Abstract
Purpose
Laser transoral laryngeal microsurgery has become widely accepted treatment method because of its organ and function preservation and shorter period of hospitalization. The aim of this study was to examine the overall, disease-specific and disease-free survival in patients with early laryngeal carcinoma treated with laser depending on age, gender, common risk factors (tobacco and alcohol use), histopathological tumor grade, anterior commissure involvement, performed tracheotomy, positive surgical margins, T stage, type of endoscopic cordectomy, postoperative radiotherapy and laryngeal preservation.
Methods
Retrospective study included 234 patients with squamocellular carcinoma of the larynx treated with laser transoral laryngeal microsurgery. 5-year overall, disease-specific and disease-free survival and the prognostic impact of mentioned factors were evaluated using Kaplan–Meier and Cox proportional hazard analyses.
Results
5-year OS and DSS was 92.5% and 95.3%, respectively. OS was significantly lower for older patients and in patients with histologically poorly differentiated tumors, 3 and 5 years postoperatively (Log rank test; p = 0.031). DSS was significantly lower in patients with anterior commissure involvement, positive surgical margins and patients who underwent postoperative RT. DFS was significantly lower in patients with anterior commissure involvement, patients with T1b tumor stage and patients who underwent cordectomies type Vb and VI (Log rank, p < 0.05). Laryngeal preservation significantly influenced 5-year OS, DSS and DFS (Log rank, p ≤ 0.001). Multivariate Cox regression analysis showed that age, histological tumor grade and laryngeal preservation were significant negative prognostic factors for 5-year DSS and DFS.
Conclusion
Transoral laryngeal microsurgery delivers excellent oncological results, even in selected patients with higher stages of early laryngeal cancer and anterior commissure involvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laryngeal cancer is the most common head and neck carcinoma with over 150,000 primary diagnosed patients each year [1]. Early stages of laryngeal carcinoma can be successfully treated with transoral laryngeal microsurgery (TLM) with cold steel or laser resection, radiotherapy (RT) or open surgery. When laser TLM was presented, it involved many controversies considering satisfactory oncological results, clean surgical margins and anatomical limitations. Today, it has become widely accepted treatment method because its organ and function preservation, fast recovery of swallowing function, lower incidences of aspiration and shorter period of hospitalization [2].
Using the European Laryngological Society (ELS) classification of endoscopic cordectomies for treatment of glottic carcinoma [3, 4], surgical techniques were more uniform, and postoperative oncological and functional results were more comparable. Even in the cases of local recurrences, post TLM treatment has been well documented, and it includes open conservation or radical surgery, radiotherapy or chemoradiotherapy [5, 6].
The aim of this study was to investigate oncological results of the patients with early laryngeal carcinoma treated with laser TLM. Overall, disease-specific and disease-free survival was determined depending on age, gender, common risk factors (tobacco and alcohol use), histopathological tumor grade, anterior commissure involvement, performed tracheotomy, positive surgical margins, T stage, type of endoscopic cordectomy, postoperative radiotherapy and laryngeal preservation.
Materials and methods
A retrospective study was conducted on 234 patients treated at the Clinic for Otorhinolaryngology and Maxillofacial Surgery, Clinical Center of Serbia in Belgrade. The data were obtained by processing medical charts of the patients with squamocellular carcinoma of the larynx treated with laser TLM in the period from April 1st, 2006 to March 31st, 2013. This study was approved by the Institutional Ethical Committee (440/IX-3/09), and all patients signed the informed consent form prior to their inclusion in the study. Patients were divided into age groups according to International Cancer Survival Standard (ICSS) using the Five Default Age Groups (15–44, 45–54, 55–64, 65–74, 75+) [7].
The diagnosis of laryngeal carcinoma was confirmed by otorhinolaryngological clinical examination and laryngomicroscopic examination of the larynx with the biopsy and histopathologic examination of the tissue. Additional diagnostics, such as ultrasonography of the neck and of the abdomen, chest X-ray and computed (CT) tomography of the neck, were performed to determine the TNM stage of the disease [8]. Study included patients diagnosed with early laryngeal carcinoma (T1 and T2N0M0), without previous treated laryngeal malignancies and distant metastases.
The modality of treatment for every patient was decided on the multidisciplinary oncological board. Laser TLM was conducted in general endotracheal anesthesia, with a Sharplan Lumenis 40C CO2 laser in Acublade mode with 10–12 W (Lumenis Ltd. London, UK), under Carl Zeiss Surgical OPMI Sensera optical microscope (Carl Zeiss Meditec Inc. Dublin, CA). Endoscopic resections were done by three different surgeons, in “en-bloc” or “piece-meal” technique according to the extension and exposure of the tumor. Classification of endoscopic cordectomies was done according European Laryngological Society (ELS) [3, 4]. If there was a heighten risk from endolaryngeal oedema or bleeding, temporary tracheostomy was done. Tracheostomy was closed at the end of hospital stay in all cases.
Surgical margins were assessed positive if there was tumor tissue on the inked margin or on less than 1 mm away from the margin and negative if the inked margin was free of the tumor tissue. Most of the patients with positive surgical margins underwent revision surgery. In little number of cases with positive surgical margins, radiotherapy (RT) was conducted and it consisted of external radiotherapy with total dose of 60 to 65 Gy in 30–35 fractions for 6–7 weeks. Patients underwent open surgery, partial laryngectomy or total laryngectomy in cases of local recurrence, because of the localization and the extent of the recurrent disease. Follow-up period was from 62 to 79 months. Demographic characteristics (age and gender) and risk factors (cigarette and alcohol consumption) were noted. Histopathological tumor grade, anterior commissure involvement, performed tracheotomy, positive surgical margins, T stage, type of endoscopic cordectomy and laryngeal preservation after follow-up period were also examined. 5-year overall, disease-specific and disease-free survival of patients was determined depending on all previously mentioned factors.
Program SPSS v20 (Statistical Package for Social Sciences, SPSS Inc, Chicago, Illinois) was used for statistical analysis. Descriptive statistics were calculated for demographic characteristics, risk factors and other followed parameters and are presented as frequencies and proportions. Overall survival (OS), disease-specific survival (DSS) and disease-free survival (DFS) rates were calculated using the Kaplan–Meier method. A Cox proportional hazards regression model was used for univariate and multivariable was used to evaluate the impact of prognostic factors on disease-specific and disease-free survival. Risk estimates are presented as hazard ratios (HR) with 95% confidence intervals (CI). Statistical significance was considered at p < 0.05.
Results
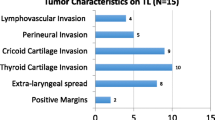
Most of the patients included in the study were males (93.6%), smokers (88.5%) and alcohol non-consumers (73.9%) (Table 1). Average age of the patients was 60.22 (SD ± 8.99). The oldest patient was 82, and the youngest 37 years old. After histopathological analysis, most of the tumors were moderately differentiated (62.8%). Considering T stage of the disease, T2 stage was most frequent (47.5%), followed by T1a stage (43.2%). Patients with T2 stage were divided into two groups, patients with tumor extension to supraglottis and/or subglottis without impaired vocal cord mobility (94 patients, 40.2%) and with impaired vocal fold mobility (17 patients, 7.3%) because of the further analysis of survival results. Patients underwent all types of endoscopic cordectomies, except type I cordectomy, according to ELS classification. Intraoperative tracheotomy was performed in 12 (5.1%) of the patients. 52 patients (22.2%) had positive tumor resection lines. 29 of then underwent revision surgery and 23 underwent postoperative RT. Local recurrence rate was 12%, mostly in the T2 group (17 patients) and T1a (7 patients). Laryngeal preservation was achieved in 94%. Laryngeal preservation for different T stages of the patients included in the study was shown in Fig. 1. Lower rates were found in patients with T1b tumors ant T2 tumors with impaired vocal fold mobility.
For patients included in the study, 3-year and 5-year OS was 97% and 92.5%, respectively; and 3-year and 5-year DSS was 97.4% and 95.3%, respectively. OS was significantly lower for older patients, 3 and 5 years postoperatively (Log rank test; p = 0.031). DSS (Log rank test; p = 0.025) and DFS (Log rank test; p = 0.024) in patients who did not consume alcohol were significantly higher comparing to patients who consume alcohol. Significantly, lower OS, DSS and DFS were noted in patients with histologically poorly differentiated tumors (Log rank, p < 0.05). DSS was significantly lower in patients with anterior commissure involvement and positive surgical margins. In patients who underwent postoperative RT, OS (Log rank, p = 0.034) and DSS (Log rank, p = 0.033) were significantly lower comparing to patients who underwent only surgical treatment. DFS was significantly lower in patients with anterior commissure involvement, patients with T1b and patients who underwent cordectomies type Vb and VI (Log rank, p ˂ 0.05). DSS and DFS for patients with T2 stage were satisfactory in the follow-up period. For further analysis, we divided T2 patient to two subgroups, one without impaired vocal cord mobility and other with impaired vocal fold mobility. DFS in T2 patients with impaired vocal fold mobility proved to be significantly lower comparing to those without impaired vocal cord mobility (5-year DFS 64.7% vs. 84.3%, respectively). Laryngeal preservation significantly influenced 5-year OS, DSS and DFS (Log rank, p ≤ 0.001) (Table 2).
Multivariate Cox regression analysis showed that age, histological tumor grade and laryngeal preservation were significant prognostic factors influencing 5-year DSS (Table 3). DSS was negatively influenced by age (HR = 1.43, p = 0.005), alcohol consumption (HR = 11.62, p = 0.022), histological G2 (moderately differentiated) (HR 3.453, p = 0.006) and G3 (poorly differentiated) (HR 4.069, p = 0.004) tumor grade, if a patient underwent cordectomy type VI (HR 6.43, p = 0.041) and if larynx was not preserved (HR 10.04, p = 0.001). 5-year DFS was negatively influenced by age (HR = 1.048, p = 0.043), histological G2 (moderately differentiated) (HR 2.022, p = 0.001) and G3 (poorly differentiated) (HR 3.541, p = 0.024) tumor grade, and if larynx was not preserved (HR 3.31, p = 0.001). In multifactorial analysis, T2 stage was not significant prognostic factor for DFS, but subgroup of T2 stage with impaired vocal ford mobility proved to be significant negative prognostic factor (HR 1.045, p = 0.047). In this study, 5-year DSS and DFS were not significantly influenced by types of endoscopic cordectomies which patients were committed to.
Discussion
Age of the patients significantly influenced OS rates in patients included in our study, which was distinguished as an important risk factor in other studies [8, 9]. Risk factors like alcohol consumption was associated with significantly lower survival in our patients. Patients with poorly differentiated laryngeal carcinoma had significantly lowest rates of OS, DSS and DFS. Other studies examining the influence of sociodemographic and clinical factors on survival of patients with laryngeal cancer confirmed those findings as well [10].
Considering T stage, 5-year OS, DSS and DFS of the patients included in the study were in concurrence with previously published studies [2, 5, 11]. Patients with T1b and T2 stages with impaired vocal fold mobility had significantly lower 5-year DFS (55.6% and 64.7%, respectively, p ≤ 0.001), comparing to other stages. Inclusion of different heterogeneous lesions into one T2 category resulted in broad outcome and survival results for patients. Several authors sub-classified T2 glottic cancer into T2a (without impaired vocal cord mobility) and T2b (with impaired vocal cord mobility), thought the official classification still does not have two subgroups [2, 5]. As in previous studies, our results highlighted the negative impact T2 tumors with impaired vocal fold mobility have on outcome, which was not noted if all T2 patients were viewed as one group. More aggressive behavior and the higher risk of recurrence in patients with T2 tumors with impaired vocal fold mobility should be recognized, and as well as the need for more extensive surgery and closer follow-up.
In this study, anterior commissure involvement significantly influenced DSS (p = 0.012) and DFS (p ≤ 0.001). Increased risk of local failure after laser surgery in cases of anterior commissure involvement was noted in the literature [12, 13], as well as in this study. Out of 28 cases with local recurrence, anterior commissure involvement was present in 15 (53.56%). This was closely linked with significantly lower 5-year DFS in T1b tumors (55.6%), and in patients where type Vb (66.7%) and VI (60%) cordectomies were done. Other types of cordectomies did not significantly influence 5-year DFS, and was 85.7% and above. Anterior commissure involvement poses a complex issue in choice of treatment modality. Comparing to other treatment modalities like radiotherapy and open surgery, laser surgery delivered equally good oncological results in cases [14, 15]. It is our position that anterior commissure involvement should not be considered a contraindication for laser surgery. These patients should have close follow-up due to higher risk of local recurrence and further treatment.
The aim of endoscopic surgery is complete removal of the tumor with clear surgical margins, as positive margins increase the risk of local recurrence and survival. DSS was significantly lower in patients (96.7% vs. 90.3%) with positive surgical margins (p = 0.049). Most of our patients with positive surgical margins underwent revision surgery, which is also recommended by many authors [16]. In cases of revision surgery, residual tumors were discovered in 17% to 58% of the cases, so it could be argued that the majority of the patients are over treated with repeated surgery [17]. That percentage in our study was close to those limits, where residual tumors were discovered in 17 patients (58.6%). Repeated resection was done in the same Acublade mode with 10–12 W. Some Italian authors proposed post-resection CO2 laser photocoagulation of surgical close or positive superficial margins, which significantly decreased rate of local recurrences [18, 19]. In our study, 23 patients with positive surgical margins underwent adjuvant RT. This is mainly due the fact that in the first 3 years of the study all patients with positive surgical margins underwent RT, which was preferred treatment in that time. We embraced revision surgery as an alternative to RT later in the study. After administrating adjuvant RT, dose-related complications such as severe laryngeal edema, radionecrosis, laryngeal stenosis, aspirational pneumonia and tracheostomy dependence were reported in the literature. It was also suggested that patients should not receive more than 50 Gy, achieving the same local control of the disease [20]. In our study, OS and DSS were significantly lower in patients who underwent RT, comparing to those who were treated only surgically. In multifactorial analysis, RT was not significant prognostic factor. Further in the follow-up period, four patients who received RT because of positive surgical margins and anterior commissure involvement had a recurrent disease and due to the extent of the process total laryngectomy was done. Now, it is our position that surgery, preferably TLM, should be the first treatment method in cases of residual tumors or recurrent disease.
In our study, 12 (5.1%) of the patients underwent temporal tracheotomy. Main reason was intraoperative bleeding in 8 cases, followed by severe dyspnea in 4 cases. Tracheostomies were closed in all cases before discharge, and this did not significantly influence survival of the patients included in the study. Incidence of temporal tracheotomy in the literature is below 6% [11, 16, 21]. The experience of the surgeon plays an important role in reducing unwelcome postoperative events such tracheostomy [22].
Laryngeal preservation rates for patients treated with laser TLM are high, for T1 tumors between 95 and 97.1%, [23,24,25], and for T2 tumors 82.5 to 93% [2, 5, 25]. This method of treatment leaves all salvage options open if needed. In our study, 5-year laryngeal preservation rate was 94%, for T1 tumors 97.56% and for T2 tumors 90.1%. Out of 28 patients with local recurrence, 14 patients underwent total laryngectomy and 14 underwent repeated TLM. Total laryngectomy was done because of thyroid cartilage infiltration in 4 cases with T1b stage, or extralaryngeal spread of the tumor in 10 cases with T2 tumors. Poorer local control was noted in tumors with anterior commissure involvement and recurrent disease spreading to the supraglottic or subglottic region, due to close contact to pre-epiglottic space and subglottic area [26]. Anterior transcommissural extension of the recurrent tumor after RT was identified as a negative predictor on OS [27]. In our study, four of the patients who underwent total laryngectomy previously had RT because of positive surgical margins and anterior commissure involvement. Literature data underline that oncological outcomes of salvage therapy are not significantly worse comparing to oncological outcomes of primary treated patients. This should be acknowledged, as TLM surgery becomes an important tool in salvage therapy, not only in primary therapy [28].
Though the study included a significant number of patients with early laryngeal carcinoma who underwent laser TLM, there are a few limitations. The study is retrospective in character, so the used data are limited. Stroboscopic findings were not available for every included patients in the postoperative follow-up period, so data about vibration patterns, scaring and anterior commissure web formation were not available, and, therefore, were not included in the study. Not all the patients underwent vocal assessment preoperatively and 6 months postoperatively, which could have led to inclusion biases considering the followed vocal parameters.
Conclusions
Laser transoral laryngeal microsurgery had excellent survival rates and local control of the disease and should be first-choice treatment for early laryngeal cancer. Anterior commissure involvement, positive surgical margins and postoperative RT negatively influenced survival rates. Age and histological tumor grade were significant negative prognostic factors. Laryngeal preservation was positive prognostic factor for survival. Patients with anterior commissure involvement, patients with T1b stage, T2 stage with impaired vocal fold mobility, and patients who underwent cordectomies type Vb and VI had high risk of local recurrence. In conclusion, transoral laryngeal microsurgery delivers excellent oncological results as primary and salvage therapy, even in selected patients with higher stages of early laryngeal cancer and anterior commissure involvement.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386. https://doi.org/10.1002/ijc.29210
Canis M, Martin A, Ihler F, Wolff HA, Kron M, Matthias C, Steiner W (2014) Transoral laser microsurgery in treatment of pT2 and pT3 glottic laryngeal squamous cell carcinoma—results of 391 patients. Head Neck 36(6):859–866. https://doi.org/10.1002/hed.23389
Remacle M, Van Haverbeke C, Eckel H, Bradley P, Chevalier D, Djukic V, de Vicentiis M, Friedrich G, Olofsson J, Peretti G, Quer M, Werner J (2007) Proposal for revision of the European Laryngological Society classification of endoscopic cordectomies. Eur Arch Otorhinol 264(5):499–504. https://doi.org/10.1007/s00405-007-0279-z
Remacle M, Eckel HE, Antonelli A, Brasnu D, Chevalier D, Friedrich G, Olofsson J, Rudert HH, Thumfart W, de Vincentiis M, Wustrow TP (2000) Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society. Eur Arch Otorhinolaryngol 257(4):227–231. https://doi.org/10.1007/s004050050228
Day AT, Sinha P, Nussenbaum B, Kallogjeri D, Haughey BH (2017) Management of primary T1–T4 glottic squamous cell carcinoma by transoral laser microsurgery. Laryngoscope 127(3):597–604. https://doi.org/10.1002/lary.26207
Gallo A, de Vincentiis M, Manciocco V, Simonelli M, Fiorella ML, Shah JP (2002) CO2 laser cordectomy for early-stage glottic carcinoma: a long-term follow-up of 156 cases. Laryngoscope 112(2):370–374. https://doi.org/10.1097/00005537-200202000-00030
Brandstorp-Boesen J, Sørum Falk R, Boysen M, Brøndbo K (2017) Impact of stage, management and recurrence on survival rates in laryngeal cancer. PLoS One 12(7):e0179371. https://doi.org/10.1371/journal.pone.0179371
Gioacchini FM, Tulli M, Kaleci S, Bondi S, Bussi M, Re M (2017) Therapeutic modalities and oncologic outcomes in the treatment of T1b glottic squamous cell carcinoma: a systematic review. Eur Arch Otorhinolaryngol 274(12):4091–4102. https://doi.org/10.1007/s00405-017-4736-z
Saini AT, Genden EM, Megwalu UC (2016) Sociodemographic disparities in choice of therapy and survival in advanced laryngeal cancer. J Otolaryngol 37(2):65–69. https://doi.org/10.1016/j.amjoto.2015.10.004
de Graeff A, de Leeuw JR, Ros WJ, Hordijk GJ, Blijham GH, Winnubst JA (2001) Sociodemographic factors and quality of life as prognostic indicators in head and neck cancer. Eur J Cancer 37(3):332–339. https://doi.org/10.1016/S0959-8049(00)00385-3
Breda E, Catarino R, Monteiro E (2015) Transoral laser microsurgery for laryngeal carcinoma: survival analysis in a hospital-based population. Head Neck 37(8):1181–1186. https://doi.org/10.1002/hed.23728
Rödel RM, Steiner W, Müller RM, Kron M, Matthias C (2009) Endoscopic laser surgery of early glottic cancer: involvement of the anterior commissure. Head Neck 31(5):583–592. https://doi.org/10.1002/hed.20993
Mizrachi A, Rabinovics N, Hilly O, Shvero J (2014) Analysis of failure following transoral laser surgery for early glottic cancer. Eur Arch Otorhinolaryngol 271(8):2247–2251. https://doi.org/10.1007/s00405-014-2964-z
Mendelsohn AH, Kiagiadaki D, Lawson G, Remacle M (2015) CO2 laser cordectomy for glottic squamous cell carcinoma involving the anterior commissure: voice and oncologic outcomes. Eur Arch Otorhinolaryngol 272(2):413–418. https://doi.org/10.1007/s00405-014-3368-9
Taylor SM, Kerr P, Fung K, Aneeshkumar MK, Wilke D, Jiang Y, Scott J, Phillips J, Hart RD, Trites JR, Rigby MH (2013) Treatment of T1b glottic SCC: laser vs. radiation—a Canadian multicenter study. J Otolaryngol Head Neck Surg 42:22. https://doi.org/10.1186/1916-0216-42-22
Blanch JL, Vilaseca I, Bernal-Sprekelsen M, Grau JJ, Moragas M, Traserra-Coderch J, Caballero M, Sabater F, Guilemany JM, Alos L (2007) Prognostic significance of surgical margins in transoral CO2 laser microsurgery for T1–T4 pharyngo-laryngeal cancers. Eur Arch Otorhinolaryngol 264(9):1045–1051. https://doi.org/10.1007/s00405-007-0320-2
Hartl DM, Ferlito A, Brasnu DF, Langendijk JA, Rinaldo A, Silver CE, Wolf GT (2011) Evidence-based review of treatment options for patients with glottic cancer. Head Neck 33(11):1638–1648. https://doi.org/10.1002/hed.21528
Lucioni M, Bertolin A, D'Ascanio L, Rizzotto G (2012) Margin photocoagulation in laser surgery for early glottic cancer: impact on disease local control. Otolaryngol Head Neck Surg 146(4):600–605. https://doi.org/10.1177/0194599811433270
Galli A, Giordano L, Sarandria D, Di Santo D, Bussi M (2016) Oncological and complication assessment of CO2 laser-assisted endoscopic surgery for T1–T2 glottic tumours: clinical experience. Acta Otorhinolaryngol Ital 36(3):167–173. https://doi.org/10.14639/0392-100X-643
Laccourreye O, Hans S, Borzog-Grayeli A, Maulard-Durdux C, Brasnu D, Housset M (2000) Complications of postoperative radiation therapy after partial laryngectomy in supraglottic cancer: a long-term evaluation. Otolaryngol Head Neck Surg 122(5):752–757. https://doi.org/10.1067/mhn.2000.98756
Preuss SF, Cramer K, Klussmann JP, Eckel HE, Guntinas-Lichius O (2009) Transoral laser surgery for laryngeal cancer: outcome, complications and prognostic factors in 275 patients. Eur J Surg Oncol 35(3):235–240. https://doi.org/10.1016/j.ejso.2008.01.012
Vilaseca-González I, Bernal-Sprekelsen M, Blanch-Alejandro JL, Moragas-Lluis M (2003) Complications in transoral CO2 laser surgery for carcinoma of the larynx and hypopharynx. Head Neck 25(5):382–388
Peretti G, Piazza C, Cocco D, De Benedetto L, Del Bon F, Redaelli De Zinis LO, Nicolai P (2010) Transoral CO(2) laser treatment for T(is)–T(3) glottic cancer: the University of Brescia experience on 595 patients. Head Neck 32(8):977–983. https://doi.org/10.1002/hed.21278
Ansarin M, Cattaneo A, De Benedetto L, Zorzi S, Lombardi F, Alterio D, Rocca MC, Scelsi D, Preda L, Chiesa F, Santoro L (2017) Retrospective analysis of factors influencing oncologic outcome in 590 patients with early-intermediate glottic cancer treated by transoral laser microsurgery. Head Neck 39(1):71–81. https://doi.org/10.1002/hed.24534
Sjögren EV (2017) Transoral laser microsurgery in early glottic lesions. Curr Otorhinolaryngol Rep 5(1):56–68. https://doi.org/10.1007/s40136-017-0148-2
Motta G, Esposito E, Motta S, Tartaro G, Testa D (2005) CO(2) laser surgery in the treatment of glottic cancer. Head Neck 27(7):566–573. https://doi.org/10.1002/hed.20135
Peretti G, Piazza C, Mora F, Garofolo S, Guastini L (2016) Reasonable limits for transoral laser microsurgery in laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg 24(2):135–139. https://doi.org/10.1097/MOO.0000000000000240
Del Bon F, Piazza C, Mangili S, Redaelli De Zinis LO, Nicolai P, Peretti G (2012) Transoral laser surgery for recurrent glottic cancer after radiotherapy: oncologic and functional outcomes. Acta Otorhinolaryngol Ital 32(4):229–237
Funding
The research was performed as part of the employment of the authors, working at the Clinic for otorhinolaryngology and maxillofacial surgery, Clinical Center of Serbia, Belgrade, Serbia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Djukic, V., Milovanović, J., Jotić, A.D. et al. Laser transoral microsurgery in treatment of early laryngeal carcinoma. Eur Arch Otorhinolaryngol 276, 1747–1755 (2019). https://doi.org/10.1007/s00405-019-05453-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05453-1