Abstract
Purpose
Early facial nerve decompression is recommended for cases of post-traumatic facial palsy on the basis of ENoG with degeneration > 95%. There is still a dispute in the literature concerning the role and timing of surgery versus conservative treatment in such cases. This study has been planned to evaluate the outcome of conservative management in traumatic facial paralysis with regard to type of trauma, onset, and electrodiagnostic tests.
Methods
A prospective cohort study included 39 patients with post-traumatic facial palsy. All patients underwent ENoG, nerve stimulation test, HRCT temporal bone and Schirmer’s test. The patients received intravenous methylprednisolone 1 gm/day for 5 days or oral prednisolone 1 mg/kg in tapering doses for 3 weeks. Follow-up was done at 4, 12 and 24 weeks after the treatment. Surgical exploration was limited to patients showing no improvement after 12 weeks. Facial nerve function was evaluated by the HBFNS and FEMA grading systems.
Results
Among the 39 patients in the study [5 women and 34 men; mean (SD) age, 33.5 (11.37) years], facial nerve recovery with conservative treatment alone was noted in 31 patients. The first signs of clinical recovery were noted in 27 patients by 4 weeks, in 31 patients by 12 weeks. Seven patients required surgical exploration. At 24 weeks, 31 patients recovered to House–Brackmann grade I/III and 1 patient to grade IV. 19 of 26 patients with longitudinal fractures had grade I/III recovery, whereas all 6 patients with transverse fracture recovered on conservative treatment.
Conclusions
Patients with incomplete facial palsy are candidates for conservative management. It is justified to try conservative management in patients with complete facial paralysis for up to 3 months even in cases where ENoG and NET suggest poor prognosis. The presence of sensorineural hearing loss or transverse fracture at presentation does not suggest a poor prognosis for improvement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Facial palsy with an estimated incidence of 20–25 cases per 100,000 population [1] as a disease has serious impact on patient’s life as it is morbid due to loss of multiple, almost infinite, expressions under its domain. Trauma is the third most common cause of facial nerve paralysis after Bell’s palsy and infection. The most common mechanism of injury is motor vehicle crashes followed by falls and assaults. Temporal bone injury is present in 14–22% of patients with skull base fractures. Facial paralysis is seen in about half the transverse fractures and in about 20% of longitudinal fractures in which around 90% involve the facial nerve in perigeniculate region [2]. It is the fracture line along the axis of petrous pyramid, which has clinical significance. In otic capsule involving fractures, there is two times chance of facial palsy compared to sparing fractures [3]. Most injuries demonstrate impingement, contusion, stretching, intraneural hematoma, surrounding fibrosis or partial crush injuries rather than a complete transection. Indication and timing of the facial nerve decompression for facial paralysis and the anatomic extent of decompression has been subject of controversy for years. Electroneuronography (ENoG) findings of more than 90% degeneration of motor fibers within 6 days of trauma paramount in decision to proceed with surgery as suggested by some [4], while others consider combination of high-resolution CT findings and nerve excitability tests for the same [4, 5]. Most commonly, the measurement of facial nerve function is done by House–Brackmann Facial Nerve Grading System (HBFNS) [6] with interobserver reliability of 93% among the different evaluators [7]. FEMA [8] grading system is more convenient to use in patients with partial weakness. Treatment depends on accurate clinical examination, a thorough understanding of facial nerve anatomy, and appropriate diagnostic tests. In most of the cases, spontaneous recovery follows but still surgical exploration and even neurosuture may be needed for a complete coaptation and recovery. Surgical methods such as posterior tympanotomy, translabyrinthine and transmastoid approaches are used in various circumstances related to associated hearing loss and site of injury but the results in literature are unequivocal. There is dearth of studies with respect to conservative management and follow-up in cases of high-grade facial palsy. This study has been planned to evaluate outcome of conservative treatment in traumatic facial paralysis with regard to type of trauma, onset, electrodiagnostic tests (EDT’s) and final outcomes using two grading systems.
Materials and methods
A single tertiary care center prospective study included 44 patients with posttraumatic facial paralysis of age group 12–65 years. All consecutive patients attending the outpatient department and trauma center of otolaryngology and head and neck surgery between the periods from July 2016 to December 2017 were included in this study. All the patients were subjected to a detailed clinical examination. The facial palsy was graded according to HBFNS and FEMA. A full audiological evaluation, EDT’s consisting of NET (nerve excitability test) and ENoG were performed to compare the degeneration of affected motor fibers to the opposite side. These EDT’s were again repeated after 4 and 12 weeks to watch for improvement in facial outcome during medical therapy. Radiological evaluation of temporal bone was done using HRCT 1-mm-thick slices of native axial and coronal views with a bone algorithm. Even the cases with bony fracture and impingement on intact facial nerve were managed conservatively for 4 weeks before any definite surgical therapy. In topodiagnostic tests, Schirmer’s test was done. Severity of facial palsy was classified on basis of HBFNS into low grade (HB2-3), intermediate (HB 4) and high grade (HB 5–6) to compare the treatment outcomes. A modified FEMA scale was used for this study. The points allotted to every facial function were added and five grades were formed to make clinical assessment more quantifiable. Here scores 1–4 were considered grade 1 (mild), 5–7 as grade 2 (moderate), 8–10 as grade 3 (severe), 11 as grade 4 (profound) and 12–14 as grade 5 (complete). Again, grade 1–2 were considered as low-FEMA-grade facial palsy, grade 3 as intermediate and grade 4–5 as high to compare treatment outcomes. A pro forma analyzing the parameters was prepared. All patients on presentation were started on corticosteroids either intravenous methylprednisolone 1 g/day for 5 days or oral prednisolone 1 mg/kg in tapering doses for 21 days according to the severity of facial palsy in addition to methylcobalamin. Conservative measures such as eye padding at night, lubricant eye drops and facial massage were also done for increasing the tone of the facial musculature. The facial massage was explained to all the patients by the authors (SY, NKP). It was done by patients themselves by facial stroking in superior and lateral direction, and closing of affected eyelids using palmar surface of hand. This was done multiple times a day for 3 months. Surgery was considered in patients with failure of conservative treatment as verified on EDTs and measurement of facial function. A modified posterior tympanotomy via retroauricular approach as described by senior author for facial nerve decompression was used [9]. Postoperatively, patients were given low-dose prednisolone for 3 weeks along with self-facial massage at regular intervals. No other rehabilitation measures were used. NET, which is a non-invasive test, was done at 4, 12 and 24 weeks to check the status of the facial nerve.
Results
During the study period of 18 months, 44 patients fulfilling the inclusion criteria were enrolled for study. Five patients were lost to follow-up after initial investigations, so were excluded from study. The data analysis was performed for 39 patients. After 3 months of follow-up, 31 patients showed improvement on clinical grading with conservative management who were then followed up consequently, whereas 7 patients required surgical intervention as there were no signs of improvement. One patient did not have the neurosurgical clearance for surgery so was followed up conservatively. Thus, two groups were created for analysis of factors for these patients:
Group I (conservative treatment)—32 patients
Group II (required surgical treatment)—07 patients.
Demographics: (n = 39)
The mean age of patients enrolled in the study was 33.5 ± 11.37 years, range being 15–64 years. There were 34 males (87.2%) and 5 females (12.8%) in the study with a male-to-female ratio of 7:1. Road side trauma was the cause of facial palsy 33 (84.6%), fall in 4 (10.3%) and assault in 2 (5.1%) patients. All seven patients who underwent surgery had roadside accident as mode of trauma. Patients with fall and assault improved on medical treatment.
Onset of paralysis: (n = 39)
21 patients had immediate onset facial palsy, i.e. facial palsy developed within 3 days of trauma, whereas 18 patients had delayed or unknown timing of facial palsy. Patients presented to hospital with facial palsy in mean time of 24 days in case immediate onset and 39 days in cases of delayed onset. There was no significant association on improvement of symptoms in terms of type of onset paralysis (p = 0.85). Patients with complete facial palsy had immediate onset in 9 days (52.9%) and delayed onset in 8 days (47.1%). There was no significant difference in cases of high-grade palsy with different timing of onset of palsy on type of intervention required (p = 0.81).
Clinical grading of paralysis
According to HBFNS, patients with incomplete facial palsy, i.e. House–Brackmann grade 2–4 were 22 (56.4%) and high grade (House–Brackmann grade 5–6) were 17 (43.6%). Of these patients, follow-up after 6 months on conservative treatment showed 100% improvement in 22 cases of incomplete facial palsy HB grade 1–3. Among seventeen patients with complete facial palsy (HB 5–6), nine improved to HB grade 1–3, one improved to HB grade 4, whereas seven required surgical treatment. Of these seven patients, after 6 months of post-surgical treatment, six improved HB grade 1–3, one had HB grade 5 (Fig. 1).
According to FEMA, patients with incomplete facial palsy, i.e. FEMA grade 1–3 were 22 (56.4%) and high grade (FEMA grade 4–5) were 17(43.6%).
The two scales were almost homogenous in distribution and outcome of results in these patients.
Hearing loss: 30/39 patients
In patients presenting with conductive hearing loss (CHL)—19/39 patients—16 (84%) were managed conservatively as they showed improvement clinically after 3 months of follow-up. Eleven patients with conductive hearing loss had incomplete facial palsy. All of them improved to HB grade 1–2 after 6 months of follow-up on conservative management. Eight patients with CHL had complete facial palsy, of which five were managed conservatively, whereas, other three required surgical intervention. Patients with incomplete palsy and CHL showed better improvement in both hearing outcome and facial function improvement when compared to those with complete palsy (p = 0.027). At 1 month of follow-up, four improved to normal hearing. At 6 months of follow-up, nine improved to normal hearing, and six had CHL (four of them improved with residual CHL). There was a statistically significant improvement in patients with conductive loss who responded to conservative treatment p = 0.001. On the contrary, those patients who required surgical intervention did not show significant improvement in hearing p = 0.072.
Eleven patients had mixed hearing loss; among them eight were managed conservatively. At 4 weeks, none improved to normal and seven had persistent hearing loss, whereas one had CHL. At 6 months of follow-up, two improved to normal hearing and five had persistent hearing loss with one having residual CHL. There was a significant improvement in hearing in patients managed conservatively p = 0.001.
Schirmer’s test
Schirmer’s test was positive in 11 (28%) patients. 7 (64%) of them showed improvement on medical management, 6 (86%) had final outcome of low-grade HB (1–2) and one had HB grade 4. Four patients required surgical intervention. Three of them recovered to HB grade 2–3 and found to have site of injury in mastoid segment in two and perigeniculate region in one. One had HB-grade 5 with injury in labyrinthine segment.
There was no statistical significant association of Schirmer-positive patients on intervention required (p = 0.214) (Table 1).
Nerve excitability test: (n = 38)
When improvement in facial outcome was compared on basis of intervention required as per nerve excitability test in patients with incomplete (HB grade 1–4) and complete (HB grade 5–6) facial palsy, the data show 100% improvement in patients with NET < 3 mA difference between normal and abnormal sides. One patient had bilateral facial palsy, and NET showed no response due to bilateral facial palsy and hence not analyzed in the group (n = 38). There was > 3.0 mA difference on nerve excitability test (NET) in 12 (32%) individuals. Here, facial function improvement was observed in six patients on clinical grading systems so were followed up conservatively. After 6 months all six had final HB grade 1–3 (low grade). Other six patients did not recover on conservative treatment so required surgery. A significant improvement in facial function was seen in five patients who improved to HB grade 2–3, and one had final outcome of HB grade 5 (Fig. 2).
There is a significant association of improvement with conservative management when patients had NET < 3.0 mA (p = 0.001). On Fisher’s exact test, there is no significant association of NET with required intervention of treatment in terms of facial outcome in patients with complete palsy p = 0.093.
Electroneuronography (ENoG)
On ENoG, there was > 90% degeneration reported in 6 (21.4%) patients among those presented early and test performed within 7–21 days after onset of palsy. All of these six patients had high-grade facial palsy on presentation. Facial improvement was observed in three patients on clinical grading systems after 1 month so were followed up conservatively. Three patients showed no recovery after 12 weeks so were taken up for surgery. Thus, 50% patients with ENoG > 90% could be managed conservatively, whereas other 50% required delayed surgical intervention.
When improvement in facial outcome was compared on basis of intervention in association with ENoG in patients with incomplete (HB grade 1–4) and complete (HB grade 5–6) facial palsy, the data show 100% improvement in patients with ENoG < 90% (n = 28).
There is a significant association of improvement with conservative management when patients had ENoG < 90% (p = 0.001). Here also 50% patients with unfavorable ENoG recovered on conservative treatment.
Fracture (n = 39)
Longitudinal fracture was evident in 26 of 32 cases with fracture of temporal bone. 20 (77%) of these cases showed improvement in clinical grading with conservative treatment. A final outcome of HB grade 1–2 in 18 (90%), HB grade 3 in 1 and HB grade 4 in 1 was observed. 6 (23%) cases with longitudinal fracture did not recover on conservative treatment so required surgery. They all had complete facial palsy. Among them, five had final facial outcome of HB grade 2–3 and one had final HB grade 5 (Table 2).
When compared using Pearson’s chi square test, there was a significant association of incomplete facial palsy with longitudinal fracture who recovered on medical treatment p = 0.010.
6/32 patients had mixed or transverse fracture on radiology, all of them recovered on medical treatment. There was no significant association of intervention modality in patients with complete facial palsy, presenting with conductive hearing loss and longitudinal fracture on radiology (p = 0.462). Thus these patients could be managed on conservative treatment.
Group II (surgical exploration group)
Seven patients required surgical exploration. Three patients had bony impingement, three had oedema of the nerve and one patient did not have any abnormality on exploration. The facial nerve was decompressed from the geniculate ganglion to the stylomastoid foramen. 6/7 of the patients who underwent surgery had improvement of HB grade 1–3 after 6 months of follow-up.
Discussion
Fisch [10] has used three terms—neuropraxia, neurotmesis, and axonotmesis—for the three primary types of facial nerve injury. In our study, a total of 39 patients were followed up. After initial clinical examination, investigations and required intervention, these patients were followed up at a period of 1, 3 and 6 months. The treatment outcome was noted on the basis of various variables during these follow-up visits. Majority of our patients were managed conservatively with only 7 (17.9%) requiring surgery.
Men outnumbered women in terms of required intervention for treatment but the difference was not significant. No association was observed for the various age groups and required intervention for treatment. This was in concurrence with the results of Peng Xu et al. [11]. The authors concluded that age and gender do not correlate with the good recovery rate of facial paralysis after temporal bone trauma.
There is a shift in trend of intratemporal injuries towards being less severe due to invents of airbags and seatbelts, and obeying of traffic rules creating a rarity of severe nerve lesions encountered during surgery [12]. Trauma due to roadside accidents was seen in 85% of cases in our study. Majority of the accidents involved two wheelers. Therefore, the resultant trauma occurs on one side of the skull secondary to fall. However, the mode of trauma had no bearing to the intervention required in these cases. Even the patients with temporal bone trauma resulting in injury to facial nerve due to fall from height or assault recovered on conservative management.
The significance of delay in onset of symptoms of facial palsy was compared with those of immediate onset in terms of prognosis with conservative management. Onset of facial palsy (immediate or delayed) had no relation to ultimate improvement of facial palsy in our study. Most of our patients with delayed onset facial palsy who showed improvement with conservative treatment had intermediate HB grade. In our study, 60% patients with delayed onset high-grade paralysis showed improvement when treated conservatively. This was a novel finding as the fate of delayed onset complete facial nerve palsy is not clear in English literature [12]. Our results are in concurrence with findings of Turel et al. [13]. The authors suggested that delayed onset incomplete facial nerve injuries have good prognosis when treated conservatively. Similar findings were reported by Chang et al. [14]. Their patients with delayed facial paralysis did not require surgical intervention.
The patients were classified based on their severity of facial paralysis with the commonly used House–Brackmann Facial Nerve Grading System [6] and a more quantitative FEMA classification suggested by Kim et al. [8] which was modified in this study. Modified FEMA grading system overcomes the demerits of House–Brackmann grading system by quantitatively scoring individual facial function among all grades. Thus different expressions can be combined to score the grading of facial palsy that was not possible with House–Brackmann system and was more observer biased [7, 8, 15].
Both HB grading and FEMA grading scales correlated well in studying the severity of facial function and subsequent recovery. The two scales were almost homogenous in distribution and outcome of results in these patients. Both the grading systems can thus be recommended for grading the severity of facial nerve paralysis.
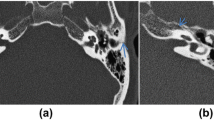
The patients with low-to-intermediate-grade facial palsy (HB grade 2–4) had complete improvement in their facial paralysis. Our results substantiated the commonly believed notion that patients with incomplete facial palsy are candidates for conservative management. This proves the reported data in the literature [12,13,14]. Regarding complete paralysis, our results showed that even patients with complete facial palsy (HB grade 5–6; FEMA grade 4–5) had improved with conservative management. This goes on to suggest that it is justified for the clinician to try conservative management in patients with complete facial paralysis for up to 3 months before any definitive surgical intervention is contemplated even in cases where ENoG and NET suggest poor prognosis. These results are similar to study conducted by Thakar et al. [16] which justifies trial of conservative management as first-line treatment for undisplaced longitudinal temporal bone fractures associated with complete facial nerve paralysis and unfavorable electrophysiological features (Figs. 3, 4).
a Patient with immediate onset facial palsy with HB grade 5; modified FEMA grade 5. b Follow-up at 1 month, HB grade 4; modified FEMA grade 3. As there was improvement clinically so patient followed up conservatively. c Follow-up at 3 months, HB grade 3; modified FEMA grade 3. d Follow-up at 6 months, HB grade 2; modified FEMA grade 1
Schirmer’s test was positive in 11/39 patients (28%) in our study. 7 (64%) of them showed improvement on medical management. Remaining four cases required surgical intervention. Here, no statistical significant association of Schirmer-positive patients was seen with required intervention. Thus, even with Schirmer’s test being positive, conservative treatment could still bring in improvement. 75% of our patients with Schirmer-positive test were false positives, a finding noted intraoperative and with postoperative facial outcomes. In one patient, site of injury could not be located, was probably in labyrinthine segment and showed House–Brackmann grade 5 after 6 months of surgery. This patient could have benefitted with a middle cranial fossa approach for decompressing labyrinthine segment. Our results were similar to the results shown by Panda et al. [17] where they showed a false-positive rate of 54.5% with positive Schirmer’s test in localizing injury.
77% of cases (30/39) had hearing loss on presentation in present study. Incudostapedial joint separation is considered as most common ossicular injury causing hearing loss as studied by Hough et al. [18], whereas sensorineural hearing loss is more common with concussion injury to cochlea as observed mostly with otic capsule involving fractures.
Conductive hearing loss was seen in 49% (n = 19/39) of all cases. Eleven patients with conductive hearing loss had incomplete facial palsy. All of them improved to HB grade 1–2 after 6 months of follow-up on conservative management. Eight patients with conductive hearing loss had complete facial palsy; 5/8 (62.5%) of them were managed conservatively, whereas other 3/8 cases required surgical intervention. Patients with incomplete palsy and conductive hearing loss showed better improvement in both hearing outcome and facial function improvement when compared to those with complete palsy. There was a statistically significant improvement of conductive loss in patients who responded to conservative treatment. On the contrary, those patients who required surgical intervention did not show significant improvement in hearing.
Among patients with mixed hearing loss, 8 (72.7%) were managed medically as they showed improvement clinically after 1 month of follow-up. 3 (16%) were managed surgically as they showed no improvement clinically after 1 month of follow-up. There was a significant improvement in sensorineural hearing loss in patients managed conservatively. Thus, the presence of sensorineural hearing loss at presentation does not mean that they would not improve on conservative treatment.
As reviewed from literature, electrodiagnostic tests such as nerve excitability test correlate with prognosis of posttraumatic facial paralysis. Patients with > 3.0 mA differences are normally considered to be subjects for surgical exploration. However, our results showed different findings. There was > 3.0 mA difference on nerve excitability test (NET) in 12 (32%) individuals. 50% of these patents with > 3 mA difference showed improvement on conservative management as evident from Fisher’s exact test. There was no significant association of NET with required intervention of treatment in terms of facial outcome in patients with complete palsy (p = 0.093). Our study also showed 100% improvement in patients with NET < 3.0 mA difference between normal and abnormal sides. There is a significant association of improvement with conservative management when patients had NET < 3.0 mA (p = 0.001).
Fisch [10] in 1974 described in a series of 40 patients the role of early surgery in fractures of petrous pyramid associated with facial nerve palsy when there is a degeneration of > 90% fibers on ENoG. This is now largely accepted as an indication of early surgery in literature [4, 10, 19, 20]. However, we got contrasting results in our study. There was > 90% degeneration reported in six (21.4%) patients among those who presented early and test performed within 7–21 days after onset of palsy. 50% (3/6) of our patients with ENoG > 90% could be managed conservatively and had final facial outcome of HB grade 1–2 after a follow-up period of 6 months. This was a novel finding and is seldom described in literature before. Additionally, other 50% patients underwent delayed surgical exploration and recovered to final HB grade 2–3 after a follow-up of 6 months. A similar finding was noted by Brodsky et al. [19] in 1983 in three patients who showed poor prognosis on ENoG and EMG, and underwent delayed surgery and recovered. This finding could be explained on the basis of early deblocking as described by Ugo Fisch [21]. Our data also showed 100% improvement in patients with ENoG < 90% degeneration (n = 28). Thus, there is a significant association of improvement with conservative management when patients had ENoG < 90% (p = 0.001). Hence the findings on NET and ENoG questions reliability of electrodiagnostic tests to be solely effective in deciding the patients requiring early surgery.
Computed tomography revealed a fracture of temporal bone in 32 (82.1%) patients out of which 26 recovered conservatively. There was no fracture in seven (17.9%) cases. Thus, the presence of fracture on computed tomography had little bearing on the required intervention. 77% (n = 20/26) of patients who had longitudinal fracture of temporal bone showed improvement in facial outcome conservatively. Thus, the patients with longitudinal fracture of temporal bone having incomplete facial palsy had a significant improvement on conservative treatment. This was in correlation with findings as observed by Turel et al. [13].
Hearing loss at presentation had no significant association with the type of fracture. We had 14 patients having conductive loss along with longitudinal fracture. Out of these 14 patients, 7 had complete facial palsy. Literature suggests surgical management as treatment of choice in such patients [22,23,24]. However, we found five of these seven cases showed improvement on conservative management.
The literature quotes a poor prognosis of sensorineural hearing loss in patients of facial palsy with transverse fracture [18, 25]. The present study had 6 out of 32 patients with mixed or transverse fracture. Three of them presented with conductive loss and two with mixed hearing loss. Here, the presence of transverse fracture does not rule out conservative treatment. In fact four out of these six patients had improved to normal hearing and all of them had final facial outcome of HB grade 1–3 on conservative treatment.
The literature also quotes poor prognosis for facial paralysis associated with transverse fracture and SNHL [18, 25]. However, in our present study, three out of six patients with mixed or transverse fracture presented with conductive loss while two with mixed hearing loss. When started on conservative therapy, four of these showed improvement to normal hearing while all six of them had final facial outcome of HB grade 1–3.
Average time for surgery from onset of facial palsy was 2–3 months. All seven patients underwent facial nerve decompression with modified posterior tympanotomy approach [9]. We had three out of eight (37.5%) cases of delayed onset facial palsy following trauma that showed no improvement after 4 weeks of medical management. Hence, these cases were taken up for delayed surgery on basis of HRCT findings and nerve excitability test. This was in concurrence with the study done by Ulug et al. [26]. The author here showed that HRCT and electromyography were more important in deciding surgical intervention in cases of traumatic facial paralysis due to late presentation of cases (mostly after 21 days) when ENoG is critical to perform. They also concluded that recovery of facial nerve function could be achieved regardless of timing of surgery performed within the first 3 months of onset of paralysis. Our study also demonstrates the type of injury does not have any clear effect on the facial outcome as long as appropriate surgical management is applied.
Many studies have pointed out that probability of recovery in cases of facial palsy is not optimum with delayed surgery [22, 27]. Our study shows contradictory findings with 6/7 (86%) of patients with delayed surgery showing improvement to HB grade 1–3.
In a retrospective study of 13 patients in a span of 16 years by Quaranta et al. [27], patients underwent late facial decompression with transmastoid extralabyrinthine posterior tympanotomy or middle cranial fossa approach; satisfactory facial function was achieved in 75% of patients. But postoperative hearing outcome was not recorded with these approaches. Popovic et al. [28] in a retrospective analysis of patients treated for traumatic facial paralysis suggested that in surgical cases best recovery is achieved with decompression while nerve anastomosis and nerve graft had similar time course and outcome in the House–Brackmann grades. We preferred modified posterior tympanotomy approach for facial nerve decompression from geniculate ganglion to stylomastoid foramen to preserve hearing as described by Panda et al. [9]. In our study, facial function of House–Brackmann grade 2–3 was achieved in 86% with improved hearing outcome in audiometry in 72% patients treated with surgery.
Conclusion
Onset of facial palsy (immediate or delayed) had no relation to ultimate improvement of facial palsy and even delayed-onset high-grade paralysis can show improvement when treated conservatively. Both HB grading and FEMA grading scales are almost homogenous in distribution and outcome of results, thus, can be recommended for grading the severity of facial nerve paralysis. Patients with incomplete facial palsy are candidates for conservative management. It is justified for the clinician to try conservative management in patients with complete facial paralysis for up to 3 months before any definitive surgical intervention even in cases, where ENoG and NET suggest poor prognosis. There is a high false-positive rate Schirmer’s test in localizing injury site to facial nerve. Patients with incomplete palsy and CHL showed better improvement in both hearing outcome and facial function improvement when compared to those with complete palsy. The presence of sensorineural hearing loss at presentation does not indicate a poor prognosis for recovery.
References
Kerr AG, Smyth GD (1987) Ear trauma. Scott-Brown’s Otolaryngology, 5th edn. Butterworths, London
Jackler RK((1990) Facial, auditory, and vestibular nerve injuries associated with basilar skull fractures. Neurol Surg 3:2305–2316
Brodie HA, Thompson TC (1997) Management of complications from 820 temporal bone fractures. Otol Neurotol 18:188–197
Fisch U (1980) Management of intratemporal facial nerve injuries. JLO 1980 94:129–134
Ulug T, Ulubil SA (2005) Management of facial paralysis in temporal bone fractures: a prospective study analyzing 11 operated fractures. Am J Otol 26:230–238
House JW, Brackmann DE (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93:146
Evans RA, Harries ML, Baguley DM, Moffat DA (1989) Reliability of the House and Brackmann grading system for facial palsy. JLO 103:1045–1046
Kim HN, Lee WS, Yoon PM, Lee HK, Kim DY(1998) Clinical application of the FEMA grading system. New horizons in facial nerve research and facial expression. Kugler, The Hague, pp 533–538
Panda NK, Kaushal D, Verma R (2012) Modified surgical approach in facial palsy: it’s worth a try. Otolaryngol Head Neck Surg 147:P214
Fisch U (1980) Maximal nerve excitability testing vs electroneuronography. Arch Otolaryngol 106:352–357
Xu P, Jin A, Dai B, Li R, Li Y (2017) Surgical timing for facial paralysis after temporal bone trauma. Am J Otol 38:269–271
Darrouzet V, Duclos JY, Liguoro D, Truilhe Y, De Bonfils C, Bebear JP (2001) Management of facial paralysis resulting from temporal bone fractures: our experience in 115 cases. Otolaryngol Head Neck Surg 125:77–84
Turel KE, Sharma NK, Verghese J, Desai S (2005) Post traumatic facial paralysis. Treatment options and strategies. Indian J Neurotrauma 2:33–34
Chang CJ, Cass SP (1999) Management of facial nerve injury due to temporal bone trauma. Am J Otol 20:96–114
Fattah AY, Gurusinghe AD, Gavilan J, Hadlock TA, Marcus JR, Marres H et al (2015) Facial nerve grading instruments: systematic review of the literature and suggestion for uniformity. Plast Reconstr Surg 135:569–579
Thakar A, Gupta MP, Srivastava A, Agrawal D, Kumar A (2018) Nonsurgical treatment for posttraumatic complete facial nerve paralysis. JAMA Otolaryngol Head Neck Surg 144:315–321
Panda NK, Mehra YN, Mann SB, Mehta SK (1991) Post traumatic facial paralysis—a review. JPMA 41:105–107
Hough JV, David Stuart W (1968) Middle ear injuries in skull trauma. Laryngoscope 78:899–937
Brodsky L, Eviatar A, Daniller A (1983) Post-traumatic facial nerve paralysis: three cases of delayed temporal bone exploration with recovery. The Laryngoscope 93:1560–1565
Beck DL, Benecke JE (1993) Electroneurography: electrical evaluation of the facial nerve. J Am Acad Audiol 4:109–115
Grosheva M, Wittekindt C, Guntinas-Lichius O (2008) Prognostic value of electroneurography and electromyography in facial palsy. Laryngoscope 118:394–397
Fisch U (1974) Facial paralysis in fractures of the petrous bone. Laryngoscope 84:2141–2154
Lambert PR, Brackmann DE (1984) Facial paralysis in longitudinal temporal bone fractures: a review of 26 cases. The Laryngoscope 94:1022–1026
Coker NJ, Kendall KA, Jenkins HA, Alford BR (1987) Traumatic infratemporal facial nerve injury: management rationale for preservation of function. Otolaryngol Head Neck Surg 97:262–269
Zayas JO, Feliciano YZ, Hadley CR, Gomez AA, Vidal JA (2011) Temporal bone trauma and the role of multidetector CT in the emergency department. Radiographics 31:1741–1755
Ulug T, Ulubil SA (2005) Management of facial paralysis in temporal bone fractures: a prospective study analyzing 11 operated fractures. Am J Otolaryngol 26:230–238
Quaranta CG, Piazza F, Quaranta N, Salonna I (2001) Facial nerve paralysis in temporal bone fractures: outcomes after late decompression surgery. Actaoto-laryngologica 121:652–655
Popović D, Stanković M, Popović Z, Milisavljević D (2003) Traumatic facial palsy. Facta Univ Med Bio 1:3
Funding
This research received no specific Grant from any funding agency, commercial or not for profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Yadav, S., Panda, N.K., Verma, R. et al. Surgery for post-traumatic facial paralysis: are we overdoing it?. Eur Arch Otorhinolaryngol 275, 2695–2703 (2018). https://doi.org/10.1007/s00405-018-5141-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5141-y