Abstract
Purpose
Chronic upper airway obstruction caused by adenotonsillar hypertrophy is one of the major cause of morbidity in children. It can lead to Obstructive Sleep Apnoea Syndrome, Pulmonary Hypertension, Cor Pulmonale and right heart failure. The study aimed to evaluate and compare various parameters of cardiac function with the help of echocardiography preoperatively and postoperatively in children undergoing adenotonsillectomy.
Methodology
A prospective cohort study was conducted on 23 patients at an apex care institute, under the age group of 4–12 years, who were diagnosed with adenotonsillar hypertrophy. Preoperative symptom analysis and Echocardiographic examination were done. After the assessment, all patients underwent surgery in the form of adenotonsillectomy. Follow-up symptom analysis and echocardiographic examination was done after 3 months postoperatively.
Results
Significant improvement in the obstructive symptoms were noted in postoperative group as expected (p = < 0.001) and also in parameters such as mPAP (p = < 0.001), TAPSE (p = < 0.001), TAV (p = 0.001), Ejection fraction (p = 0.027) and RVMPI (p = 0.044) were improved in postoperative group. 4 patients had Grade 1 Right ventricular diastolic dysfunction, which disappeared in three patients postoperatively.
Conclusion
We have concluded that there can be subclinical cardiac dysfunctions which occurs as a result of chronic upper airway obstruction due to untreated adenotonsillar hypertrophy. Routine cardiac screening in children presenting with sleep disordered breathing associated with adenotonsillar hypertrophy may be helpful in identifying and preventing the development of cardiopulmonary complication. These changes can be reversed by performing adenotonsillectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
One of the most common causes of upper airway obstruction and morbidity in the paediatric age group is adenotonsillar hypertrophy. Adenoid and tonsils are a group of lymphoid tissues that are part of Waldeyer’s ring. The common cause of hypertrophy of adenoid and tonsils is recurrent episodes of upper airway infection and inflammation. Adenoid hypertrophy can cause nasal obstruction, snoring, mouth breathing during sleep and daytime, daytime hypersomnolence, nocturia, and daytime stertor [1]. The main sequelae faced by children due to upper airway obstruction is “Sleep Disordered Breathing” (SDB). The prevalence of sleep-disordered breathing caused by adenotonsillar hypertrophy varies among different populations. As per studies, prevalence of sleep-disordered breathing in paediatric age group is 1–4% [2]. Sleep-disordered breathing adversely affects children’s cognition, behaviour, growth, and cardiac functions [3]. Untreated adenoid hypertrophy or chronic adenotonsillar hypertrophy causes the narrowing of the upper airway lumen. The patients require more respiratory effort to maintain a sufficient flow of airway through a narrowed lumen. The anatomic obstruction causes cessation of airflow leading to the increase in partial pressure of carbon dioxide (PaCO2) and decrease in partial pressure of oxygen (PaO2) leading to respiratory acidosis. Change in pH causes stimulation of both central and peripheral chemoreceptors leading to arousal from sleep. When these changes happen continuously, because of untreated upper airway obstruction, it may lead to high pulmonary artery pressure due to chronic vasoconstriction. Chronic pulmonary hypertension can cause right ventricular hypertrophy and cor pulmonale [4]. Adenotonsillar hypertrophy is a preventable cause of upper airway obstruction. In the present study, we are using Echocardiography as a tool to diagnose the early changes which can happen in cardiac functions due to chronic upper airway obstruction.
Due to already existing specific guidelines for adenotonsillectomy, most of the patients with adenotonsillar hypertrophy are subjected to conservative management irrespective of their symptoms, which increases the risk for the development of cardiopulmonary diseases in severe cases [5]. This is prevented by early detection of changes in cardiac functions. Doppler Echocardiography is a better, cheap, and cost-effective method to assess different cardiac parameters. Mean Pulmonary Arterial Pressure (mPAP) is one of the most important parameters used to measure pulmonary hypertension. Other parameters used to evaluate right ventricular function includes RVMPI(Right Ventricular Myocardial Performance Index), TAPSE (Tricuspid Annular Plane Systolic Excursion), TAV(Tricuspid Annular Velocity), RVEF(Right Ventricular Ejection Fraction), and Right ventricular diastolic function. One of the unique parameter included in our study is Strain Imaging by Speckle Tracking Echocardiography (STE). As far as our knowledge, this is the first study where strain imaging is used to assess right ventricular function in children with adenotonsillar hypertrophy. The strain of the free wall of the right ventricle is found to be lower in patients with chronic airway obstruction and pulmonary hypertension [6]. So, in the current study, we assessed clinical symptoms and cardiac function in children who required adenotonsillectomy for adenotonsillar hypertrophy using Doppler Echocardiography during the preoperative and postoperative period.
Materials and methods
A prospective cohort study was conducted at an apex care centre in a north-western state of India. Twenty-three consecutive patients of the age group 4–12 years, who were diagnosed with adenotonsillar hypertrophy of grade 3 and 4 with symptom score of more than 6 were included in the study group. The study was conducted in the Department of Otorhinolaryngology in collaboration with the Department of Cardiology from July 2018 to July 2020. Patients with cardiac disease, obesity (BMI > 25 kg/m2), patients with confirmed recurrent tonsillitis or adenotonsillitis (more than seven in a year, more than five for 2 years, more than three for 3 years), any other cause of respiratory obstruction and who had contraindication for general anaesthesia were excluded from the study group. The study protocol fulfilled the ethical consideration and approval was obtained by the Institutional Ethics Committee (IEC).
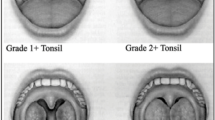
As a part of preoperative evaluation, a detailed clinical, general physical examination, and routine ENT examination were done for all patients. The symptoms score was assessed based on the obstructive symptoms [7]. The size of the tonsil was graded according to Brodsky’s scale [8]. The size of adenoid was assessed by nasal endoscopy. Adenoid grading was done by Cohen and Konak’s method [9]. Patients were asked to score the obstructive symptoms by 0, 1 and 2 suggestive of absent, occasionally, and always, respectively. All patients were given medical management for 3 months and children who did not have any improvement from the medical management were selected for surgery. The total symptoms score was graded as mild, moderate, and severe. Oxygen saturation measurement was done in all patients by pulse oximetry on the day before surgery. After getting fitness for General Anaesthesia, patients were planned for surgery. All patients were admitted 1 or 2 days before surgery and Echocardiography was done preoperatively. Preoperative subclinical cardiac dysfunction was noted and the anaesthetic management of induction and maintenance was done accordingly.
Echocardiography
2-D Doppler Echocardiography was performed in all children both preoperatively and postoperatively using PHILIPS EPIQ 7 Echocardiography machine. Cardiac functions of all patients were evaluated using two-dimensional, M Mode, Doppler echocardiography, and 3D full volume acquisition. Echocardiography was performed with patients lying on the left lateral position, calm and breathing comfortably. mPAP was measured using the formula 90-(0.62xacceleration time) and documented in units of mmHg. TAPSE was measured in millimetres, during systole in the right ventricle through an apical four chamber view. Tricuspid Annular Velocity (cm/sec) was recorded using Tissue Doppler imaging. Myocardial Performance Index was calculated as the sum of isovolumetric contraction time and isovolumetric relaxation time and divided by the ejection time of the corresponding ventricle. Strain imaging of the free wall of the right ventricle was calculated as an average of peak longitudinal strain of basal, mid, and apical segments of the free wall of the right ventricle in RV focused apical four-chamber view. Diastolic functions of both ventricles were determined as the ratio of peak E wave and A wave.
Follow up
Symptom analysis and Echocardiographic analysis were done and compared with the preoperative values at 3 months after the surgery.
Statistical analysis
All collected data were analysed using Statistical Package for Social Sciences (SPSS) version 24.0. (IBM Corp). Qualitative data were expressed in the form of proportion and percentage. Quantitative data were expressed as Mean ± Standard Deviation. Non-parametric data were analysed using the Wilcoxon Signed-Rank test and McNemar test. Quantitative-dependant variables were analysed using the Paired t test. A p value of < 0.05 was taken as significant with a 95% confidence interval.
Results
We enrolled 23 children (20 males and 3 females) in the study group with a mean age of 7.43 ± 2.19 years. We have included patients with moderate and severe symptoms in our study. The mean duration of the presentation of symptoms was 2.22 ± 1.476 years. Grading of adenoid and tonsils was done for all patients by Cohen and Konak Grading system and Brodsky’s scale, respectively. 95.7% of the patient had grade 3 tonsillar enlargement and 4.3% of the patient had grade 4 tonsillar enlargement. 52.2% of the patient had grade 3 adenoid hypertrophy and 47.8% had grade 4 adenoid hypertrophy. All 23 patients had snoring, nasal obstruction, and mouth breathing during sleep with varying severity during the preoperative period. The total symptoms score was moderate in 19 patients (82.6%) and severe in 4 patients (17.4%). There was a significant improvement in obstructive symptoms postoperatively with a p value of < 0.05 (Table1). Only one patient had mild symptoms in the postoperative period.
Echocardiographic parameters were noted (Table 2). mPAP, which is a measure of increased pulmonary artery pressure was 23.713 ± 7.99 mmHg in the preoperative group. After performing surgery, it got improved to a mean level of 16.752 ± 3.070 mmHg (p = < 0.001) (Fig. 1). The preoperative and postoperative value of TAPSE was 18.830 ± 1.775 and 21.622 ± 1.537 mm which shows improvement in right ventricular function (p = < 0.001). Similarly, there was an improvement in RVMPI in the postoperative group (0.3791 ± 0.023) when compared with the preoperative group (0.396 ± 0.034, p = 0.044). RVEF was below 60% in seven patients, although the average ejection fraction was above 60% (61.239 ± 2.420. There was a significant improvement in mean RVEF in the postoperative group (61.239 ± 2.420, p = 0.027). Out of 23 patients, 4 patients had Grade 1 Right Ventricular Diastolic Dysfunction in the preoperative period. Among the four, three patients returned to normal diastolic function after performing the surgery. Right ventricular free wall strain was reduced in the preoperative group (29.696 ± 3.461), which also improved after surgery (31.452 ± 3.477, p = 0.062).
Left ventricular functions were normal in all patients preoperatively. We observed a significant improvement in left ventricular ejection fraction in the postoperative group as compared to the preoperative group.
Discussion
Untreated adenotonsillar hypertrophy with sleep-disordered breathing can lead to subclinical cardiac dysfunction [10]. Long-term obstruction of the upper airway causes chronic hypoxemia and hypercarbia leading to pulmonary vasoconstriction. Chronic pulmonary vasoconstriction can lead to the development of pulmonary hypertension and further right ventricular dysfunction [11]. Tissue Doppler echocardiography is useful in identifying subclinical cardiac abnormalities. Earlier identification can prevent complications.
In the present study, obstructive symptoms were higher in the preoperative group. The symptoms included snoring (100%), mouth breathing during sleep (100%), daytime mouth breathing (95.7%), obstructive breath during sleep (95.7%), nasal obstruction (100%), and daytime hypersomnolence (21.7%). Significant improvement in the symptoms was noted in the postoperative period with almost complete disappearance of all the symptoms. Our findings on preoperative and postoperative symptom scores were consistent with a previous study by Miman et al. on 17 children. The symptom score in our study group decreased from 8.8261 ± 1.557 to 0.0435 ± 0.209. In the Miman et al. study, the change was from 4.88 ± 1.17 to 0.53 ± 0.72[12]. We have obtained a very significant decrease in symptom scores of the patients after adenotonsillectomy. We know that not all children with adenotonsillar hypertrophy develop cardiovascular complications. However, we should anticipate that changes in cardiac function may happen in untreated adenotonsillar hypertrophy. We aimed to identify the subclinical cardiac changes at the earliest by a simple non-invasive technique, to prevent the development of complications.
Elevated mPAP is an indicator of pulmonary hypertension [13]. Pulmonary hypertension is defined as when mPAP is ≥ 25 mmHg [13]. In our study, mPAP in the preoperative and postoperative group was 23.713 ± 7.99 and 16.752 ± 3.070 mmHg, respectively with a p value of < 0.001 which was consistent with another study by S Koc et al. in 2012 (31 ± 9 mmHg; 25 ± 7 mmHg; p = 0.001).
TAPSE is an indicator of the global function of the right ventricle. It describes the axial shortening of the right ventricle during systole [14]. Chronic airway obstruction due to adenotonsillar hypertrophy leads to increased pulmonary vascular resistance. In our study, TAPSE in the preoperative group was 18.830 ± 1.775 mm which was consistent with the study by Lee et al. (19.54 ± 3.32). In their study postoperative TAPSE was 19.88 ± 3.2 which showed no statistically significant difference [15]. Decreased TAPSE is associated with poor prognosis in pulmonary hypertension and cor pulmonale [18]. In the present study, we found improvement in TAPSE after adenotonsillectomy (21.622 ± 1.537; p = < 0.001). Cetin et al. have conducted a study on a greater number of patients (n = 41); where there was a statistically significant difference between preoperative and postoperative group (18.46 ± 1.67 mm and 19.97 ± 1.61; p = 0.000). Thus, more studies on a larger population are required for better results.
Symptoms of increased pulmonary arterial pressure are usually subclinical and their progression into pulmonary hypertension may be slow. But as it progresses it may become severe due to the lack of intervention and it can lead to sudden cardiac decompensation, although these complications occur very rarely in children with adenotonsillar hypertrophy. Adenotonsillectomy, as a surgical intervention, can relieve the upper airway obstruction caused by adenotonsillar hypertrophy.
RVMPI is also an indicator of global right ventricular function, which correlates closely with TAPSE. In our case RVMPI in preoperative and postoperative group was 0.396 ± 0.034 and 0.3791 ± 0.023, respectively (p = 0.044), which shows improvement in ventricular function. Tatlipinar et al. found that RVMPI was on the higher side in the study group with adenotonsillar hypertrophy. They proposed that increase in pulmonary arterial pressure without significant right ventricular dysfunction is the first sign of cardiac complication in children with ATH [16]. Improvement in RVMPI indicates there could have undiagnosed right ventricular dysfunction which got reversed by relieving upper airway obstruction.
RVEF in our study was 61.239 ± 2.420% and 62.626 ± 1.868% in preoperative and postoperative group, respectively (p = 0.027). In the previous studies, LVEF was more studied than RVEF. In a study by Chan et al., RVEF was compared between a normal reference group and children suffering from Obstructive Sleep Apnoea (OSA) due to adenotonsillar hypertrophy [10]. RVEF was lower in OSA group than the control group (51.4 v/s 59.3%; p = 0.001). They proved that cardiac abnormalities improved with effective treatment. In children with persistent OSA, cardiac abnormalities were not reversible. In our study, RVEF was less than 60 percent only in 6 patients, but overall there was an improvement in the ejection fraction of the right ventricle.
Echocardiographic strain imaging is a new method to evaluate contractile functions of heart muscles. Initially, strain imaging was used to evaluate subclinical cardiac dysfunction in diseases like diabetes, cardiomyopathies, systemic sclerosis, and myocardial infarction [17]. But recently, strain imaging is also used to evaluate right ventricle function in pulmonary hypertension which can be seen as a complication of untreated adenotonsillar hypertrophy [6]. In our study, the mean value of the longitudinal free wall shortening of the right ventricle was 29.696 ± 3.461 and 31.452 ± 3.477 in the preoperative and postoperative group, respectively (p = 0.062). The only available literature of the use of strain imaging on children with adenotonsillar hypertrophy is the study done by Kang et al., where they studied the right atrial deformation mechanism [17]. In our study, we assessed RV free wall strain to look for any right ventricular dysfunction which is first in the literature to our best knowledge.
In our study, tricuspid annular velocity (TAV) was 13.87 ± 1.890 cm/sec in the preoperative group and 15.70 ± 1.363 cm/sec, p = 0.001 in the postoperative group. This was in consistent with the study by Koc et al. in 2012, TAV was 17.7 ± 3.6 cm/sec in the preoperative which got improved after adenotonsillectomy (19.1 ± 5.5; p = 0.04)[18]. Although the TAV in preoperative group was not abnormal, but it got significantly improved after surgery. It implies that there may be initial changes in cardiac functions which do not show any clinical impact on the patient. Out of 23 children, 2 patients had mild Tricuspid Regurgitation, which disappeared after the surgery. Thus, we know that early changes in the cardiac functions can be reversed by adenotonsillectomy.
Diastolic functions of the right ventricle were evaluated in our study. Out of 23 children, 4 patients had Grade 1 RVDD (right ventricular diastolic dysfunction) preoperatively. Postoperatively, three patients’ diastolic function became normal and one still had persistent dysfunction. Tezer et al. have got a significant improvement in the diastolic function of the right ventricle postoperatively (p = < 0.001) representing the relationship between adenoid hypertrophy and impaired right ventricular function [19]. As expected, diastolic functions of the left ventricle were normal in both preoperative and postoperative groups which were consistent with previous studies.
Left ventricular functions are also important to evaluate in cases of chronic upper airway obstruction. LVEF was 63.022 ± 1.991% and 64.187 ± 2.321% (p = 0.010) in preoperative and postoperative group, respectively. This was contradictory to the Tal et al. study where there was no significant change in LVEF [20]. However, there was > 10% improvement in some individuals in this study. LVMPI was normal in our study and there was no significant change in the preoperative and postoperative group (p = 0.773). This was compared to a study by Mirecka et al. where left ventricular functions were assessed in children with snoring associated with adenotonsillar hypertrophy [21]. In their study, there was no significant change in both LVMPI and LVEF. In our study, we could find that LVEF improved in the postoperative group compared to the preoperative group. However, it should be kept in mind that ejection fraction calculation is dependent on contractility and loading conditions, which may influence the results on echocardiography examination. Therefore these small changes should not be taken as a significant change.
Limitations
-
Sample size was limited and no control population was taken in the study.
-
No sleep study was done to assess sleep disordered breathing although patients included were having grade 3 and 4 adenotonsillar hypertrophy with obstructive symptom score more than 6.
Conclusion
Long-term upper airway obstruction due to untreated Adenotonsillar hypertrophy may cause cardiovascular changes. Echocardiography which is a simple, cheap and non-invasive modality may be helpful in identifying the earlier cardiovascular changes. Early detection and timely management can prevent development of late sequelae of cardiac complications which is more important in children with known cardiac elements. More studies are required to ascertain the relationship between cardiac changes and adenotonsillar hypertrophy. If a child presents with adenotonsillar hypertrophy causing obstructive sleep symptoms, we recommend sleep study by polysomnography and cardiac screening in the form of echocardiography as a part of preoperative work up.
References
Li H-Y, Lee L-A (2009) Sleep-disordered breathing in children. Chang Gung Med J 32:247–257
Kaditis AG, Alonso Alvarez ML, Boudewyns A et al (2016) Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J 47:69–94
Attia G, Ahmad MA, Saleh AB et al (2010) Impact of obstructive sleep apnea on global myocardial performance in children assessed by tissue Doppler imaging. Pediatr Cardiol 31:1025–1036
Rosenzweig EB, Widlitz AC, Barst RJ (2004) Pulmonary arterial hypertension in children. Pediatr Pulmonol 38:2–22
Barst RJ, Ertel SI, Beghetti M et al (2011) Pulmonary arterial hypertension: a comparison between children and adults. Eur Respir J 37:665–677
Dandel M, Lehmkuhl H, Knosalla C et al (2009) Strain and strain rate imaging by echocardiography—basic concepts and clinical applicability. Curr Cardiol Rev 5:133–148
Chan J, Edman JC, Koltai PJ (2004) Obstructive sleep apnea in children. Am Fam Physician 69:1147–1154
Ng SK, Lee DLY, Li AM et al (2010) Reproducibility of Clinical grading of tonsillar size. Arch Otolaryngol Neck Surg 136:159
Sharifkashani S, Dabirmoghaddam P, Kheirkhah M et al (2015) A new clinical scoring system for adenoid hypertrophy in children. Iran J Otorhinolaryngol 27:55–61
Chan JYS, Li AM, Au C-T et al (2009) Cardiac remodelling and dysfunction in children with obstructive sleep apnoea: a community based study. Thorax 64:233–239
Sevimli S, Gundogdu F, Aksakal E et al (2007) Right ventricular strain and strain rate properties in patients with right ventricular myocardial infarction. Echocardiography 24:732–738
Miman MC, Kirazli T, Ozyurek R (2000) Doppler echocardiography in adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 54:21–26
Çetin M, Yılmaz M, Özen S et al (2014) Assessment of pulmonary artery pressure and right ventricular function in children with adenotonsillar hypertrophy using different parameters. Int J Pediatr Otorhinolaryngol 78:1837–1842
Kjaergaard J, Akkan D, Iversen KK et al (2007) Right ventricular dysfunction as an independent predictor of short- and long-term mortality in patients with heart failure. Eur J Heart Fail 9:610–616
Lee JH, Yoon JM, Lim JW et al (2014) Effect of adenotonsillar hypertrophy on right ventricle function in children. Korean J Pediatr 57:484
Tatlipinar A, Duman D, Uslu C et al (2011) The effects of obstructive sleep apnea syndrome due to adenotonsillar hypertrophy on the cardiovascular system in children. Turk J Pediatr 53:359–363
Kang SJ, Kwon YW (2018) Right atrial deformation mechanics in children with adenotonsillar hypertrophy. J Cardiovasc Imaging 26:201
Koc S, Aytekin M, Kalay N et al (2012) The effect of adenotonsillectomy on right ventricle function and pulmonary artery pressure in children with adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol 76:45–48
Tezer MS, Karanfil A, Aktaş D (2005) Association between adenoidal–nasopharyngeal ratio and right ventricular diastolic functions in children with adenoid hypertrophy causing upper airway obstruction. Int J Pediatr Otorhinolaryngol 69:1169–1173
Tal A, Leiberman A, Margulis G et al (1988) Ventricular dysfunction in children with obstructive sleep apnea: radionuclide assessment. Pediatr Pulmonol 4:139–143
Mirecka J, Mazurek-Kula A, Ostrowska K et al (2019) Left heart ventricle function in children snoring due to adeno-tonsillar hypertrophy. Pediatr Pol 94:13–17
Acknowledgements
We thank Dr. Prem Prakash Sharma (Associate Professor, Department of Community Medicine and Family Medicine) for his tremendous help in statistical analysis of the data.
Funding
No funding was received to conduct this study or with the preparation of manuscript.
Author information
Authors and Affiliations
Contributions
All authors certify that they have no affiliations or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
Ethical approval for this study was obtained from Institutional Ethical Committee, AIIMS Jodhpur vide their letter number No. AIIMS/IEC/2018/1440. There was no extra financial burden for the patients in relation to study.
Consent to participate
All parents of the patients were informed about the purpose of the study before enrolling. Informed written consent was taken from parents or caretakers of all the children included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sameema, V.V., Soni, K., Deora, S. et al. Assessment of preoperative and postoperative cardiac function in children with adenotonsillar hypertrophy: a prospective cohort study. Eur Arch Otorhinolaryngol 279, 3013–3019 (2022). https://doi.org/10.1007/s00405-022-07255-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07255-4