Abstract
Background
Non-allergic rhinitis (NAR) in children, named local allergic rhinitis (LAR) and non-allergic rhinitis with eosinophilia syndrome (NARES), are recently termed entities in childhood characterized by symptoms suggestive of allergic rhinitis in the absence of systemic atopy. Nasal eosinophils (nEo) are the principal cells involved in the allergy inflammation and nasal allergen provocation test is the gold standard method for the diagnosis, albeit with several limitations. The aim of this study was to validate the presence of nEo in combination with the therapeutic response to nasal steroids, as a preliminary discriminator of NAR in real life data.
Methods
In a prospective cohort study, 128 children (63.3% male, aged 72 ± 42 m) with history of NAR were enrolled and followed up for 52 ± 32 m. Nasal cytology was performed and nasal steroids trial was recommended initially in all and repeatedly in relapsing cases. Response to therapy was clinically evaluated using 10-VAS.
Results
Significant nEo was found in 59.3% of the cases and was related to reported dyspnea episodes. 23.4% had no response to therapy, whereas 51.5% were constantly good responders. Response to therapy was related to nEo and a cutoff point of 20% was defined as the most reliable biological marker with 94% sensitivity and 77% specificity.
Conclusions
In children with symptoms of NAR, the presence of nEo > 20% constantly responding to nasal steroid therapy, is a clear indicator of atopy. In an everyday clinical setting, it emerged as an easy, preliminary, cell biomarker suggestive of further investigation such as NAPT, to discriminate LAR from NARES.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Local allergic rhinitis (LAR) and non-allergic rhinitis with eosinophilia syndrome (NARES) are recently termed entities in the spectrum of non allergic rhinitis (NAR) in childhood [1]. They are characterized by symptoms suggestive of allergic rhinitis, attributed to a localized allergic response in the absence of systemic atopy, assessed by skin prick test or serum specific IgE [2, 3]. The diagnosis of NARES is supported by the detection of nasal eosinophilia and anosmia, whereas the diagnosis of LAR, is evidenced by the detection of local specific IgE or/and by the positivity of nasal allergen provocation test (NAPT) [1,2,3,4,5]. Their recognition in children, even though being of epidemiological importance, are often misdiagnosed and underrated, as they cannot fit into any subgroup of rhinitis by formal criteria. LAR is a common disease that affects children on average 44.5% contrary to NARES, which is estimated to affect less than 2% of children suffering from NAR [1].
NAPT remains the gold standard diagnostic tool for LAR, and the key evidence to define the proper individualized immunotherapeutic strategy [5, 6]. However, besides the high sensitivity and specificity, NAPT exhibits several limitations in clinical practice, principally, the absence of standardized methods and reagents. Reports have suggested a wide diversity of test protocols, allergenic extract, dose, timing, cutoff points and interpretation of the results [7]. Moreover, NAPT is time consuming and requires well-trained personnel, thus is infrequently performed even in adult clinical settings. What is more confusing, is the fact that only few patients, not only with LAR but even with confirmed allergic rhinitis (AR), experience positive NAPT [8, 9]. Thus, cases with increase risk to react in NAPT should be well-collected. On the other hand, the identification of IgE in nasal smear is of limited sensitivity and reports showed a low detection rate in a cohort of LAR patients with positive NAPT [6, 10]. In contrast, nasal eosinophils (nEo) were strongly related to the severity of allergic rhinitis in cases with affirmative NAPT [11]
Moreover, clinical and experimental observations have shown that prior to the detection of specific serum IgE, eosinophils can be found in the nasal smears of atopic children which were strongly correlated with severity, recurrence or prolongation of the disease, and the development of airway hyperreactivity [12,13,14,15]. In addition, in recent nasal biopsies, increased numbers of eosinophil progenitors have been identified, suggesting that eosinophils’ differentiation in situ may contribute to the accumulation of tissue effector eosinophils [16, 17].
Eosinophils in nasal smears are the principal cells involved in the pathogenesis of NAR and AR and also the key inflammatory cells associated with combined allergic respiratory disease, chronic rhinosinusitis with nasal polyps (CRSwNP) or amino salicylic acid sensitivity [18]. In addition, nEo in NARES cases is a risk factor for the development of nasal polyposis and aspirin sensitivity as well as obstructive sleep apnea [19]. CRSwNP is extremely rare in children with few exceptions, such as pediatric patients with cystic fibrosis, allergic fungal sinusitis and aspirin-exacerbated respiratory disease [20].The prevalence of NARES is even lower and less described than CRSwNP contrary to cases with LAR. The clinical presentation suggesting LAR is growing in childhood, yet diagnostic procedure is difficult to perform [21].
Treatment consists mainly of intranasal corticosteroids. Steroids are the key therapeutic agents for eosinophilic diseases. Nasal steroids are mainly used in allergic rhinitis cases with eosinophilic nasal smears which leads to a better control of symptoms [1, 2].
The detection of an easy algorithm customised for children with chronic NAR in every clinical pediatric setting is mandatory. The determination of eosinophils in nasal secretions might be a useful, additional, diagnostic tool. The aim of this study was to evaluate the eosinophils in nasal smear as a preliminary sensitive, easy, rapid and effective test for the differentiation of non-atopic patients with persistent nasal allergic presentation. We hypothesized that the consistent presence of nEo is a valuable easy cell biomarker, strongly recommending the conduction of NAPT for the discrimination of LAR from NARES.
Patients and methods
Study population and definitions
This prospective cross sectional cohort study included novel subjects < 16 years with history of chronic rhinitis, longer than 12 weeks, attending our outpatient Allergy and Pulmonology Unit during the last 5 years (2015–2020). The protocol of this study was approved by the scientific committee of the Hospital and complied with the principles set forth in the Declaration of Helsinki (1964).
The participating patients satisfied three of the following criteria: (a) symptoms of chronic rhinitis (congestion, rhinorrhoea, sneezing, itching) during the last 12 weeks, (b) negative skin prick test (SPT) or specific IgE to any allergen and (c) no use of the following medications: systemic corticosteroid (4 weeks), intranasal corticosteroid (2 weeks), oral antihistamine (1 week), and topical nasal decongestant (1 day), prior to the start of the study.
Patients that had any of the following characteristics were excluded: (a) underlying diseases, including cystic fibrosis, infective chronic rhinosinusitis, immunological diseases or any systemic chronic disease, and (b) a recent history of severe respiratory tract infection within the previous 4 weeks.
Patient baseline characteristics were recorded, including (a) socioeconomic status, family habits and indoor environment and (b) disease characteristics concerning atopy. Rhinitis symptoms were classified according to the Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines. The number of impaired items, including sleep, daily activities, sport, leisure, work, school performance, and troublesome symptoms, was used to categorize rhinitis as mild (no affected items) or moderate-to-severe (at least one affected item). Asthmatic symptoms were recorded and lung function tests for children older than 6 years were performed at baseline and every 6 months throughout the follow-up period.
Skin prick test (SPT)/ sIgE
SPT or/and sIgE were performed using a panel of the most prevalent local aeroallergens, including house dust mites (Dermatophagoides pteronyssinus, Dermatophagoides farinae), molds (Alternaria spp., Cladosporium spp.), American cockroach, cat and dog dander, Cynodon Dactylon, mix grass pollens (Timothy grass, Dactylis glomerata, Festuca elatior Lolium perenne), Parietaria officinalis, Mediterranean cypress and European Olive. Commercial allergens were purchased from ALK Abello (Port Washington, NY, USA). Histamine (10 mg/ml) and saline were used as positive and negative control, respectively. A positive SPT was defined at a wheal diameter of ≥ 3 mm compared to the negative control. Study patients were instructed to discontinue antihistamine and systematic steroids for at least 10 days prior to SPT. SPT were repeated in the 2nd and 4th year of the follow up period. A positive specific IgE was defined, if value was > 0.35 U/L.
Nasal eosinophils
A sterile Rhinoprobe (Arlington Scientific, Springville, UT, USA) was used to collect the nasal mucosa surface samples using the standardized method described by Gelardi et al. [14]. It was inserted into both nostrils along with the tip of the inferior turbinate and the adjacent median nasal wall was under direct visualization, using a headlamp. Nasal cells were collected by a few rotatory movements scraping the middle portion where the ratio ciliate/mucinous cells is expected to be well balanced. When the sampling was obtained, the material was placed on two glass slide, fixed by air drying and stained by May-Grunwald-Giemsa method for 30 min. The slide was then studied through light microscopy supplied with an object-glass, able to magnify up to 1000 × which allows the detection of all the cellular components of the nasal mucosa, including neutrophils and eosinophils. For the rhinocytogram analysis, at least 50 microscopic fields were read. Cell percentages was calculated. nEo > 20% was considered as a positive finding.
Treatment trials
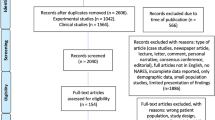
In all cases irrespectively of nasal eosinophils’ percentage, nasal steroids (nasal Fluticasone propionate 1 puff into each nostril twice a day or Mometasone Furoate 1 puff into each nostril per day was recommended for 2 weeks (Fig. 1). The same recommendations and evaluation were repeated, if the nasal symptoms relapsed and nEo was again detected. The success of trials for at least three times was reported as positive. Cases were divided in two groups according to trial responses as follows: non-responding group, if no response was recorded and responding group, if definitely good response to nasal steroids was observed. Ten Visual analogue scale (10-VAS) was used to evaluate symptoms’ score pre and after trial. This scale was used in many clinical trials in children > 6 years with allergy rhinitis and is considered as a sensitive evaluating method [22]. In comparison to pre-treatment values, values less than 5 reported from both parents and children, was considered as a good indicator of a successful response to therapy.
Protocol description. Nasal cytology was tested at baseline to non-atopic children with symptoms suggestive of allergic rhinitis for more than 8 weeks. All cases received nasal steroids for 20 days and were reevaluated using 10-VAS. In cases with relapsing symptoms and nEo, the same therapeutic trial was repeated. During the follow-up period, cases with constantly responded to nasal steroids were considered candidates for proceeding to NAPT to discriminate LAR from NARES. nEo nasal eosinophils, NAPT nasal allergen provocation test, LAR local allergic rhinitis, NARES non allergic rhinitis with eosinophilia syndrome
Statistical analysis
Data analysis was performed using SPSS Statistics for Windows version 23.0 (SPSS, Inc., Chicago IL, USA). Categorical data are presented as number and percentage. Normality of the continuous data was evaluated using Kolmogorov–Smirnov test and Q–Q plots. Description through mean ± standard deviation (SD) for parametric variables and median and interquartile range (IQR) for nonparametric variables was given. Clinical data and eosinophils counts were compared using Mann–Whitney U test or Kruskal Wallis H test. Lineal Logistic regression analysis was used to identify factors significantly associated with nEo, whereas multiple regression analysis was used to evaluate clinical symptoms severity with therapy response. A p value less than 0.05 was considered significant. Specificity and sensitivity of the diagnostic score and a cut-off point were calculated using ROC curve and AUC.
Results
Basic characteristics and nasal eosinophils
One hundred twenty eight (males 63.3%) cases mean aged 72 ± 42 months old with chronic non allergic rhino sinusitis were included in the study and followed up for 52 ± 32 months, during which period all subjects had repeatedly tested negative for systemic atopic. The predominant nasal symptoms were moderate/ severe congestion (64.8%) and rhinorrhoea (70.3%). None of the cases reported anosmia. Seventy-six cases (59.3%) showed substantial amount of nEo > 20%, whereas 52 (40.6%) cases showed no or small numbers of nasal eosinophils (Fig. 1). Moderate-to-severe nasal neutrophilia was found in 50 (39%) cases. nEo was related to reported dyspnoea episodes, OR (95%CI): 2.9 (1.16–7.53) and to nasal neutrophilia (OR (95%CI): 14.5 (5.2–40.9) contrary to nasal clinical symptoms, which showed no association.
Nasal steroids therapy
All cases received nasal steroids for 20 days (Fig. 1). Thirty cases (23.4%) showed no response to therapy. This treatment failure was not related to the presence of neutrophils in nasal smears (OR (95%CI 2.66 (1.04–6.8). Thirty two more cases (25%) responded to therapy once but never again needed any additional treatment during the 5-year follow-up time. Thus, these 62 subjects were considered as not true responders. For the remaining 66 (51.5%) who repeatedly responded to therapy according to 10-VAS, NAR suggestive of LAR or NARES was considered. To confirm the diagnosis, NAPT was recommended.
There were no significant different clinical or environmental characteristics between the two (according to therapy response) groups, as shown in Table 1, except nasal congestion, OR (95%CI): 3.18 (1.49–6.82), and episodes of dyspnoea, OR (95%CI): 3.6 (1.47–8.86). In addition, family history of respiratory allergy was related to therapeutic response. Other atopic diseases or other symptoms, such as rhinohrrea/sneezing or asthmatic cough, did not show any association to therapy success. From the cytology perspective, nEo and nasal neutrophils were significantly correlated to nasal steroids response. Neither serum eosinophils or high IgE nor lung function test showed any correlation.
Multiple regression analysis, used to evaluate all previous results, confirmed that only nEo and nasal congestion were independently strongly correlated with the therapy response (Table 2), whereas the correlation that was found in univariated analysis concerning nasal neutrophils was vanished.
Biomarker—cutoff point
Using ROC curve and AUC, a cutoff point of 20% of nEo was defined as the most reliable biological marker with 94% sensitivity and 77% specificity for evaluating response to nasal steroids therapy (Table 3). In the next step forward analysis, no other clinical or laboratory characteristics, individually or in combinations, were found to have any significance higher than the one that was revealed by the nEo (Table 3, Fig. 2).
Discussion
This study emphasizes the crucial role of eosinophils in nasal mucosa for the diagnosis of NAR based on response to therapy. Patients with non allergic rhinitis are managed using therapeutic measures similar to those adopted in AR [1, 2]. In diseases in which cumbersome or invasive procedures are needed for the diagnosis, a favorable therapeutic response is considered a beneficial tool reflecting the underlying inflammatory mechanism. This has been an accepted trial process in other eosinophils allergy diseases, such as allergic proctocolitis and cough variant asthma [23, 24]. Nasal steroids are the main drug significantly controlling nasal allergic symptoms and, in general, steroids are fundamental in dampening any eosinophilic inflammation [25]. Thus, the main therapy that was evaluated in our study against eosinophils aggregation was the repeated need of nasal steroids in the 5-year follow-up period.
The evaluation of nasal epithelial samples is, nowadays, part of clinical allergy practice based on the evidence that allergic rhinitis inflammation is mainly associated with selective recruitment of eosinophils and basophils in the nasal mucous membrane. Eosinophils can easily be discerned among other mucosal cells, after being stained by May–Grunwald–Giemsa in a simple lab setting.
Eosinophils are not normally sited in nasal mucosa and are extremely rare to be part of the nasal cell diversity. Children with chronic rhinitis have more tissue lymphocytes, macrophages and neutrophils. Malmberg et al. reported that nasal neutrophilia occurred in 47% of students, 79% of school children and 97% of infants [26]. Tissue eosinophilia is uncommon contrary to adults [27]. Ronchetti et al. reported that in their study most of the collected pediatric samples from general population contained no eosinophils and only a few had 1% [28]. The presence of eosinophils in nasal smears is considered as evidence of localized atopy. It has been used as an indicator of allergic rhinitis in cases of atopic asthma strengthening the theory of the united airway disease, while nasal steroids improved clinical symptoms and lung function [29]. However, there are some concerns for pediatric age as common viral infections had temporarily caused accumulation of eosinophils, mainly in cases with atopic background [30]. Besides, there were reports showing the presence of mixed pattern in nasal samples with high neutrophils and eosinophils often accompanied by positive nasal cultures to common microbes such as haemophilus influenza, Moraxella catarrharlis, Streptococcus pneumonia and Staphylococcus aureus. In these cases, infective agents with proteolytic enzymes damaged nasal epithelium tight junctions leading to easily trading of cells and elements, drifting also piles of eosinophils [31, 32]. In addition, in these cases, in contrast to cases with allergic rhinitis, nasal steroids were ineffective and neutrophilia was reported to be an adverse factor non-indicating active nasal allergy [26]. This was also evident in our study, where nasal neutrophils was strongly related to nEo but non-responsive to nasal steroids therapy. Nasal steroids trials were adopted in our study as an additional confirmatory tool. Only clear evidence of a positive outcome abating nasal symptoms in cases with consistent presence of > 20% nEo was considered a strong indicator suggesting non atopic non-infective rhinitis.
There are no definitive quantitative criteria for nasal eosinophilia as a biological allergic marker. Burrows et al. stated that 25% of nEo were a good indicator and Pal et al. reported 100% sensitivity and specificity if nEo increased to more than 30% [33, 34]. Jankowski et al. have set the cutoff point at 20% of cells [35]. Similarly, our study suggested that the detection of > 20% of eosinophils in nasal smears had a high sensitivity and specificity. This is the diagnostic condition for NARES, but it can also be a preliminary indication for LAR [1, 2].
Sensitivity and specificity of the nasal cytology vary in the medical literature even in cases with confirmed allergic rhinitis [36]. The reliability of nasal cytology depends on obtaining adequate specimens, appropriate sample staining and results interpretation. Various techniques such as nasal lavage, mucosal scraping, mucosal imprints or blown secretions have been evaluated as burdensome or impractical to be routinely performed in the clinical setting [37]. Contrary, a suitable biological sample for nasal cytology can be easily collected in pediatric or allergy daily practice using a rhinoprobe. It is non-invasive, simple to perform in office, easy to examine in lab, not time-consuming and inexpensive. The simplicity of a procedure pursuing basic scientific elements increases its sensitivity and specificity [34].
LAR is characterized by an allergen-related nasal hyper-reactivity, despite the absence of specific systemic atopy and NAPT is the absolute gold standard method for the diagnosis and the definition of specific allergic sensitisation. It is performed by administering a set of purified airborne allergens intra-nasally. The positive response to specific allergens such as house dust mite, grass and olive pollen suggesting the presence of LAR [5, 6] was first reported by Huggins et al. in 1975 [38]. NAPT has high sensitivity and specificity when provided with the correct allergens [39]. Nonetheless, NAPT has several limitations in clinical practice, principally the need of multiple tests with different allergens and the absence of standardized methods and reagents [7, 40]. To shorten the procedure, a multiple-NAPT, sequentially using more allergens in a single session, has been proposed in a clinical centre, yet the procedure has not been evaluated by other studies and is not considered suitable for suggesting specific immunotherapy [41]. Apart from that, the diagnostic work-up of NAPT in children is extremely limited. Thus, nEo seems to be a valuable preliminary indicator for worthily selecting cases with increased possibility of a positive reaction in NAPT [39].
An additional method to evaluate LAR is the investigation of local production of IgE. Fuiano et al. were the first to assess specific nasal mucosal IgE in a pediatric population [42]. Marcucci et al. described a novel method to detect nasal IgE in children [43]. However, these methods had limited sensitivity as the detection rate of specific nasal IgE was 35% in a cohort of LAR patients with positive NAPT [10]. Furthermore, studies and current evidences on pediatric LAR cases are still lacking and insufficient to draw any consistent conclusions.
Further diagnostic investigations (e.g., Rhinomanometry, acoustic rhinometry, basophilis activation test), cannot routinely be performed as they lacked to show any acceptable sensitivity or standardization. All techniques for estimating nasal allergy still need to be improved and standardized in children, except nasal cytology, which has been evaluated in a number of studies. The visualization of nasal cytology, as a simple and inexpensive method to investigate children with chronic rhinitis, might allow the description and classification of inflammatory pathology of nasal diseases.
The presence of nEo acts as a characteristic pattern of LAR and NARES that discriminates them from other non-allergic, non-infectious rhinitis endotypes in children, such as idiopathic or vasomotor [1]. From a clinical perspective, nasal congestion in our study was not related to recruitment of eosinophils but was related independently to nasal steroid response and seems to be the main nasal symptom in the therapeutic evaluation. Sympathetic neuromediators, being mainly norepinephrine, cause local vascular constriction, whereas parasympathetic neuropeptides (i.e., acetylcholine) stimulate nasal glands and induce vasodilation and secretions production. Actually, the neural system of the nasal mucosa seems to be part of the underlying mechanisms producing several protective nasal responses against potential stimuli entering the nasal cavities. Thus, patients without nEo that are classified as blockers and respond to nasal steroids might express a different phenotype.
It has been suggested that LAR could overlap with NARES [1, 2].However, more research is needed to further define this entity. Moreover, LAR is a common disease that affects on average 44.5% of children with NAR contrary to NARES, which is estimated to affect less than 2%. Subjects without systemic atopy but with excess nEo and success in nasal steroid therapeutic trials were highly probable to suffer from LAR. On the other hand, NAPES in children was not well described and might be more frequent than expected. Moreover, nEo in NARES cases is a risk factor for the development of nasal polyposis [18, 19]. Thus, nEo could be the preliminary useful biomarker in the diagnostic procedure. LAR, NARES and CRSwNP might represent the different time spectrum of the same disease.
It has also been suggested that LAR could be an allergic rhinitis precursor rather than a distinct phenotype, although this has been contested by more recent findings in agreement with ours. None of the cases during the follow up period showed systemic atopy. It had been shown that the rate of conversion of LAR to “systemic” allergic rhinitis was similar to the percentage observed in a healthy population [44]. These observations seemed to support the concept that LAR and AR seem to be distinct pathological entities.
Limitations
NAPT was not done in our study for the diagnosis of LAR. As the gold standard method for specifying allergy diseases, its correlation with any other method always strengthens the results of any study. However, the inability to perform NAPT not only in children but also in adults due to severe limitations that were discussed in the previous section, minimized the utility of method on a large scale. NAPT results will be presented in a following report. Moreover, eosinophilic inflammation can be unambiguously identified by measuring the eosinophil-specific toxic granules (eosinophil peroxidase (EPO), eosinophil derived neurotoxin (EDN), and eosinophil cationic protein (ECP). However, accurate measurements of eosinophilic granules can be performed using highly equipped lab and ELISA kits. This study major aim was to recommend an easy, non-invasive, inexpensive method using basic medical science that can be applied in a daily clinic as a preliminary diagnostic tool for the evaluation of NAR.
Conclusions
The daily clinical experience comprises children with a clinical history consistent with AR in the absence of any atopic evidence. The diagnostic work-up in these cases is still limited to excluding typical AR. Other methods for a non-invasive and simple evaluation are highly needed, in evidence that NAR diagnosis is growing. Thus, the rising interest on nasal cytology as a possible procedure to define inflammatory response constitutes a clear new indication in children. Taking into consideration the three main points of this study, a diagnostic algorithm can be proposed. In cases with chronic symptoms of non-AR, the presence of nEo > 20% was shown to be a cell preliminary biomarker with high sensitivity and specificity, which mandated the used of nasal steroids as a therapeutic trial. The constantly favourable therapeutic response to steroids strongly suggested the presence of atopy and recommended the conduction of NAPT to discriminate LAR from NARES.
References
Yum HY, Ha EK, Shin YH, Han MY (2021) Prevalence, comorbidities, diagnosis, and treatment of nonallergic rhinitis: real-world comparison with allergic rhinitis. Clin Exp Pediatr 64:373–383. https://doi.org/10.3345/cep.2020.00822
Testera-Montes A, Salas M, Palomares F et al (2021) Local respiratory allergy: from rhinitis phenotype to disease spectrum. Front Immunol 12:691964. https://doi.org/10.3389/fimmu.2021.691964
Rondón C, Campo P, Togias A et al (2012) Local allergic rhinitis: concept, pathophysiology, and management. J Allergy Clin Immunol 129:1460–1467. https://doi.org/10.1016/j.jaci.2012.02.032
Campo P, Rondón C, Gould HJ et al (2015) Local IgE in non-allergic rhinitis. Clin Exp Allergy 45:872–881. https://doi.org/10.1111/cea.12476
Rondón C, Romero JJ, López S et al (2007) Local IgE production and positive nasal provocation test in patients with persistent nonallergic rhinitis. J Allergy Clin Immunol 119:899–905. https://doi.org/10.1016/j.jaci.2007.01.006
López S, Rondón C, Torres MJ et al (2010) Immediate and dual response to nasal challenge with Dermatophagoides pteronyssinus in local allergic rhinitis: immediate and late response to nasal challenge in LAR. Clin Exp Allergy 40:1007–1014. https://doi.org/10.1111/j.1365-2222.2010.03492.x
Klimek L, Hammerbacher AS, Hellings PW et al (2015) The influence of European legislation on the use of diagnostic test allergens for nasal allergen provocation in routine care of patients with allergic rhinitis. Rhin 53:260–269. https://doi.org/10.4193/Rhin14.316
Krajewska-Wojtys A, Jarzab J, Gawlik R, Bozek A (2016) Local allergic rhinitis to pollens is underdiagnosed in young patients. Am J Rhinol Allergy 30:e198–e201. https://doi.org/10.2500/ajra.2016.30.4369
Tantilipikorn P, Siriboonkoom P, Sookrung N, Thianboonsong A, Suwanwech T, Pinkaew B, Asanasaen P (2021) Prevalence of local allergic rhinitis to Dermatophagoides pteronyssinus in chronic rhinitis with negative skin prick test. Asian Pac J Allergy Immunol. https://doi.org/10.12932/AP-170918-0408
Rondón C, Doña I, López S et al (2008) Seasonal idiopathic rhinitis with local inflammatory response and specific IgE in absence of systemic response. Allergy 63:1352–1358. https://doi.org/10.1111/j.1398-9995.2008.01695.x
Park K-I, Jang TY, Yang S-C et al (2018) Correlation of nasal eosinophilia and response after nasal provocation test in patients with nonallergic rhinitis. Otolaryngol Head Neck Surg 159:231–237. https://doi.org/10.1177/0194599818768806
Murayama N, Murayama K (2018) Nasal discharge eosinophils in childhood asthma patients as a predictive factor for persistent asthma. Mediators Inflamm 2018:2563978. https://doi.org/10.1155/2018/2563978
Vinke JG, KleinJan A, Severijnen LWFM et al (1999) Differences in nasal cellular infiltrates between allergic children and age-matched controls. Eur Respir J 13:797. https://doi.org/10.1034/j.1399-3003.1999.13d17.x
Gelardi M, Cavaliere C, Jannuzzi L (2018) Nasal cytology. J Biol Regul Homeost Agents 32:37–40
Hamelmann E, Takeda K, Schwarze J et al (1999) Development of eosinophilic airway inflammation and airway hyperresponsiveness requires interleukin-5 but not immunoglobulin E or B lymphocytes. Am J Respir Cell Mol Biol 21:480–489. https://doi.org/10.1165/ajrcmb.21.4.3659
Cameron L, Christodoulopoulos P, Lavigne F et al (2000) Evidence for local eosinophil differentiation within allergic nasal mucosa: inhibition with soluble IL-5 receptor. J Immunol 164:1538–1545. https://doi.org/10.4049/jimmunol.164.3.1538
Allakhverdi Z, Comeau MR, Smith DE et al (2009) CD34+ hemopoietic progenitor cells are potent effectors of allergic inflammation. J Allergy Clin Immunol 123:472-478.e1. https://doi.org/10.1016/j.jaci.2008.10.022
Barham HP, Osborn JL, Snidvongs K et al (2015) Remodeling changes of the upper airway with chronic rhinosinusitis: remodeling of upper airway in CRS. Int Forum Allergy Rhinol 5:565–572. https://doi.org/10.1002/alr.21546
Ellis AK, Keith PK (2006) Nonallergic rhinitis with eosinophilia syndrome. Curr Allergy Asthma Rep 6:215–220. https://doi.org/10.1007/s11882-006-0037-0
Snidvongs K, Sangubol M, Poachanukoon O (2020) Pediatric versus adult chronic rhinosinusitis. Curr Allergy Asthma Rep 20:29. https://doi.org/10.1007/s11882-020-00924-6
Rondón C, Eguiluz-Gracia I, Campo P (2018) Is the evidence of local allergic rhinitis growing? Curr Opin Allergy Clin Immunol 18:342–349. https://doi.org/10.1097/ACI.0000000000000456
Izquierdo-Dominguez A, Jauregui I, del Cuvillo A et al (2017) Allergy rhinitis: similarities and differences between children and adults. Rhin 55:326–331. https://doi.org/10.4193/Rhin17.074
Mennini M, Fiocchi AG, Cafarotti A et al (2020) Food protein-induced allergic proctocolitis in infants: literature review and proposal of a management protocol. World Allergy Organ J 13:100471. https://doi.org/10.1016/j.waojou.2020.100471
Kim CK, Kim JT, Kang H et al (2003) Sputum eosinophilia in cough-variant asthma as a predictor of the subsequent development of classic asthma: sputum eosinophilia as a predictor of the development of classic asthma. Clin Exp Allergy 33:1409–1414. https://doi.org/10.1046/j.1365-2222.2003.01788.x
Gotlib J (2017) World Health Organization-defined eosinophilic disorders: 2017 update on diagnosis, risk stratification, and management. Am J Hematol 92:1243–1259. https://doi.org/10.1002/ajh.24880
Malmberg H (1979) Symptoms of chronic and allergic rhinitis and occurrence of nasal secretion granulocytes in university students, school children and infants. Allergy 34:389–394. https://doi.org/10.1111/j.1398-9995.1979.tb02008.x
Coffinet L, Chan KH, Abzug MJ et al (2009) Immunopathology of chronic rhinosinusitis in young children. J Pediatr 154:754–758. https://doi.org/10.1016/j.jpeds.2008.11.035
Ronchetti R, Villa MP, Martella S et al (2002) Nasal cellularity in 183 unselected schoolchildren aged 9 to 11 years. Pediatrics 110:1137–1142. https://doi.org/10.1542/peds.110.6.1137
Togias A, Gergen PJ, Hu JW et al (2019) Rhinitis in children and adolescents with asthma: ubiquitous, difficult to control, and associated with asthma outcomes. J Allergy Clin Immunol 143:1003.e10-1011.e10. https://doi.org/10.1016/j.jaci.2018.07.041
Meyer J, Stangenberg S, Weise J et al (2006) Nasal RANTES and eotaxin production pattern in response to rhinovirus infection. Rhinology 44:140–144
McCauley K, Durack J, Valladares R et al (2019) Distinct nasal airway bacterial microbiotas differentially relate to exacerbation in pediatric patients with asthma. J Allergy Clin Immunol 144:1187–1197. https://doi.org/10.1016/j.jaci.2019.05.035
Zhang N, Van Crombruggen K, Gevaert E, Bachert C (2016) Barrier function of the nasal mucosa in health and type-2 biased airway diseases. Allergy 71:295–307. https://doi.org/10.1111/all.12809
Burrows B, Hasan FM, Barbee RA et al (1980) Epidemiologic observations on eosinophilia and its relation to respiratory disorders 1–3. Am Rev Respir Dis 122:709–719. https://doi.org/10.1164/arrd.1980.122.5.709
Pal I, Babu AS, Halder I, Kumar S (2017) Nasal smear eosinophils and allergic rhinitis. Ear Nose Throat J 96:E17–E22. https://doi.org/10.1177/0145561317096010-1105
Jankowski R, Persoons M, Foliguet B et al (2000) Eosinophil count in nasal secretions of subjects with and without nasal symptoms. Rhinology 38:23–32
Miman MC, Uzun O, Gurses I et al (2007) The sensitivity of nasal eosinophilia in allergic rhinitis. Eur Arch Otorhinolaryngol 264:1013–1018. https://doi.org/10.1007/s00405-007-0310-4
Pipkorn U, Karlsson G (1998) Methods for obtaining specimens from the nasal mucosa for morphological and biochemical analysis. Eur Respir J 1:856–862
Huggins KG, Brostoff J (1975) Local production of specific IgE antibodies in allergic-rhinitis patients with negative skin tests. Lancet 306:148–150. https://doi.org/10.1016/S0140-6736(75)90056-2
Jang TY, Kim YH (2015) Nasal provocation test is useful for discriminating allergic, nonallergic, and local allergic rhinitis. Am J Rhinol Allergy 29:e100–e104. https://doi.org/10.2500/ajra.2015.29.4214
Tsilochristou O, Kyriakakou M, Manolaraki I et al (2019) Detection of local allergic rhinitis in children with chronic, difficult-to-treat, non-allergic rhinitis using multiple nasal provocation tests. Pediatr Allergy Immunol 30:296–304. https://doi.org/10.1111/pai.13021
Rondón C, Campo P, Herrera R et al (2011) Nasal allergen provocation test with multiple aeroallergens detects polysensitization in local allergic rhinitis. J Allergy Clin Immunol 128:1192–1197. https://doi.org/10.1016/j.jaci.2011.06.012
Fuiano N, Fusilli S, Incorvaia C (2012) A role for measurement of nasal IgE antibodies in diagnosis of alternaria-induced rhinitis in children. Allergol Immunopathol 40:71–74. https://doi.org/10.1016/j.aller.2011.03.010
Marcucci F, Sensi L (1989) A new method for IgE detection in nasal mucosa. Clin Exp Allergy 19:157–162. https://doi.org/10.1111/j.1365-2222.1989.tb02358.x
Rondon C, Campo P, Eguiluz-Gracia I et al (2018) Local allergic rhinitis is an independent rhinitis phenotype: the results of a 10-year follow-up study. Allergy 73:470–478. https://doi.org/10.1111/all.13272
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Papadopoulou, A., Lambidi, S., Lagousi, T. et al. Nasal eosinophilia as a preliminary discriminative biomarker of non-allergic rhinitis in every day clinical pediatric practice. Eur Arch Otorhinolaryngol 280, 1775–1784 (2023). https://doi.org/10.1007/s00405-022-07704-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07704-0