVA for repeated measures was performed. Post hoc mean comparisons with the Bonferroni test were used to identify specific site, gender, or stimulation durations which exhibited significant differences. Pearson correlations were calculated between self-rated nasal patency and nasal trigeminal sensitivity (trigeminal thresholds, TS intensity rating, mean intensity ratings, and intensity rating of 200 ms, 300 ms, 400 ms, and 500 ms). Pearson statistics were performed for correlation analysis. The alpha level was set at 0.05. Test–retest reliability (repeatability) of trigeminal threshold and suprathreshold intensity was determined via calculation of the Intraclass Correlation Coefficient (ICC), with the ICC values < 0.4 considered poor, 0.4–0.75 fair to good, and > 0.75 excellent. We also constructed a Bland–Altman Plot and reported mean difference and limits of agreement. A range of agreement was defined as mean bias ± 2 SD. Repeatability was reported via the coefficient of repeatability and its precision, as described by Bland et al. [29].
Results
Participant characteristics
Thirty-two healthy, normosmic participants (17 women and 15 men; age = 26 ± 3 years) were included in the study. Table 1 shows the demographic and baseline clinical characteristics.
Trigeminal threshold
According to Mauchly's test of sphericity, the variance–covariance matrix of dependent variables is equal (χ2 = 1.241, p = 0.538). There was a significant effect of the trigeminal threshold in the examined areas (F(2.0, 64.0) = 16.7, p < 0.001), showing a lower trigeminal threshold at nasal vestibule (37.4 ± 22.5 ms) compared to nasal septum (66.2 ± 48.1 ms; p < 0.001) and inferior turbinate (67.9 ± 45.6 ms, p < 0.001) (Fig. 2).
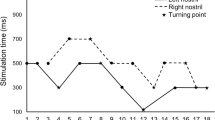
Trigeminal suprathreshold intensity
A main effect of stimulation duration for intensity ratings of trigeminal suprathreshold stimuli was found (F(3.0, 96) = 57.2, p < 0.001), showing that participants rated the intensity to mechanical stimuli higher when the duration increased (Fig. 3). A main effect of stimulation site for intensity rating was found (F(2.0, 64) = 13.7, p < 0.001). Intensity ratings at nasal vestibule [6.4, 95% CI (5.8, 7.1)] were higher than at the nasal septum [5.2, 95% CI (4.6, 5.9)] and the inferior turbinate [4.9 ± 0.3, 95% CI (4.2, 5.5)]. There was no interaction effect of stimulation site and duration for intensity ratings (p = 0.30).
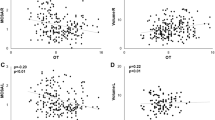
Test–retest reliability
The values of trigeminal threshold obtained by mechanical stimuli showed good ICC levels for intra reliability, specifically, 0.61 (p < 0.05) for inferior turbinate, 0.63 (p < 0.05) for nasal vestibule, except for the point on the nasal septum, which presented an excellent ICC value for intra rater reliability (ICC = 0.90, p < 0.05).
Test–retest Bland–Altman analysis for trigeminal threshold at three nasal positions revealed good mean agreement and narrow limits of agreement across the two tests (Fig. 4). For the interior turbinate, mean difference was 7.5 and limits of agreement − 17 to 32.4. For the nasal septum, mean difference was 9.0 and limits of agreement − 52.3 to 70.3. For the nasal vestibule, mean difference was 5.6 and limit of agreement − 23.3 to 34.6.
ICC scores for the values of trigeminal suprathreshold intensity of the first and second assessments ranged from 0.46 to 0.59 (0.59 for nasal vestibule, 0.54 for nasal septum, and 0.46 for inferior turbinate, all p < 0.05).
Bland–Altman plots for trigeminal suprathreshold (Fig. 4) showed that this test was generally repeatable with the mean difference falling within the RC limits for the majority of subjects. This indicates a high level of repeatability for this measure [30]. For the inferior turbinate, mean difference was − 0.4 and limits of agreement − 2.2 to 1.4. For the nasal septum, mean difference was 0.9 and limits of agreement − 2.9 to 4.6. For the nasal vestibule, mean difference was − 0.3 and limit of agreement − 2.9 to 2.3.
There was no correlation found for trigeminal threshold and self-rated nasal obstruction at the different areas (nasal vestibule, nasal septum, and inferior turbinate, all p > 0.05).
Correlations among trigeminal suprathreshold intensity and self-rated nasal obstruction
At nasal vestibule
Overall, trigeminal suprathreshold intensity, including TS and Mean intensity ratings, had no significant association with self-rated nasal obstruction (p > 0.05), only TS had a weak negative association with intensity rating at 300 ms (r = − 0.36, p < 0.05), and a weak positive association with intensity rating at 500 ms (r = 0.35, p < 0.05).
At nasal septum
Overall, trigeminal suprathreshold intensity, including TS and mean intensity rating, had no significant association with self-rated nasal obstruction (p > 0.05), and only TS had moderate positive association with intensity rating at 500 ms (r = 0.59, p < 0.05).
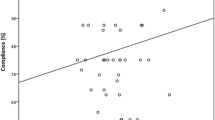
At inferior turbinate
Correlation analysis revealed significant positive correlations between intensity ratings at 300 ms (r = 0.35, p < 0.05), intensity ratings at 400 ms (r = 0.43, p < 0.05) (Fig. 5), mean intensity ratings (r = 0.36, p < 0.05), and self-rated nasal obstruction. TS had a weak negative association with intensity rating at 200 ms (r = − 0.35, p < 0.05), and positive association with intensity ratings at 400 ms (r = 0.35, p < 0.05) and intensity ratings at 500 ms (r = 0.69, p < 0.05).
Discussion
In this study, we investigated thresholds as well as suprathreshold measures of nasal trigeminal sensitivity to mechanical stimuli, shown to relate to the perception of nasal patency. To accomplish this, first, we constructed a device to produce precisely timed quantifiable natural air stimuli, and demonstrated good test–retest reliability regarding measurement of nasal trigeminal sensitivity. Second, we compared the trigeminal sensitivity among different nasal sites, and found the nasal vestibule to be significantly more sensitive to mechanical stimuli than the nasal septum and the inferior turbinate. Third, we tested for correlations between nasal trigeminal sensitivity to mechanical stimuli and perception of nasal patency, and demonstrated suprathreshold rating at inferior turbinate is correlated to the perception of nasal patency. Therefore, these data indicated that the lining of nasal cavity is not a homogeneous tissue, and nasal trigeminal sensitivity to mechanical stimuli is one of the underlying factors contributing to the sensation of nasal patency.
Our study suggested that the nasal vestibule is more sensitive to mechanical stimuli of air puffs compared to inferior turbinate and anterior septum. This result coincides with the previous research, where the nasal vestibule is considered to be the predominant area for sensing nasal airflow. Jones et al. [17] reported that local anesthesia of the nasal vestibule causes the feeling of nasal obstruction, but anesthesia of the nasal mucosa had no such effect. Similar results have been reported by Clarke and Jones, they observed that the nasal vestibule is the most sensitive area to mechanical stimulations [26]. From the perspective of histology, one obvious explanation can be, the lining of nasal vestibule is the skin continued with that of external nose and is comprised of keratinized stratified squamous epithelium, while the lining of the posterior nose becomes pseudostratified columnar respiratory epithelium posteriorly just starting from piriform aperture. In other word, nasal trigeminal sensitivity seems to vary according to the type of tissue [31]. Moreover, support for different sensitivity in different areas of the nasal mucosa can be found in the literature [27]. Measuring trigeminal sensitivity to different type and site of stimulation, the most sensitivity area to CO2 stimuli was the mucosa of anterior septum, while the most sensitivity area to mechanical stimuli was the mucosa of posterior septum [32]. Interestingly, previous work demonstrated an anterior–posterior gradation of nasal trigeminal sensitivity [27]. In line with this, several studies identify the heterogeneous distribution of trigeminal sensory receptors throughout the nasal cavity. The distribution density of thermoreceptors was higher in the nasal vestibule than in the nasal cavum or adjacent cheekbones’ skin. Opposite to this result, the recent study shown that the highest trigeminal receptor RNA expression was found in the posterior nasal mucosa [33, 34]. Taken together, these studies suggest that the mucosa of the nasal cavity is not a homogeneous tissue, logically, reflected by the various degrees of trigeminal sensitivity.
We could further demonstrate that the nasal trigeminal sensitivity to mechanical stimuli correlated with the subjective nasal patency. The perception of nasal patency is traditionally thought to be dependent on direct physical factors, such as cross-sectional areas of a nasal cavity or the nasal airway resistance. There are several causes for changes of physical factors, including chronic inflammation and mechanical obstruction, such as septal deviation, leading to lower nasal patency. Objective measurements of the physical factors are available using peak nasal inspiratory flow, rhinomanometry and acoustic rhinometry, etc. However, these objective measurements do not always correlate to the subjective sensation of nasal patency. The correlation we found between nasal trigeminal sensitivity to mechanical stimuli and subjective nasal patency is in line with the recent increasing evidence of a potential role of trigeminal sensitivity in the perception of nasal patency. For example, some patients complain about low nasal patency, but without obvious structural obstruction or chronic inflammation. This may be due to insensitivity of the trigeminal nerve [35]. Low intranasal trigeminal sensitivity is related to worse rate of postoperative satisfaction after septal surgery [14]; notably, intranasal trigeminal sensitivity may be impaired after functional nasal surgery [36]. In addition, impaired trigeminal sensitivity may also play a role in the pathophysiology of patients suffering from empty nose syndrome, who experience a paradoxical sensation of nasal patency [21]. Although our study focused on nasal trigeminal sensitivity to mechanical stimuli, the trigeminal nerve responds to multimodal activation, for example, temperature change of nasal lining or mucosal cooling. A growing body of evidence indicates that the sensation of nasal patency may be secondary to nasal mucosal temperature changes [37,38,39]. Using a non-contact temperature probe, Willat and Jone found that lower nasal mucosal temperatures were associated with greater nasal patency reported by patients [40]. Computed fluid dynamics studies have shown the significant correlation between the peak heat loss and perception of nasal patency [37]. Other studies show that mucosal cooling is processed via activation of TRPM8 receptors [41, 42]. This receptor responds to temperatures between 8 and 25 °C. Of note, our study used trigeminal mechanical stimulation with air puffs, which produces mechanical shear stress at the nasal mucosa, but could also produce mucosal temperature changes. In other words, the correlation we found between mechanical stimuli and perception of nasal patency is mediated not only through mechanoreceptors, but might also involve TRPM8 [16]. Most interestingly, compared to the areas of laminar airflow, temperature changes are more prominent near areas of turbulent airflow [43], specifically around the mucosa of the turbinates. In line with this finding, we demonstrated that trigeminal sensitivity at the mucosa of the inferior turbinate, but not the nasal septum, is correlated with the perception of nasal patency. This emphasizes the important role of the inferior turbinate contributing to the perception of nasal patency, helping to understand the alteration of perception of nasal patency after removal of the inferior turbinate.
This study has some limitations, first, it is worth to note that we did not control the nasal cycle, a normal condition characterized by the alternation of nasal airflow asymmetry. Future studies should take this question into account. Second, the cross-sectional results cannot give the answer on causation between nasal obstruction ratings and trigeminal sensitivity, and future longitudinal studies should be designed.
Despite these limitations, the present study suggests that measuring nasal trigeminal sensitivity to mechanical stimuli is reliable and interesting, because it extends the current understanding of nasal patency perception. When patients complain of low nasal patency, this should be considered not just as a problem of nasal resistance or nasal anatomy, but should also be considered in terms of trigeminal sensitivity. Despite the correlation coefficient of 0.4 identified in our study, it is crucial to interpret this correlation with caution. We must specifically elucidate the extent to which trigeminal sensitivity influences nasal obstruction. Future research should quantify the impact of nasal mechano-sensitivity on the perception of nasal airway obstruction in patients and compare our air puff tool with the established methods like the lateralization task to determine the sensitivity, specificity, and accuracy of the air puff tool for assessing intranasal trigeminal sensitivity. Simple clinical tools should be developed and more research is needed for the assessment of nasal mechanical sensations.
Conclusion
Reliable assessment of nasal trigeminal sensitivity with air puffs appears to be possible. The preliminary results suggested that the nasal trigeminal sensitivity to mechanical stimuli is associated with the perception of nasal patency. Although it is likely just one piece of a larger puzzle, this is valuable to open a window into the assessment of the perception of nasal airflow in various clinical populations, e.g., patients with sinonasal disorders.
References
Wever CC (2016) The nasal airway: a critical review. Facial Plast Surg 32:17–21. https://doi.org/10.1055/s-0035-1570323
Stull DE, Roberts L, Frank L, Heithoff K (2007) Relationship of nasal congestion with sleep, mood, and productivity. Curr Med Res Opin 23:811–819. https://doi.org/10.1185/030079907x178793
Phillips KM, Hoehle LP, Bergmark RW et al (2017) Association between nasal obstruction and risk of depression in chronic rhinosinusitis. Otolaryngol Head Neck Surg 157:150–155. https://doi.org/10.1177/0194599817696294
Hsu DW, Suh JD (2018) Anatomy and physiology of nasal obstruction. Otolaryngol Clin North Am 51:853–865. https://doi.org/10.1016/j.otc.2018.05.001
Segboer CL, Holland CT, Reinartz SM et al (2013) Nasal hyper-reactivity is a common feature in both allergic and nonallergic rhinitis. Allergy 68:1427–1434. https://doi.org/10.1111/all.12255
Ottaviano G, Staffieri A, Stritoni P et al (2012) Nasal dysfunction induced by chlorinate water in competitive swimmers. Rhinology 50:294–298. https://doi.org/10.4193/Rhino11.024
van Spronsen E, Ingels KJO, Jansen AH et al (2008) Evidence-based recommendations regarding the differential diagnosis and assessment of nasal congestion: using the new GRADE system. Allergy 63:820–833. https://doi.org/10.1111/j.1398-9995.2008.01729.x
Konstantinidis I, Triaridis S, Triaridis A et al (2005) Long term results following nasal septal surgery. Focus on patients’ satisfaction. Auris Nasus Larynx 32:369–374. https://doi.org/10.1016/j.anl.2005.05.011
Sundh C, Sunnergren O (2015) Long-term symptom relief after septoplasty. Eur Arch Otorhinolaryngol 272:2871–2875. https://doi.org/10.1007/s00405-014-3406-7
Lam DJ, James KT, Weaver EM (2006) Comparison of anatomic, physiological, and subjective measures of the nasal airway. Am J Rhinol 20:463–470. https://doi.org/10.2500/ajr.2006.20.2940
André RF, Vuyk HD, Ahmed A et al (2009) Correlation between subjective and objective evaluation of the nasal airway. A systematic review of the highest level of evidence. Clin Otolaryngol 34:518–525. https://doi.org/10.1111/j.1749-4486.2009.02042.x
Sozansky J, Houser SM (2014) The physiological mechanism for sensing nasal airflow: a literature review. Int Forum Allergy Rhinol 4:834–838. https://doi.org/10.1002/alr.21368
Migneault-Bouchard C, Boselie FJM, Hugentobler M et al (2021) Trigeminal impairment in treatment-refractory chronic nasal obstruction. Rhinology 59:312–318. https://doi.org/10.4193/Rhin20.510
Scheibe M, Schulze S, Mueller CA et al (2014) Intranasal trigeminal sensitivity: measurements before and after nasal surgery. Eur Arch Otorhinolaryngol 271:87–92. https://doi.org/10.1007/s00405-013-2466-4
Sozansky J, Houser SM (2015) Pathophysiology of empty nose syndrome. Laryngoscope 125:70–74. https://doi.org/10.1002/lary.24813
Voets T, Owsianik G, Nilius B (2007) TRPM8. Handb Exp Pharmacol. https://doi.org/10.1007/978-3-540-34891-7_20
Jones AS, Crosher R, Wight RG et al (1987) The effect of local anaesthesia of the nasal vestibule on nasal sensation of airflow and nasal resistance. Clin Otolaryngol Allied Sci 12:461–464. https://doi.org/10.1111/j.1365-2273.1987.tb00233.x
Malik J, Spector BM, Wu Z et al (2021) Evidence of Nasal Cooling and Sensory Impairments Driving Patient Symptoms With Septal Deviation. 9
Saliba J, Fnais N, Tomaszewski M et al (2016) The role of trigeminal function in the sensation of nasal obstruction in chronic rhinosinusitis. Laryngoscope 126:E174-178. https://doi.org/10.1002/lary.25952
Konstantinidis I, Tsakiropoulou E, Chatziavramidis A et al (2017) Intranasal trigeminal function in patients with empty nose syndrome. Laryngoscope 127:1263–1267. https://doi.org/10.1002/lary.26491
Kanjanawasee D, Campbell RG, Rimmer J et al (2021) Empty nose syndrome pathophysiology: a systematic review. Otolaryngol Head Neck Surg. https://doi.org/10.1177/01945998211052919
Huart C, Hummel T, Kaehling C et al (2019) Development of a new psychophysical method to assess intranasal trigeminal chemosensory function. Rhinology 57:375–384. https://doi.org/10.4193/Rhin19.024
Hummel T (2000) Assessment of intranasal trigeminal function. Int J Psychophysiol 36:147–155. https://doi.org/10.1016/s0167-8760(99)00108-7
Hummel T, Livermore A (2002) Intranasal chemosensory function of the trigeminal nerve and aspects of its relation to olfaction. Int Arch Occup Environ Health 75:305–313. https://doi.org/10.1007/s00420-002-0315-7
Hummel T, Kaehling C, Grosse F (2016) Automated assessment of intranasal trigeminal function. Rhinology 54:27–31. https://doi.org/10.4193/Rhino15.002
Clarke RW, Jones AS (1994) The distribution of nasal airflow sensitivity in normal subjects. J Laryngol Otol 108:1045–1047. https://doi.org/10.1017/s0022215100128853
Wrobel BB, Bien AG, Holbrook EH et al (2006) Decreased nasal mucosal sensitivity in older subjects. Am J Rhinol 20:364–368. https://doi.org/10.2500/ajr.2006.20.2862
Ehrenstein WH, Ehrenstein A (1999) Psychophysical methods. In: Windhorst U, Johansson H (eds) Modern techniques in neuroscience research. Springer, Berlin, pp 1211–1241
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8:135–160. https://doi.org/10.1177/096228029900800204
Bloom JD, Antunes MB, Becker DG (2011) Anatomy, physiology, and general concepts in nasal reconstruction. Facial Plast Surg Clin North Am 19:1–11. https://doi.org/10.1016/j.fsc.2010.10.001
Frasnelli J, Heilmann S, Hummel T (2004) Responsiveness of human nasal mucosa to trigeminal stimuli depends on the site of stimulation. Neurosci Lett 362:65–69. https://doi.org/10.1016/j.neulet.2004.02.059
Jones AS, Wight RG, Durham LH (1989) The distribution of thermoreceptors within the nasal cavity. Clin Otolaryngol Allied Sci 14:235–239. https://doi.org/10.1111/j.1365-2273.1989.tb00367.x
Poletti SC, Hausold J, Herrmann A et al (2019) Topographical distribution of trigeminal receptor expression in the nasal cavity. Rhinology 57:147–152. https://doi.org/10.4193/Rhin18.181
Bischoff S, Poletti SC, Kunz S et al (2020) Trigeminal endonasal perception - an outcome predictor for septoplasty. Rhinology 58:437–443. https://doi.org/10.4193/Rhin19.292
Migneault-Bouchard C, Boselie FJM, Landis BN, Frasnelli J (2022) Intranasal trigeminal sensitivity may be impaired after functional nasal surgery. RHINOL 5:8–9. https://doi.org/10.4193/RHINOL/21.049
Zhao K, Jiang J, Blacker K et al (2014) Regional peak mucosal cooling predicts the perception of nasal patency. Laryngoscope 124:589–595. https://doi.org/10.1002/lary.24265
Zhao K, Blacker K, Luo Y et al (2011) Perceiving nasal patency through mucosal cooling rather than air temperature or nasal resistance. PLoS ONE 6:e24618. https://doi.org/10.1371/journal.pone.0024618
Tjahjono R, Singh N (2021) Correlation between nasal mucosal temperature change and the perception of nasal patency: a literature review. J Laryngol Otol 135:104–109. https://doi.org/10.1017/S0022215121000487
Willatt DJ, Jones AS (1996) The role of the temperature of the nasal lining in the sensation of nasal patency. Clin Otolaryngol Allied Sci 21:519–523. https://doi.org/10.1111/j.1365-2273.1996.tb01102.x
Lumpkin EA, Caterina MJ (2007) Mechanisms of sensory transduction in the skin. Nature 445:858–865. https://doi.org/10.1038/nature05662
Frasnelli J, Albrecht J, Bryant B, Lundström JN (2011) Perception of specific trigeminal chemosensory agonists. Neuroscience 189:377–383. https://doi.org/10.1016/j.neuroscience.2011.04.065
Lindemann J, Leiacker R, Rettinger G, Keck T (2002) Nasal mucosal temperature during respiration. Clin Otolaryngol Allied Sci 27:135–139. https://doi.org/10.1046/j.1365-2273.2002.00544.x
Funding
The authors have no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial relationships, or conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, X., Menzel, S., Zhao, K. et al. Intranasal trigeminal sensitivity to mechanical stimuli is associated with the perception of nasal patency. Eur Arch Otorhinolaryngol 280, 5391–5399 (2023). https://doi.org/10.1007/s00405-023-08126-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08126-2