Abstract
Objective
This study aimed to analyze the role of the endoscope in revision canal-wall down (CWD) tympanomastoid surgery and compare its use to the more traditional microscopic approach. Moreover, we aim to investigate functional outcomes of revision surgeries in a cohort of two tertiary reference centers.
Methods
A total of 103 patients undergoing revision surgery after previous CWD tympanomastoidectomy were included in the present study and divided in three groups according to the surgical technique used: endoscope exclusive (n = 22), combined (n = 35) and microscope exclusive (n = 46). Data regarding surgical indications, pre-operative clinical and audiological assessments, intraoperative findings and surgical considerations were extracted. During follow-up, data regarding anatomic and audiologic outcomes were collected and persistence or recurrence of the disease assessed.
Results
The most frequent sites of cholesteatoma recurrence or persistence was the anterior epitympanum. There was a statistically significant ABG improvement of − 6.02 dB HL (95% CI − 8.87 to − 3.16, p < 0.001) between pre-operative and postoperative ABG, without significant effect of surgical technique. During follow-up, no significant differences regarding disease or otorrhea control were observed. Duration of surgery and hospitalization was shorter in the endoscopic cohort without statistical significance. Intra- and postoperative complications were lower in the endoscopic group.
Conclusion
Revision CWD surgery can take advantage of the endoscope as a minimally invasive exclusive or adjunct tool to traditional microscopic procedures. Outcome measures of endoscopic revision CWD surgery showed anatomic and functional results comparable to those of the microscopic group. The complication rate, the duration of surgery and hospitalization were favorable in the endoscopic group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Canal-wall down (CWD) tympanomastoidectomy is a common and well-established technique used for the surgical treatment of chronic otitis media, especially regarding cholesteatoma eradication. The main advantage associated with this procedure is the wide exposure of the middle ear by creating an open mastoid cavity for improved postoperative monitoring [1]. Contrarily, the canal-wall up (CWU) technique preserves the integrity of the external auditory canal (EAC) and the creation of a mastoid bowl is avoided. However, CWU is characterized by high recidivism rates ranging between 16.7 and 61% in children and up to 20% in adults, which is probably due to the poor exposure of the middle ear and antrum during surgery. In contrast, low rates of recidivism were reported from 0 to 13.2% for the CWD technique [2, 3].
However, CWD tympanomastoidectomy has several well-known drawbacks, such as cosmetic concerns regarding the enlarged meatus, water intolerance, calorically induced vertigo and intermittent ear discharge, which have an impact on the quality of life of the patients [1, 4]. In particular, recurrent otorrhea requires periodic consultations for aural toilet and prescription of topical and/or systemic antibiotics. Moreover, recurrent and residual cholesteatoma might develop even after CWD tympanoplasties. These situations require revision surgery to restore a safe, dry and disease-free ear. Similarly, as reported for CWU tympanoplasties, there is a consistent amount of recurrent and or persistent cholesteatomas associated within the hidden areas of the middle ear, such as the retrotympanum and the anterior epitympanic space [5, 6].
In this context, the endoscope may be useful to control and eradicate the disease from these regions deemed difficult to access. The enhanced view of the surgical field and the capability to look and work around the corner are the most appreciated advantages of endoscopic ear surgery (EES) [5, 6]. However, the use of endoscopes in cases of revision surgery after CWD procedures has not been investigated so far. This study aimed to analyze the role of the endoscope in revision CWD tympanomastoid surgery and compare its use to the microscopic approach. Moreover, we aim to investigate functional outcomes of revision surgeries in a cohort of two tertiary reference centers.
Materials and methods
Ethical considerations
The institutional review board (Kantonale Ethikkomission Bern) granted approval to perform the present study (KEK-BE Nr. 2019-00555). The institutional review board of Modena University hospital granted exemption from formal ethical approval, as it is not required for retrospective studies. This study was performed according to the Declaration of Helsinki.
Patients
All patients undergoing revision surgery after previous CWD tympanomastoidectomy were included in the present study and divided in three groups according to the surgical technique used during revision surgery: (1) endoscope exclusive, (2) combined and (3) microscope exclusive. Data regarding previous surgeries, surgical indications, pre-operative clinical and audiological assessments, intraoperative findings and surgical considerations were extracted. During follow-up, data regarding anatomic and audiologic outcomes were collected and persistence or recurrence of cholesteatoma assessed. The role of the endoscope was quantified by the classification by Cohen et al. [7] as follows: class 0: microscope only; class 1 endoscope for inspection only; class 2a < 50% endoscopic dissection and 2b > 50% endoscopic dissection and class 3 exclusive endoscopic technique. The choice of the surgical technique was at the discretion of the operating surgeon.
Statistical analysis
Patient demographics, perioperative factors, intraoperative and postoperative variables were summarized using descriptive statistics. To compare the effects of surgical technique on the ABG improvement, we conducted a mixed 3 × 2 Anova with surgical technique as a between and measurement point as a within factor. To compare the effects of surgical technique on surgery duration, a one-way ANOVA was conducted with surgical technique as a between factor and surgery duration as the dependent variable. Normality checks and Levene’s test were carried out and the assumptions met.
To observe the effect of the surgical technique on the disease persistence and recurrence after revision surgery, we calculated odds ratio with endoscope as the reference group. We added 0.5 to each observed frequency in a table where a zero observed frequency occurred. Confidence intervals are provided as well as effect sizes in terms of generalized eta squared, whereas 0.02 is considered a small, 0.13 a medium and 0.26 a large effect [8]. Statistical analyses were conducted in R, version 3.6.2 (R Project for Statistical Computing).
Results
A total of 103 patients were included in the present study and analyzed. All patients underwent previous CWD surgery (CWD: 38.80%, obliterated CWD: 16.50% and radical mastoidectomy: 44.70%). None of the patients underwent modified Bondy’s technique. Depending on surgical technique during revision surgery, the cohort was divided in 3 groups: exclusive endoscopic revision surgery (n = 22), combined endoscopic and microscopic (n = 35) and exclusive microscopic (n = 46) technique. Preoperative patient characteristics are summarized in Table 1. The only significant differences observed among the groups were the pre-operative otorrhea rate (χ2(4, N = 103) = 18.909, p = 0.001) and indications for revision surgery (χ2(6, N = 103) = 27.062, p < 0.001).
Revision surgery was planned according to the preference of the operating surgeon(s). Details of the surgical procedures are summarized in Table 2. Persistent or recurrent cholesteatoma was intraoperatively observed in n = 80 patients or 77.67% of the cases.
The localization of cholesteatoma during revision surgery is illustrated in Fig. 1.
These patients were treated with either endoscopic exclusive approach (n = 19/22, 86.4%), combined approach (n = 32/35, 91.4%) or microscopic exclusive approach (n = 29/46, 63.0%), depending on cholesteatoma extension and presence of complications (Table 2).
Complications during revision surgery (intraoperative) and up to 30 days following surgery (postoperative infection, wound problems and vertigo) were observed in n = 31 patients (30.1%). The distribution of complications per technique is illustrated in Fig. 2. Depending on the intraoperative findings the surgical plan was adapted from an exclusively endoscopic to a combined approach in 21 cases. The reasons therefore were extension of cholesteatoma (n = 18), infiltration of dura (n = 1), CSF leak (n = 2).
After a mean follow-up of 31.1 months, the outcome of revision surgeries per last follow-up is summarized in Table 3. The audiometric data were available only for n = 88 patients (n = 20 endoscope exclusive, n = 31 combined and n = 37 microscope exclusive).
Comparative statistical analysis
There was a statistically significant ABG improvement [F(1,85) = 15.67, p < 0.001, η2G = 0.06] with a mean difference of − 6.02 dB HL (95% CI − 8.87 to − 3.16) between pre-operative and postoperative ABG. There was no statistically significant effect of surgical technique on the ABG gain [F(2,85) = 1.78, p = 0.206, η2G = 0.03], nor was there a statistically significant interaction [F(2,85) = 0.05, p = 0.95, η2G < 0.01].
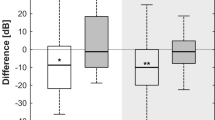
The effect of surgical technique on surgery duration reached statistical significance [F(2,100) = 9.05, p < 0.001, η2G = 0.15]. Post hoc comparisons showed that surgeries lasted longer with combined techniques than with endoscopic technique (mean difference: 61.16 min, 95% CI 26.26–96.07) and with microscopic technique (mean difference: 32.70 min, 95% CI 3.91–61.46). However, the mean difference between endoscopic and microscopic techniques did not reach statistical significance (mean difference: 28.47 min, 95% CI − 4.79 to 61.73). The surgery duration among the three techniques is illustrated in Fig. 3. No statistically significant differences among the techniques were found in terms of residual or recurrent cholesteatoma during the follow-up period.
Surgery duration in minutes compared for endoscopic, microscopic and combined procedures. The lower and upper hinges correspond to the first and third quartiles (the 25th and 75th percentiles). The thick horizontal line represents the median, the diamond the mean. The upper and lower whiskers extend from the hinge to the largest and smallest value, respectively, no further than 1.5 * IQR (inter quartile range) from the hinge. Data beyond the end of the whiskers are outliers. * < 0.05 ** < 0.001
Discussion
This comparative, multi-centric study on revision surgery after CWD tympanoplasties shows the outcomes of three different approaches. In particular, this case series represents the first experience of endoscope use for revision CWD surgery. The results indicate that an endoscopic transcanal approach might be a viable option in selected cases. Comparable postoperative functional outcomes and disease-control rates were obtained among the three different subgroups. The endoscopic technique appears suitable regarding residual or recurrent disease in the middle ear, especially the retrotympanum and anterior epitympanum. However, large disease extensions posteriorly, as well as infiltrations of the lateral skull base or mastoid obliteration procedures require the use of the microscopic approach. This is exemplarily illustrated by the n = 21 conversions from exclusive endoscopic to a combined approach.
Forty-six patients (44.6%) underwent exclusive microscopic revision surgery, 22 (21.4%) underwent exclusive endoscopic revision surgery and the remaining 35 (34%) cases underwent a combined approach. In this latter subgroup, the endoscope was mostly used for inspection only, while in 25.7%, it was used for less than 50% of dissection (Cohen’s Class 2A) and the remaining 11.4% of the patients had more than 50% of dissection performed endoscopically (Cohen’s Class 2B) [7]. These observations highlight the versatility of the endoscope in this surgical setting ranging from exclusive surgical technique to a simple adjunct to visualize hidden areas, which cannot be explored under microscopic view, notably despite a large CWD cavity. Moreover, the role of the microscope in CWD revision surgery is illustrated in the present cohort regarding the relatively frequent occurrence of extensive recurrent or persistent cholesteatomas or complications thereof (i.e. lateral semicircular canal fistula, dural infiltration, etc.).
The goals of cholesteatoma surgery are (1) complete eradication of the disease, (2) preventing recurrence, and (3) maintaining or restoring hearing. CWD tympanomastoidectomy is one of the techniques used for this purpose and a successful CWD procedure should result in a dry postoperative cavity [9]. The removal of the posterior EAC allows better disease visualization and therefore disease-control resulting in lower rates of recurrence, which is reported between 0 and 15% compared to CWU procedures [2, 3, 10]. However, our results suggest a not-negligible prevalence of recurrent/residual cholesteatoma in difficult to access areas, such as the anterior epitympanum and retrotympanum (Fig. 1). Similar observations were reported by Das et al. who described the sinus tympani as the commonest site of recurrence [11]. Pareschi et al. reported in their CWD case series of 895 patients, that the 86.6% of residual cholesteatomas were located in the retrotympanum [10]. These anatomic subsites have been also classified as “difficult areas” for microscope-based surgeries in several cholesteatoma staging classifications [12, 13]. In this context and as reported herein, the endoscope’s capability to look around corners is helpful in the assessment of these areas and in the detection of possible residual disease [14]. In this study, the reported residual cholesteatoma rate was 0% (mean follow-up: 28.1 months) for the endoscope exclusive group and 10.9% (mean follow-up: 29 months) for the microscope exclusive technique. However, this difference did not reach statistical significance (p = 0.09), probably due to the limited number of patients in this cohort.
Consistently higher rates of pre-operative intermittent and continuous othorrea were found amongst the microscopic exclusive and combined subgroups. This finding may be explained by the relationship among local inflammation and intraoperative bleeding, which is one the major drawbacks of exclusive endoscopic ear surgery [15, 16]. Moreover, the indication for mastoid obliteration to treat chronic otorrhea (e.g. without presence of recurrent or residual cholesteatoma) would not be suitable for the endoscopic approach.
A shorter duration of surgical procedures was reported for patients undergoing the exclusive endoscopic group (Table 2). Interestingly, the group of patients who underwent a combined (endoscopic– microscopic) procedure had a statistically significant longer surgical time with respect to the other two groups. This could be explained by the time needed to switch amongst two different surgical equipment and to the extension of disease requiring the combination of both surgical techniques.
Several authors reported that revision CWD surgery is potentially more challenging since most of anatomic landmarks are lacking [10, 11]. However, a relatively low rate of complications is observed in the presented case series of exclusive endoscopic revision CWD procedures, both intraoperatively and postoperatively [17]. Thus, the endoscopic technique might also have a role in preventing complications related to CWD revision procedures due to its refined capability to identify the remaining anatomic landmarks in a post-surgical cavity. When compared to the other two groups, the complication rate is lower (Fig. 2). However, the cases treated by an exclusive endoscopic approach were less extensive, than in the other groups. Moreover, complications have not consistently been found to be different for microscopic versus endoscopic approaches in the literature, including dizziness, dysgeusia, and facial paralysis [18]. Concerning the postoperative functional outcomes, we found a statistically significant ABG improvement, but no significant effect of surgical technique on the ABG gain. The pre-operative and postoperative BC thresholds were comparable among the three different techniques, demonstrating that no major cochlear function damage occurred [19].
The role of the endoscope in revision CWD surgeries should be tailored on a case-by-case basis to allow most favorable results for the patient. The anterior epitympanic space is best reached with the endoscope, especially when a deep suprageniculate pneumatization is encountered. Likewise, the sinus tympani is better examined with angled endoscopes, even in an open mastoid cavity, as already stated by several other authors [10, 11, 14]. However, limitations of the exclusive endoscopic approach should be considered. Dural infiltration by cholesteatoma, large or posteriorly placed lateral semicircular canal fistulas and residual disease in an obliterated cavity cannot be managed with an exclusive endoscopic approach. Similarly, cholesteatomatous extension toward the petrous bone apex should be primarily managed microscopically (Table 4).
This study has limitations related to the retrospective nature of the study and additionally: (1) despite being multi-centric, the number of included patients is limited, possibly affecting the power of the statistical analyses; (2) the surgical technique was chosen by the operating surgeon; therefore, a selection bias related to the disease’s extension and location should be considered in the interpretation of the results; (3) the mean follow-up duration of the endoscope exclusive group was shorter than in the other two groups and (4) the anatomic and audiologic outcomes evaluations were performed at variable time points. To address these issues, future investigations using a prospective study design would be suitable.
Conclusion
Revision tympanomastoidectomy after CWD surgery can take advantage of the endoscopic technique revealing satisfactory results regarding anatomical and functional outcomes. The endoscope may be employed exclusively or in combination with the microscopic technique, depending on the indication for revision surgery and the extension of disease. Especially regarding persistent or recurrent disease in the anterior epitympanum or retrotympanum, the endoscope appears advantageous. However, in extensive disease including infiltration of the lateral skull base, the microscope was predominantly used.
Availability of data and material
All relevant data and the final dataset are available upon motivated request to the corresponding author.
References
Kasenõmm P (2013) Intraoperative findings of revision canal wall-down tympanomastoid surgery. ActaOtolaryngol 133(8):826–832. https://doi.org/10.3109/00016489.2013.787645
Kerckhoffs KGP, Kommer MBJ, van Strien THL et al (2016) The disease recurrence rate after the canal wall up or canal wall down technique in adults: a review on cholesteatoma recidivism after CWU and CWD. Laryngoscope 126(4):980–987. https://doi.org/10.1002/lary.25591
Walker PC, Mowry SE, Hansen MR, Gantz BJ (2014) Long-term results of canal wall reconstruction tympanomastoidectomy. OtolNeurotol 35(6):954–960. https://doi.org/10.1097/MAO.0b013e3182a446da
Lucidi D, De Corso E, Paludetti G, Sergi B (2019) Quality of life and functional results in canal wall down vs canal wall up mastoidectomy. ActaOtorhinolaryngol Ital 39(1):53–60. https://doi.org/10.14639/0392-100X-2005
Alicandri-Ciufelli M, Fermi M, Bonali M et al (2018) Facial sinus endoscopic evaluation, radiologic assessment, and classification: facial sinus endoscopic study. Laryngoscope 128(10):2397–2402. https://doi.org/10.1002/lary.27135
Anschuetz L, Alicandri-Ciufelli M, Bonali M et al (2018) Novel surgical and radiologic classification of the subtympanic sinus: implications for endoscopic ear surgery. Otolaryngol-Head Neck Surg 159(6):1037–1042. https://doi.org/10.1177/0194599818787180
Cohen MS, Basonbul RA, Barber SR, Kozin ED, Rivas AC, Lee DJ (2018) Development and validation of an endoscopic ear surgery classification system: endoscopic ear surgery classification system. Laryngoscope 128(4):967–970. https://doi.org/10.1002/lary.26802
Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences. 2nd ed. L. Erlbaum Associates
Košec A, Kelava I, Ajduk J, Ries M, Trotić R, Bedeković V (2017) Significance of intraoperative findings in revision tympanomastoidectomy. Am J Otolaryngol 38(4):462–465. https://doi.org/10.1016/j.amjoto.2017.04.006
Pareschi R, Lepera D, Nucci R (2019) Canal wall down approach for tympano-mastoid cholesteatoma: long-term results and prognostic factors. ActaOtorhinolaryngol Ital 39(2):122–129. https://doi.org/10.14639/0392-100X-2237
Das S, Dutta M, Panja T, Sinha R (2019) Chronic draining ear and cholesteatoma recidivism: a retrospection from clinical, imaging, and surgical perspectives. Turk Arch Otorhinolaryngol 57(3):133–139. https://doi.org/10.5152/tao.2019.4266
Yung M, Tono T, Olszewska E et al (2017) EAONO/JOS joint consensus statements on the definitions, classification and staging of middle ear cholesteatoma. J IntAdvOtol 13(1):1–8. https://doi.org/10.5152/iao.2017.3363
van der Toom H, van der Schroeff M, Janssen J, Westzaan A, Pauw R (2020) A retrospective analysis and comparison of the STAM and STAMCO Classification and EAONO/JOS cholesteatoma staging system in predicting surgical treatment outcomes of middle ear cholesteatoma. OtolNeurotol 41(4):e468–e474. https://doi.org/10.1097/MAO.0000000000002549
Bonali M, Fermi M, Alicandri-Ciufelli M et al (2020) Correlation of radiologic versus endoscopic visualization of the middle ear: implications for endoscopic ear surgery. OtolNeurotol 41(9):e1122–e1127. https://doi.org/10.1097/MAO.0000000000002787
Anschuetz L, Bonali M, Guarino P, et al (2018) Management of bleeding in exclusive endoscopic ear surgery: pilot clinical experience. Otolaryngol-Head Neck Surg. Published online September 5, 2017:019459981772698. https://doi.org/10.1177/0194599817726982
Ferri G, Fermi M, Alicandri-Ciufelli M, Villari D, Presutti L (2019) Management of jugular bulb injuries during endoscopic ear surgery: our experience. J Neurol Surg Part B Skull Base. Published online January 21, 2019. https://doi.org/10.1055/s-0039-1677679
Marchioni D, Rubini A, Gazzini L et al (2018) Complications in endoscopic ear surgery. OtolNeurotol 39(8):1012–1017. https://doi.org/10.1097/MAO.0000000000001933
Chiao W, Chieffe D, Fina M (2021) Endoscopic management of primary acquired cholesteatoma. OtolaryngolClin North Am 54(1):129–145. https://doi.org/10.1016/j.otc.2020.09.014
Botti C, Fermi M, Amorosa L, et al (2019) Cochlear function after type-1 tympanoplasty: endoscopic versus microscopic approach, a comparative study. Eur Arch Oto-Rhino-Laryngol. Published online October 25, 2019. https://doi.org/10.1007/s00405-019-05706-z
Funding
No funding is reported for the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fermi, M., Siggemann, T., Melchiorri, C. et al. Revision canal-wall down surgery: comparison of surgical outcomes with three different techniques. Eur Arch Otorhinolaryngol 279, 1731–1739 (2022). https://doi.org/10.1007/s00405-021-06829-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06829-y