Abstract
Objective
The aim of this study was to investigate the potential protective and therapeutic effects of milrinone, a specific phosphodiesterase (PDE) III inhibitor, on acoustic trauma-induced cochlear injury and apoptosis.
Methods
A total number of 30 healthy Wistar albino rats were evenly divided into five groups as follows: group 1 was assigned as control group; group 2 and 3 were assigned as low-dosage groups (0.25 mg/kg) in which milrinone was administered 1 h before acoustic trauma (AT) and 2 h after AT, respectively; group 4 and 5 were assigned as high-dosage groups (0.50 mg/kg) in which the drug was administered 1 h before AT and 2 h after AT, respectively. Except control group, all treatment groups received a single dosage of milrinone for 5 days. Distortion product otoacoustic emissions (DPOAE) measurements were recorded before AT as well as at second and fifth post-traumatic days. At the end of fifth day, all rats were sacrificed and the cochlea of the rats was removed for histopathological evaluation. In addition, the groups were compared in terms of apoptotic index via caspase-3 staining.
Results
In terms of signal-to-noise ratio (SNR), there was no statistically significant difference among the groups following AT (p > 0.05). After 5 days of milrinone treatment, the best SNR values were found in group 5, though all groups did not statistically differ (p > 0.05). In histopathological evaluation, vacuolization, inflammation, and edema scores in all treatment groups were statistically lower than those of the control group (p < 0.05). In group 2 and 4 where the drug was administered before AT, the inflammation and apoptosis index was lower than those of group 3 and 5 where the drug was administered after AT (p < 0.0001).
Conclusion
We reveal that milrinone has a protective effect on cochlear damage in the experimental acoustic model of rats. This protective effect was more apparent following the pre-traumatic milrinone administration, and is associated with its effect on decreasing inflammation and apoptosis. Based on DPOAE measurements following AT, especially in the group 5 (high-dosage group), milrinone may also have a therapeutic effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While noise is increasingly encountered in our daily life, noise-induced hearing loss (NIHL) has become a serious public health concern [1]. According to the World Health Organization (WHO), it is estimated that almost 10% of world population is exposed to excessive noise which can potentially cause NIHL. Auditory hair cells loss is one of the major causes of NIHL. Since hair cells in mammals can never be replaced, preventing hair cell death or a therapeutic intervention in early stage of NIHL is critical to maintain hearing ability [2]. Though various mechanisms have been described so far for NIHL, its pathogenesis has not been totally explained yet. Apoptosis in the organ of corti is thought to be the main factor leading to NIHL [3]. Producing reactive oxygen species (ROS) because of increased metabolic activity, cellular necrosis of the outer hair cells induced by mechanical trauma, and decreased blood flow to the inner ear (causing hypoxia) are among the major causes of the cell death following AT [4, 5]. Therefore, researchers have previously used a variety of pharmacological agents to increase the blood flow and to reduce the oxidative stress on the cochlea, inflammation, and apoptosis in NIHL. Thymoquinone, pentoxifylline, N-acetylcysteine, and dexamethasone are just few examples of the agents [6,7,8]. The efficacy of pentoxifylline, a nonspecific phosphodiesterase inhibitor, in preventing NIHL was previously demonstrated in the experimental study conducted on guinea pigs. In that study, the protective effect of pentoxifylline was reported to be associated with vasodilatation and increased cochlear blood flow [9].
The hair cells lost due to the decreased blood flow in inner ear, hypoxia, inflammation, ROS production, and increased apoptosis plays a major role in the pathogenesis of NIHL. Therefore, an optimal pharmacological agent preventing NIHL should increase the blood flow and reduce ROS production, hypoxia, inflammation, and apoptosis.
Milrinone, a phosphodiesterase (PDE) III inhibitor, is generally used in acute congestive heart failure. Cardioprotective effects of milrinone associated with increasing heart muscle contraction, providing vasodilatation, and reducing inflammatory damage produced by tumor necrosis factor-alpha (TNF-alpha) have been previously established [10, 11]. Reducing ischemia-reperfusion injury in the heart, lung, liver, and kidney of rats with milrinone administration was also reported [12,13,14]. In addition, it has been demonstrated in several studies that milrinone decreases apoptosis [15, 16], shows an anti-inflammatory effect [17], and decreases the releasing of free oxygen radicals [18]. Tissue perfusion is also increased by means of vasodilatation, anti-inflammatory, and anti-aggregan effects of milrinone on regulating the microcirculation [19]. Likewise, milrinone increases the calcium entry into the cell by activating the calcium sensitive signaling cascades, resulting in a considerable neuroprotective effect on ischemic brain [20]. Taking all into consideration, milrinone with its vasodilation effect may be an ideal agent to prevent cochlear damage following NIHL and to reduce hearing loss by increasing blood flow and decreasing ROS production, hypoxia, inflammation, and apoptosis. To the best of our knowledge, a potential preventive effect of milrinone on hearing loss following an acoustic trauma has not been reported to date. The purpose of this present study was to investigate the potential preventive or/and therapeutic effects of milrinone on cochlear damage following experimental AT in rats.
Materials and methods
Ethic statement
The experimental protocol was approved by the local institutional animal ethics review committee (permit no: 09.02.2018/01-12). All experiments were conducted in compliance with the relevant laws and institutional guidelines.
Animals and study groups
Thirty healthy Wistar albino rats, weighing between 250 and 350 g, were included in this study. All rats were initially exposed to experimental AT. Following the AT, these rats were randomly assigned into the following five groups:
-
Group 1 (control; n = 6) did not receive any drug.
-
Group 2 [low-dosage milrinone group (LD 1); n = 6] received 0.25 mg/kg of intraperitoneal milrinone 1 h before AT and the same dosage was continued daily based during 5 days after AT.
-
Group 3 [low-dosage milrinone group (LD 2); n = 6] received 0.25 mg/kg of intraperitoneal milrinone 2 h after AT and the same dosage was continued daily based during 5 days after AT.
-
Group 4 [high-dosage milrinone group (HD 1); n = 6] received 0.5 mg/kg of intraperitoneal milrinone 1 h before AT and the same dosage was continued daily based during 5 days after AT.
-
Group 5 [high-dosage milrinone group (HD 2); n = 6] received 0.5 mg/kg of intraperitoneal milrinone 2 h after AT and the same dosage was continued daily based during 5 days after AT.
In each group, the rats were housed in separate cages located in a temperature-controlled room (~ 20 °C) under a 12-h light/dark cycle. All rats had free access to food and water. The level of background noise was frequently measured and kept below 50 dB at all times. During the experiment period, external ear canal and tympanic membrane of rats were periodically examined by an otoscope, and removed any secretion and obstruction like earwax that can potentially influence the test outcomes. Rats with pathological findings including serous otitis, acute otitis, and chronic otitis were excluded from the study. AT and hearing function test of the rats were performed under anesthesia through mixture of intraperitoneal 75 mg/kg ketamine hydrochloride (Ketalar, Pfizer, Turkey) and 10 mg/kg xylazine hydrochloride (Rompun®, Bayer AG, Leverkusen, Germany).
Acoustic trauma model
Under anesthesia, all rats were first located in a quite cabin. For AT procedure, the rats were exposed to 120 dB SPL, 4 kHz white noise for 4 h using GSI Two-Channel Audiometer clinical audiometry device and binaural speakers, while the rats’ head was located at 5–7 cm far away from the speaker.
Hearing function test: DPOAE measurements
DPOAE measurement was carried out in the audiology room (the noise level not exceeding 50 dB) to test the hearing function of both ears for each rat. DPOAE measurements were performed three times at different time points (i.e., before AT, second hour and fifth day after AT) through placing an infant size hearing probe [5 Ear Tip Lamelae, firmware version 2.3 ALL (build 9133, 2018-1-16), Germany] into the external ear canal. The average test time was limited to 60 s. Acoustic stimuli was occurred via two tones (f1 and f2, f1 < f2, f2:f1 ratio fixed at 1.22). These tones at the stimulus level of 65 and 55 dB by two separate speakers were consecutively delivered, and DPOAE values were recorded at four frequencies below the geometrical average of f1 and f2, namely at 1000, 2000, 4000, and 6000 Hz. We considered the significance in DPOAE amplitudes if they were at least 3 dB above the noise threshold. Signal-to-noise ratio (SNR) was also used to assess DPOAE outcome, since SNR is more trustworthy approach than DPOAE amplitudes. Displaying SNR frequency–response curves was realized with measuring SNR for each frequency using Sentiero Advanced (Path Medical GmbH, Germany).
Histopathologic analysis
Following the experimental phase, the rats were sacrificed at fifth post-trauma day and the inner ear was totally removed. The samples were immediately placed into a 10% formaldehyde buffer solution, and sent for pathological evaluation. After standard decalcification procedure, the samples were fixed in 10% formaldehyde buffer solution for 48 h. These samples following the routine tissue processing for pathological analysis were embedded in paraffin blocks and cut in 4 µm sections. Afterwards, the sections were stained with Hematoxylin and Eosin (H&E) for histopathologic observation by a light microscopy (Olympus BX51, Japan). Two pathologists without knowing group assignment evaluated blindly the samples specifically for the parameters associated with acoustic trauma damage such as stria vascularis vacuolization, inflammatory cell infiltration, and edema. Semi-quantitative scores were used to evaluate the samples: 0 = no presence, 1 + = mild, 2 + = moderate, and 3 + = severe.
Caspase-3 (apoptotic index) evaluation
As described previously [21], caspase-3 localization was performed in paraffin-embedded cochlea by immunohistochemistry using a standard avidin–biotin peroxidase complex technique. A polyclonal rabbit anti-human Caspase-3 antibody (Ventana, Roche, USA) recognizing the 32 and 17 kD Caspase-3 subunits with no cross reactivity against other caspase family members (manufacturer's specification) were diluted 1:100 and then applied overnight at 4 °C in a humid atmosphere. Thereafter, the sections were stained by an avidin-biotinylated HRP procedure using a commercially available kit (ABC Elite, Vector Laboratories). AEC was used as the substrate. Finally, sections were counterstained with hematoxylin. Negative control sections were incubated with normal mouse IgG or normal rabbit serum at the same protein concentration as the primary antibody. Human tonsil tissue is used as a positive control.
The apoptotic index was then calculated using the following formula:
where mean Caspase-3 refers the mean number of Caspase-3 positive cells in five random fields, and mean total cells refers the mean number of total cells in five random fields.
Statistical analysis
All statistical analyses were conducted with SAS/STAT version 9.3 (SAS Institute, Inc, Cary, North Carolina, USA). Normality assumptions of SNR values and apoptotic index scores were confirmed with Kolmogorov–Smirnov and Shapiro–Wilk tests. The apoptotic index scores at post-traumatic fifth day and the SNR values at each measurement time point (before AT, second hour and fifth day after AT) among the five groups were compared by one-way ANOVA. The SNR values were also compared among the three measurement time points within each group by one-way ANOVA. Tukey’s multiple comparisons test was used for pairwise differences between the groups. Distribution of the five groups among vacuolization, inflammation, and edema scores were compared by Chi-square and Fisher’s exact test. p values less than 0.05 were considered statistically significant level.
Results
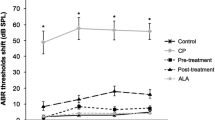
DPOAE results
There was no statistically significant difference in terms of pre-trauma and post-trauma DPOAE outcome among the groups (p > 0.05). However, post-traumatic SNR values were found to be significantly lower than that of pre-traumatic values (the SNR values at before AT and fifth post-trauma day).
Within-group comparisons
In all groups after AT, we observed an overall decrease in SNR values at higher frequencies starting from 2000 kHz. More specifically, in the group 1 (control) at fifth post-trauma day, the decline in SNR values at 6000 kHz in right ear was statistically significant (p < 0.05), though the SNR values at other frequencies had also a trend of decreasing, but did not reach a statistically significant level. Regardless of frequencies, all SNR values of left ear at the fifth post-trauma day were significantly lower than those of pre-traumatic values (p < 0.05) (Fig. 1).
In the group 4 (HD 1), there were significant decreases in the SNR values of both ears at 4000 and 6000 kHz at fifth post-trauma day when compared to the pre-traumatic values (p < 0.05), while the pre- and post-traumatic SNR values at 1000 and 2000 kHz did not significantly differ.
In the group 2 (LD 1), although it did not reach the significance level, there was a trend of improvement in the post-traumatic SNR values of right ear at all frequencies, when compared to the pre-traumatic values. For the left ear, the post-traumatic SNR values at 4000 and 6000 kHz were significantly lower than those of pre-traumatic values (p < 0.05), whereas no statistically significant differences were observed at 1000 and 2000 kHz.
In the group 5 (HD 2), the pre- and post-traumatic SNR values of both ears at all frequencies did not statistically differ, though a trend of increase in post-traumatic SNR values at all frequencies was observed.
In the group 3 (LD 2), for right ear, only the post-traumatic SNR values at 4000 and 6000 kHz were statistically lower than the pre-traumatic values (p < 0.05). For left ear, along with 4000 and 6000 kHz, the post-traumatic values at 2000 kHz were also lower (p < 0.05) (Fig. 2).
Histopathologic assessment and apoptotic index
The histopathologic assessment revealed that the vacuolization, inflammation, and edema scores in all treatment groups (LD 1, LD 2, HD 1, and HD 2) were statistically lower than those of the control group (p = 0.02). Significant decreases in the vacuolization, inflammation and edema scores of LD 1 and HD 1 groups were also found when compared to those scores of LD 2 and HD 2 (p < 0.05). Furthermore, a decreasing trend in the scores was observed for HD 1 and HD 2 groups, comparing to LD 1 and LD 2 groups, respectively, though this trend did not reach a statistically significant level (p > 0.05) (Fig. 3).
The apoptotic index scores of all treatment groups were statistically lower than that of the control group (p < 0.0001). We also found a statistically significant decrease in the apoptotic index scores of LD 1 and HD 1 groups when compared to those of the LD 2 and HD 2 groups (p > 0.05). Finally, between low- (LD 1 and LD 2) and high-dosage (HD 1 and HD 2) groups, there was no statistically significant difference in terms of apoptotic index score (p > 0.05) (Figs. 4, 5).
Hematoxyline and eosine staining of the rat cochlea. a Inflammation in stria vascularis (asterisks) and epithelial disarray (arrows) ( × 200). b Edema in stria vascularis (arrow) and blister formation (asterisks) ( × 40). c Plasma cell infiltration and severe inflammation in control group ( × 200). d Reduced inflammation in high dose milrinone group (HD 1)
Caspase-3 immunohistochemistry staining of the rat cochlea. a Large number of apoptotic cells (caspase-positive) in control group ( × 200). b High apoptotic score is observed at a large magnification in control group ( × 400). c Apoptotic cells appear to be partially reduced in the low-dose milrinone-treated group (LD 2) moderate apoptotic cells (black arrows) ( × 400). d Apoptotic cells appear to be significantly reduced in the high-dose milrinone-treated group (HD 1) moderate apoptosis cells (black arrows) ( × 400)
Discussion
The main factor leading to NIHL is thought to be apoptosis in the organ of corti, though several other mechanisms have been also described, yet its pathogenesis remains unclear [3]. An excessive noise exposure can potentially cause permanent hearing loss damage due to the bending, fusion, or damage of hair cell stereocilia which, consequently, leads to hair cell vacuolization and death. The lost hair cells are then replaced with squamous epithelium that causes scar formation [22].
Another pathophysiological mechanism of NIHL is the decrease in blood flow in the cochlear [23]. Therefore, in the past, several agents such as Mg, pentoxifylline, gingko biloba, and SQ 29,548 were used to increase cochlear blood flow [8, 9, 24]. However, the effect of increased cochlear blood flow on hearing is still controversial. A limited number of studies reported an improvement on both NIHL and hearing ability following the increased cochlear blood flow [25, 26]. On the other hand, Lamm et al. [27] reported that pentoxifylline, a nonspecific phosphodiesterase inhibitor, increases the cochlear blood flow without any therapeutic effect on hearing improvement. In the same study, an improvement in hearing functions was achieved with HES 70 treatment despite of decreased cochlear blood flow, indicating no association between cochlear blood flow and hearing functions [27]. Contrariwise, Kansu et al. [9] reported an improvement on histopathologic findings and auditory brainstem response (ABR) of guinea pig with pentoxifylline treatment. The potential protective effect of pentoxifylline on NIHL was thought to be associated with increased cochlear blood flow and regulating microcirculation [9].
Milrinone as a specific phosphodiesterase type III inhibitor is a bipyridine methyl carbonitrile analog of amrinone with inotropic and direct vasodilator action. The previous experimental study showed that milrinone is 10–30 times more effective than amrinone with considerable fewer side effects [28]. Because of its vasodilator action, we thought that milrinone can potentially increase cochlear blood flow and microcirculation.
Increased inflammatory response is suggested as another mechanism leading to NIHL. Experimental and clinical studies on inflammation showed that the administration of steroids systematically and transtympanically has protective and therapeutic effects on NIHL [8]. In the experimental NIHL model of rat, Arslan et al. [29] reported the anti-inflammatory effect of dexamethasone and an improvement on ABR test following dexamethasone treatment compared to non-treatment group [29]. Besides vasodilator and inotropic action of milrinone, it has independently anti-inflammatory effect [30]. Previously, it was reported that, by the means of cyclic adenosine monophosphate (cAMP) increase, milrinone decreases TNF-alpha induced inflammatory response and edema formation, and recovers endothelial functions [11, 31]. Likewise, in our study, significant decreases in the vacuolization, inflammation, and edema scores in all treatment groups, comparing to control group suggest that milrinone reduces inflammation and edema on the cochlea.
More recent studies reported that ischemia–reperfusion damage due to the decreased blood flow plays a role in the pathogenesis of NIHL [32]. Similarly, free ROS production and accumulation also play a role in the pathogenesis of NIHL [33]. Therefore, neuroprotective effect with decreased ROS and increased antioxidant mechanism can protect organism from NIHL [34, 35]. Before ischemia, phosphodiesterase III inhibitors administration in different species (e.g., rats, dogs, and rabbits) and organs (e.g., liver heart) prevents ischemia-reperfusion injury [13, 14, 36, 37]. Along with preventing ischemia-reperfusion, milrinone shows antioxidant effect with decreasing ROS production [38]. Taking all into consideration, in our study, the improvements in the treatment groups could be also associated with antioxidant effect of milrinone.
Excessive noise, ischemia, or hypoxia-induced apoptosis is the eventual step in the pathogenesis of NIHL. The protective effects of several anti-apoptotic agents were previously reported [8]. For example, Wang et al. [39] demonstrated the protective effect of X-linked inhibitor of apoptosis protein (XIAP) overexpression on NIHL. It is known that intracellular c-AMP level is altered with apoptosis, and the reactive chemicals leading to an increase in intracellular c-AMP level can promote or prevent apoptosis in different tissue cells [40]. Furthermore, it was reported that milrinone exhibits anti-apoptotic effect on Rolipram, phosphodiesterase-4 (PDF-4) inhibitor, induced apoptosis [40]. Lanfear et al. [17] showed that, along with regulating hemodynamics, milrinone can suppress inflammation and decrease apoptotic biomarkers by other means in the patients with severe cardiac dysfunction [17]. In other studies on cardioprotective effect of milrinone [41] and the protective effect of milrinone on renal ischemia–reperfusion injury [15, 16], milrinone was observed to reduce apoptosis.
Caspase-3 is an important marker of the apoptotic signaling pathway [42]. Schmutzhard et al. [43] previously showed that severe sepsis-induced hearing loss can be explained with the upregulation of caspase-3-mediated apoptosis. Han et al. [21] reported caspase-3 expression in hair cell, spiral ganglion neurons, and stria vascularis through immunohistochemistry technique. In our study, we also used immunohistochemistry technique (Active Caspase-3 Antibody Staining) to investigate potential apoptosis in the cochlea, and the effect of milrinone on the prevention of apoptosis. We found that the apoptotic index scores of all treatment groups were statistically lower than that of the control group. Furthermore, the apoptotic index scores of the groups with pre-traumatic milrinone administration were significantly lower than the apoptotic index scores of the groups with post-traumatic milrinone administration, indicating that milrinone decreases apoptosis in accordance with the literature.
The neuroprotective effect of milrinone was first showed by Saklani et al. [20] that milrinone treatment in mice with ischemia–reperfusion significantly decreased cerebral infarct size and improved memory and motor coordination [20]. This therapeutic effect is considered due to the increased intracellular calcium levels via ryanodine receptors. On the other hand, it has also been found that, in ischemia-reperfusion injury model, calcium channel antagonists improve memory and exhibit neuroprotective effect [44, 45]. Consistent exposure of ischemia resulting massive intracellular accumulation of calcium ions leads to cell death because of triggering deleterious biochemical events [20]. As showed by Reetu et al. [20], milrinone treatment has a protective effect against these events. Therefore, the improved DPOAE values following the post-traumatic milrinone treatment may be also associated with the neurotherapeutic effects of milrinone.
Along with its vasodilator action, neuroprotective, anti-inflammatory, and anti-apoptotic effects, milrinone has also an anti-thrombotic effect [19]. Therapeutic dosage of milrinone inhibits adenosine, diphosphate, and arachidonic acid-induced platelet activation [46]. Decreased microvascular platelet aggression treats tissue perfusion by increasing capillary blood flow [47]. Anti-thrombotic effect of milrinone with its regulating effect on hemodynamic parameters contributes to potential protective and therapeutic effects by increasing microcirculation on the cochlea.
Several different AT models have been used in the literature such as 120 dB, 4 kHz octave band noise for 4 h, 103–107 dB SPL, 5 kHz for 4 h, and 120 dB 6 kHz noise for 40 min [48,49,50]. In our study, we used 120 dB SPL, 4 kHz white noise for 4 h. ABR, DPOAE, or both can be used to evaluate the effects of AT [48, 49], and we used DPOAE measurement in our study. AT-induced permanent hearing loss is generally observed at higher frequencies, ranging between 3000 and 6000 kHz as reported in the previous studies [3, 51]. In accordance with the previous studies, we also observed that AT mostly affected at 2000 kHz and above, while this effect was more clearly observed at 4000 and 6000 kHz. We observed that the most protective and therapeutic effect of milrinone was observed in the group 5 (HD 2) where a 0.50 mg/kg dosage was administrated after post-traumatic second hour. In this group, we observed that SNR values of both ears at all frequencies improved the level of pre-traumatic SNR values. Based on the histologic parameters, we found significant decreases in edema, inflammation, vacuolization score, and apoptotic index values of all treatment groups when compared to control group, suggesting the protective and therapeutic effects of milrinone on AT-induced hearing loss. The protective effect is more specifically observed in pre-traumatic milrinone administered groups regardless of the drug dosage.
To the best of our knowledge, our study is the first study showing the effects of milrinone on the cochlea. Thus, there were no readily available data for the optimum dosage and frequency selection of milrinone. Previously, several different dosages of milrinone have been used for different purposes. For instance, Lanfear et al. [17] used between 0.25 and 0.50 µg/kg/min dosages for the patients with severe cardiac dysfunction, and found statistically significant decrease in necrosis, apoptosis and inflammation biomarkers. Saklani et al. [20] administered 50 and 100 µg/kg/min milrinone intravenously for cerebral ischemia-reperfusion in mice model. A single dosage of 50 mg/kg milrinone was also administered intraarterially [15] and intraperitoneally [16] for kidney ischemia–reperfusion in the rat model. Desjardins et al. [52] used the varying dosage, 0.1, 0.5, 1, 5, and 10 mg/kg, of milrinone. However, 25% of the rats in the groups of 1, 5, and 10 mg/kg dosages were dead because of ventricular fibrillation. After taking all into consideration, we decided to use either 0.25 mg/kg or 0.50 mg/kg intraperitoneally because of its easy use and no necessity of catheter use. Since the effect of milrinone starts 5–10 min following the administration and its terminal half-life is around 2–3 h when single bolus dosage used [53], we decaded to administer milrinone 1 h before AT and also after AT for investigating its potential therapeutic effect.
This study is also not without limitations. The lack of ABR measurement is an important limitation. Since there is no prior research and this study is the first one, further future studies are required to determine the optimum dosage and frequency. Different dosages and the way of drug administration may also influence the outcomes. The extended period (more than 5 days after AT) of follow-up may also improve the analysis of the results. Moreover, the use of an electron microscopy technique might further help tracking ultra-structural alterations on the cochlea.
Conclusion
In summary, we showed the protective effect of milrinone against cochlear damage in NIHL. Our cumulative results suggest that this protective effect is associated with its effect on decreasing inflammation and apoptosis in the cochlea. Systematic administration of milrinone before and after AT may also have a therapeutic effect against NIHL. The investigation of optimum dosage and frequency and the possible effect of the milrinone on threshold of hearing remain to be studied in future studies.
References
Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, Stansfeld S (2014) Auditory and non-auditory effects of noise on health. Lancet 383:1325–1332
Zhang J, Song YL, Tian KY, Qiu JH (2017) Minocycline attenuates noise-induced hearing loss in rats. Neurosci Lett 639:31–35
Ogurlu M, Celebi Erdivanli O, Tumkaya L, Ozgur A, Ozergin Coskun Z, Terzi S, Demirci M, Dursun E (2017) The therapeutic effect of thymoquinone on acoustic trauma-induced hearing loss in rats. Eur Arch Otorhinolaryngol 274(2):743–749
Motalebi Kashani M, Saberi H, Hannani M (2013) Prevention of acoustic trauma-induced hearing loss by N-acetylcysteine administration in rabbits. Arch Trauma Res 1:145–150
Fetoni AR, Ralli M, Sergi B, Parrilla C, Troiani D, Paludetti G (2009) Protective effects of N-acetylcysteine on noise-induced hearing loss in guinea pigs. Acta Otorhinolaryngol Ital 29:70Y5
Gumrukcu SS, Topaloglu İ, Salturk Z, Tutar B, Atar Y, Berkiten G, Göker AE (2018) Effects of intratympanic dexamethasone on noise-induced hearing loss: an experimental study. Am J Otolaryngol 39(1):71–73
Lorito G, Giordano P, Petruccelli J, Martini A, Hatzopoulos S (2008) Different strategies in treating noiseinduced hearing loss with N-acetylcysteine. Med Sci Monit 14(8):159–164
Sakat MS, Kilic K, Bercin S (2016) Pharmacological agents used for treatment and prevention in noise-induced hearing loss. Eur Arch Otorhinolaryngol 273:4089–4101
Kansu L, Ozkarakas H, Efendi H, Okar I (2011) Protective effects of pentoxifylline and nimodipine on acoustic trauma in guinea pig cochlea. Otol Neurotol 32:919–925
Boswell-Smith V, Spina D, Page CP (2006) Phosphodiesterase inhibitors. Br J Pharmacol 147:252–257
Jung HS, Joo JD, Kim DW et al (2014) Effect of milrinone on the inflammatory response and NF-kB activation in renal ischemia-reperfusion injury in mice. Korean J Anesthesiol 66:136–142
Besirli K, Burhani SM, Arslan C et al (2006) Effect of combining phosphodiesterase III inhibitors with St Thomas Hospital’s solution used as transplantation preservative solution in isolated rat hearts. Transplant Proc 38:1253–1258
Zhang J, Chen F, Zhao X et al (2009) Nebulized phosphodiesterase III inhibitor during warm ischemia attenuates pulmonary ischemia-reperfusion injury. J Heart Lung Transplant 28:79–84
Satoh K, Kume M, Abe Y et al (2009) Implication of protein kinase A for a hepato-protective mechanism of milrinone pretreatment. J Surg Res 155:32–39
Nishiki T, Kitada H, Okabe Y, Miura Y, Kurihara K, Kawanami S, Tanaka M (2011) Effect of milrinone on ischemia-reperfusion injury in the rat kidney. Transplant Proc 43:1489–1494
Uysal E, Dokur M, Altınay S, Saygılı Eİ, Batcıoglu K, Ceylan MS, Kazımoglu H, Uyumlu BA, Karadag M (2017) Investigation of the effect of milrinone on renal damage in an experimental non-heart beating donor model. J Investig Surg 14:1–10
Lanfear DE, Hasan R, Gupta RC et al (2009) Short term effects of milrinone on biomarkers of necrosis, apoptosis, and inflammation in patients with severe heart failure. J Transl Med 7:67
White M, Ducharme A, Ibrahim R et al (2006) Increased systemic inflammation and oxidative stress in patients with worsening congestive heart failure: improvement after short-term inotropic support. Clin Sci (Lond) 110(4):483–489
Miranda ML, Pereira SJ, Santos AOMT, Villela NR, Kraemer-Aguiar LG, Bouskela E (2015) Milrinone attenuates arteriolar vasoconstriction and capillary perfusion deficits on endotoxemic hamsters. PLoS One 10(2):e0117004
Saklani R, Jaggi A, Singh N (2010) Pharmacological preconditioning by milrinone: memory preserving and neuroprotective effect in ischemia-reperfusion injury in mice. Arch Pharm Res 33(7):1049–1057
Han X, Ge R, Xie G, Li P, Zhao X, Gao L, Zhang H, Wang O, Huang F, Han F (2015) Caspase-mediated apoptosis in the cochleae contributes to the early onset of hearing loss in A/J mice. ASN Neuro 7(1):1–13
Boettcher FA, Caldwell RK, Gratton MA, White DR, Miles LR (1998) Effects of nimodipine on noise-induced hearing loss. Hear Res 121:139Y46
Lamm K, Arnold W (1996) Noise-induced cochlear hypoxia is intensity dependent, correlates with hearing loss and precedes reduction of cochlear blood flow. Audiol Neurootol 1(3):148–160
Dogan R, Sjostrand AP, Yenıgun A, Karatas E, Kocyigit A, Ozturan O (2018) Influence of Ginkgo Biloba extract (EGb 761) on expression of IL-1 Beta, IL-6, TNF-alfa, HSP-70, HSF-1 and COX-2 after noise exposure in the rat cochlea. Auris Nasus Larynx 45(4):680–685
Sendowski I (2006) Magnesium therapy in acoustic trauma. Magnes Res 19(4):244–254
Lamm K, Arnold W (1999) Successful treatment of noise-induced cochlear ischemia, hypoxia, and hearing loss. Ann N Y Acad Sci 884:233–248
Lamm K, Arnold W (2000) The effect of blood flow promoting drugs on cochlear blood flow, perilymphatic pO2 and auditory function in the normal and noise-damaged hypoxic and ischemic guinea pig inner ear. Hear Res 141:199–219
Anderson JL, Baim DS, Fein SA, Goldstein RA, Lejemtel TH, Likoff MJ (1987) Efficacy and safety of sustained (48 hour) intravenous infusion of milrinone in patients with severe congestive heart failure. A multicenter study. J Am Coll Cardiol 9:711–722
Arslan HH, Satar B, Serdar MA, Ozler M, Yilmaz E (2012) Effects of hyperbaric oxygen and dexamethasone on proinflammatory cytokines of rat cochlea in noise-induced hearing loss. Otol Neurotol 33(9):1672–1678
Kume M, Banafsche R, Yamamoto Y, Yamaoka Y, Nobiling R et al (2006) Dynamic changes of postischemic hepatic microcirculation improved by a pre-treatment of phosphodiesterase-3 inhibitor, milrinone. J Surg Res 136:209–218
Hayashida N, Tomoeda H, Oda T, Tayama E, Chihara S, Kawara T et al (1999) Inhibitory effect of milrinone on cytokine production after cardiopulmonary bypass. Ann Thorac Surg 68:1661–1667
Honkura Y, Matsuo H, Murakami S et al (2016) NRF2 is a key target for prevention of noise-induced hearing loss by reducing oxidative damage of cochlea. Sci Rep 6:19329
Kamogashira T, Fujimoto C, Yamasoba T (2015) Reactive oxygen species, apoptosis, and mitochondrial dysfunction in hearing loss. Biomed Res Int 2015:617207
Yamashita D, Shiotani A, Kanzaki S, Nakagawa M, Ogawa K (2008) Neuroprotective effects of T-817MA against noise-induced hearing loss. Neurosci Res 61(1):38–42
Fetoni AR, Paciello F, Rolesi R, Eramo SL, Mancuso C, Troiani D, Paludetti G (2015) Rosmarinic acid up-regulates the noise-activated Nrf2/HO-1 pathway and protects against noise-induced injury in rat cochlea. Free Radic Biol Med 85:269–281
Kobayashi T, Sugawara Y, Ohkubo T, Imamura H, Makuuchi M (2002) Effects of amrinone on hepatic ischemiareperfusion injury in rats. J Hepatol 37:31–38
Kucuk C, Akcan A, Akyildiz H, Akgun H, Muhtaroglu S, Sozuer E (2009) Effects of amrinone in an experimental model of hepatic ischemia-reperfusion injury. J Surg Res 151:74–79
Yoon SY, Eum JH, Cha SK, Yoon TK, Lee DR, Lee WS (2018) Prematuration culture with phosphodiesterase inhibitors after vitrification may induce recovery of mitochondrial activity in vitrified mouse immature oocytes. Biopreserv Biobank 16(4):296–303
Wang J, Tymczyszyn N, Yu Z, Yin S, Bance M, Robertson GS (2011) Overexpression of X-linked inhibitor of apoptosis protein protects against noise-induced hearing loss in mice. Gene Ther 18(6):560–568
Zhu WH, Majluf-Ctuz A, Omburo GA (1998) Cyclic AMP specific phosphodiesterase inhibitor rolipramandRo-20-1724 promoted apoptosis in HL 60 promyelocytic leukemic cells via cyclic AMP-independent mechanism. Life Sci 63:265–274
Jafari A, Baghaei A, Solgi R, Baeeri M, Chamanara M, Hassani S, Gholami M, Ostad SN, Sharifzadeh M, Abdollahi M (2015) An electrocardiographic, molecular and biochemical approach to explore the cardioprotective effect of vasopressin and milrinone against phosphide toxicity in rats. Food Chem Toxicol 80:182–192
Morrill S, He DZZ (2017) Apoptosis in inner ear sensory hair cells. J Otol 12:151e164
Schmutzhard J, Glueckert R, Pritz C et al (2013) Sepsis otopathy: experimental sepsis leads to significant hearing impairment due to apoptosis and glutamate excitotoxicity in murine cochlea. Dis Model Mech 6:745–754
Yanpallewar SU, Hota D, Rai S, Kumar M, Acharya SB (2004) Nimodipine attenuates biochemical, behavioral and histopathological alterations induced by acute transientand long-term bilateral common carotid occlusion in rats. Pharmacol Res 49:143–150
Iwasaki K, Egashira N, Takagaki Y, Yoshimitsu Y, Hatip-Al-Khatib I, Mishima K, Fujiwara M (2007) Nilvadipine prevents the impairment of spatial memory induced by cerebral ischemia combined with beta-amyloid in rats. Biol Pharm Bull 30:698–701
Wesley MC, McGowan FX, Castro RA, Dissanayake S, Zurakowski D, DiNardo JA (2009) The effect of milrinone on platelet activation as determined by TEG® Platelet Mapping™. Anesth Analg 108:1425–1429
Mariscalco MM (2006) Unlocking (perhaps unblocking) the microcirculation in sepsis. Crit Care Med 34:561–562
Murashita H, Tabuchi K, Hoshino T, Tsuji S, Hara A (2006) The effects of tempol, 3-aminobenzamide and nitric oxide synthase inhibitors on acoustic injury of the mouse cochlea. Hear Res 214:1–6
Zhuravskii SG, Aleksandrova LA, Ivanov SA, Sirot VS, Lopotko AI, Zhloba AA (2004) Protective effect of carnosine on excitable structures of the auditory apparatus in albino rats with acute acoustic trauma. Bull Exp Biol Med 137:98–102
Fetoni AR, Ferraresi A, Greca CL, Rizzo D, Sergi B, Tringali G et al (2008) Antioxidant protection against acoustic trauma by coadministration of idebenone and vitamin E. Neuroreport 19(3):277–281
Lopes AC, Otowiz VG, de Barros Lopes PM, Lauris JRP, Santos CC (2012) Prevalence of noise-induced hearing loss in drivers. Int Arch Otorhinolaryngol 16:509–514
Desjardins S, Cauchy MJ (1989) Acute effects of milrinone on the electrocardiogram and the cardiac hemodynamics of rats with pressure overload-induced congestive heart failure. Arch Int Pharmacodyn Ther 301:182–199
Baruch L, Patacsil P, Hameed A, Pina I, Loh E (2001) Pharmacodynamic effects of milrinone with and without a bolus loading infusion. Am Heart J 141:266–267
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have neither financial disclosure nor conflict of interest.
Ethical approval
The study was performed in accordance with the 2011 Guide for the Care and Use of Laboratory Animals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ceylan, S.M., Uysal, E., Altinay, S. et al. Protective and therapeutic effects of milrinone on acoustic trauma in rat cochlea. Eur Arch Otorhinolaryngol 276, 1921–1931 (2019). https://doi.org/10.1007/s00405-019-05417-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05417-5