Abstract
Background
Notable differences have been identified between low-resolution manometry (LRM) and high-resolution manometry (HRM) in normative data.
Objective
This study aimed to investigate within-subject differences between unidirectional LRM and circumferential HRM solid-state measurement sensors in the pharyngoesophageal segment during swallowing.
Methods
Ten healthy subjects (mean 26.9 years) were evaluated with both a 2.10 mm unidirectional catheter and a 2.75 mm circumferential catheter, with randomized order of catheter placement. Unidirectional measurements were made in four directions (posterior, anterior, right-lateral, left-lateral). Pressures and durations were analyzed to compare (1) posterior to anterior and lateral recordings and (2) posterior and average-LRM measures (C-LRM) to HRM measures at same anatomical location.
Results
No significant differences were found in any of the measures across the four radial directions. A lower amplitude was measured in C-LRM compared to HRM for pharyngeal sensors (LRM Sensor 1: − 39.7 mmHg; Sensor 2: − 61.4 mmHg). Compared with posterior-LRM, HRM recorded higher UES pressures (− 12.8 mmHg) and longer UES relaxation durations (− 0.31 s).
Conclusion
This exploratory study is the first to compare within-subject pressures between unidirectional LRM and circumferential HRM. Substantial differences in pharyngeal manometric measures were found, particularly with regard to UES function. This is clinically important as manometry is uniquely able to evaluate UES function and clarify differential diagnoses in patients with dysphagia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pharyngeal low-resolution manometry (LRM) typically has unidirectional, posteriorly oriented sensors to record timing and amplitude of pressure during swallowing [1]. Low-resolution manometry is a useful adjunct to clinical evaluations, providing quantitative data regarding pharyngeal and UES functioning at sufficient temporal resolutions and straightforward to interpret by a clinician [2, 3]. One identifiable advantage of unidirectional LRM over modern systems is cost, specially associated to catheter and the limitation on the number of uses of the catheter (e.g., 200 uses for HRM vs unlimited uses for LRM) [4]. There are however limitations worth discussing. While this design appears appropriate for the uniform peristaltic motion seen in the esophagus, researchers have questioned the use of unidirectional measurement in the non-uniform pharyngeal lumen [5]; in addition, prior publications have demonstrated a lack of clinical implementation of LRM in clinical practice, this may be due to limited number of measurement sensors [6]. However, there are still clinical and research users implementing this technique and existing differences in normative data when compared to more modern systems as discussed below.
It has recently been suggested that circumferential sensors may improve manometric measurement by averaging pressure radially, thereby overcoming limitations in unidirectional measurement [5, 7]. Substantial differences have been identified between unidirectional and circumferential sensor recordings in the lower esophageal sphincter [8] suggesting that careful comparison at other levels is indicated. McConnel et al. [9] simultaneously evaluated radial symmetry of the pharynx in healthy volunteers (n = 7) using an LRM catheter with four solid-state measurement sensors oriented at 90° angles. Asymmetry in pharyngeal swallowing was identified, with the greatest asymmetry measured within the UES at rest and at the level of the hypopharynx during saliva swallows. Sears et al. [10] replicated this study in healthy participants (n = 12). With a similar catheter housing four solid-state measurement sensors oriented at 90° angles, radial asymmetry was documented in the distal pharynx, with anterior and posterior pressures (365 ± 29 mmHg) substantially higher than lateral pressures (86 ± 13 mmHg) [10, 11]. This has been considered a consequence of increased catheter diameter, as circumferential sensors result in a catheter width of 6 mm in contrast to 2.1 mm [1].
With advances in the design of circumferential sensors, pediatric HRM catheters are now available at 2.75 mm diameter. Therefore, comparison of unidirectional and circumferential sensors of similar diameter is now feasible. This exploratory study evaluated timing, amplitude, and variability of swallowing pressure by comparing unidirectional-LRM to circumferential-HRM within subjects. Improved understanding of the differences between these two solid-state recording sensors may provide clarification of variability in, and differences between, existing normative data.
Methods
Participants
Ten healthy volunteers (3 females), ages ranging 19–33 years (mean 26.9 years), participated in the study. No volunteer reported a history of dysphagia, or neurological or muscular disorder. Ethical approval was obtained from the University of Canterbury Human Ethics Committee (Ref. HEC 2014/70) and written informed consent was obtained from each volunteer included in the study. Volunteers were recruited based on their response to advertisement of the study; as this was an exploratory study, formal sample size calculations exceeded the scope and convenience sampling was implemented to achieve the desired sample size (n = 10).
Equipment
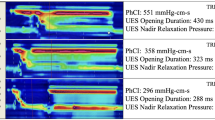
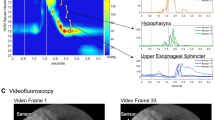
Unidirectional data were collected using a low-resolution manometric catheter as per standard catheter recommendations [1]. Specifically, data were acquired using a catheter 100 cm long and 2.10 mm in diameter, housing 3 solid-state unidirectional, ovoid sensors of approximately 5 mm × 2 mm, with 20 mm spacing between Sensors 1 and 2, and 30 mm between Sensors 2 and 3 (Model CTO/2E-3, Gaeltec, Hackensack, NJ, USA). Manufacturer specifications reports less than ± 2.5 mmHg drift over 18 h of recording (Fig. 1a). The catheter was connected to the Kay Elemetrics Digital Swallowing Workstation (Model 7120, Kay Pentax, Lincoln Park, NJ, USA) with pressure sampled at 250 Hz. Each recording session was preceded by calibration per standard operating instructions. Circumferential data were collected with a high-resolution manometry catheter, using the ManoScan™ HRM system (Model A120) with a data acquisition at 100 Hz using a ManoScan™ ESO catheter (EPS0042). This catheter is 265 mm long, 2.75 mm in diameter and contains 36 circumferential pressure sensors, spaced 7.5 mm apart along its length. Each sensor is 4.0 mm long with 2.0 mm active sensing area and has 16 pressure-sensitive segments distributed circumferentially (Fig. 1b); average circumferential pressures are calculated from these pressure sensing elements at sensor level. Drift over time for this catheter has been reported previously [12, 13]. In vivo calibrations were routinely performed; each recording session was preceded by calibration per standard operation. All recorded studies were corrected, post hoc, with thermal compensation.
Procedure
Each volunteer was seen for two sessions in which they were evaluated with either LRM or HRM. The order of LRM or HRM assessment was randomized, with 5 volunteers having LRM preceding HRM. Topical nasal anesthetic was not applied. The LRM catheter was inserted per standard methods [11, 14]. A pull-through technique was performed in 5-mm increments. This was continued until correct catheter placement was confirmed through visualization of the typical ‘M’ wave at Sensor 3 during swallowing, corresponding to the superior aspect of the high pressure zone of the UES [11]. Posterior orientation of the three sensors was confirmed by monitoring unidirectional markers on the catheter. The catheter was then secured to the nose with medical tape. At final placement, Sensor 1 was located in the proximal pharynx (approximately at the level of the base of tongue), Sensor 2 in the distal pharynx (approximately at the level of the laryngeal aditus) and Sensor 3 in the proximal aspect of the UES. Throughout data collection, evaluation of manometric waveforms by the researcher ensured correct placement was maintained.
Previous research has shown that pharyngeal asymmetry is altered by the presence of a bolus, as the temporary fluid-filled space created from bolus entry into the pharynx can essentially eliminate radial asymmetry [9, 15]. Hence, this study utilized saliva swallows. Each subject was asked to perform five saliva swallows at a self-generated pace, approximately one swallow every minute, to record baseline function. Sips of water were offered as needed to moisten the mouth between trials. Five swallows were completed with sensors in each direction, including posterior, left, anterior, and right (total of 20 swallows). The unidirectional catheter was repositioned by rotating 90° at the level of the nares. Rotational stability has been found robust with standard ovoid catheters [1].
The HRM catheter was placed transnasally using a routine protocol [16]. As HRM catheters contain 36 pressure sensors spaced 0.75 mm apart, a pull-through technique to enable optimal placement was not required. Thus, the catheter was inserted until Sensor 1 was located just inside the naris and Sensor 36 in the cervical esophagus, enabling the length of the upper aerodigestive tract to be evaluated. The insertion depth was recorded for subsequent comparison to LRM catheter placement. Five saliva swallows were completed in the HRM condition.
Data analysis
Data extraction
Depth of insertion was compared between the LRM and HRM catheters to enable direct comparison of measurements, thus, the only sensors analyzed from the HRM system were three sensors that directly corresponded to the three LRM sensors. The beginning and end of each swallow were identified off-line as a substantial increase from baseline and a stable return to baseline, consistent with prior research [7]. The LRM and HRM data and the start- and end-of-swallow annotations were exported for post hoc analysis with customized MATLAB software (MATLAB R2014a, The MathWorks Inc., Natick, MA, 2014).
Measurements
There were two measures extracted from the data for all comparisons:
-
1.
Maximum amplitude (mmHg) at Sensor 1 and Sensor 2, and nadir amplitude at Sensor 3.
-
2.
Durations from onset to offset of the previously marked annotations for Sensors 1 and 2. Peak-to-peak of the characteristic M-wave for Sensor 3 [17].
An additional measure was then calculated to quantify the variability of data between swallowing trials within a radial direction (anterior, posterior, lateral left and right):
-
1.
Mean coefficient of variation (mCV; %) obtained by aligning the waveforms of the five swallows at each direction using the onset annotation point and calculating the CV at each time point of recorded data. The CVs across time were then averaged to obtain a single measure.
Inter-rater reliability
Three independent raters identified the onset and offset of a single randomly selected swallow for each volunteer in each direction. Inter-rater reliability was assessed using a two-way random, absolute agreement, single-measures intra-class correlation coefficient [ICC (2, 1)]. The average ICC and its standard deviation across sensors were calculated for the duration measure. The acceptance criterion was defined a priori as ICC > 0.70. The ICC for the maximum/nadir amplitude measure was not derived as it was generated from automated software (in MATLAB).
Radial symmetry
Comparisons were made across the four measurement directions of LRM comparing conventional posterior (P) to anterior (A), lateral left (LL) and lateral right (LR) directions. A separate analysis was performed for each sensor individually. Linear mixed effects analysis was performed using R [18] and lme4 [19]. Measurement direction was entered into the model as fixed effect and intercept for subject was entered as random effect. Inclusion of the by-subject random slopes for the effect of direction was evaluated for the amplitude and duration measures using a likelihood ratio test. By-subject random slopes inclusion is not possible for the mCV measure as it is a summary measure of the five trials.
P values for the measurement direction were obtained comparing the full model with the measurement direction effect against the model without the measurement direction effect using a likelihood ratio test. When the likelihood ratio test indicated that the full model was appropriate (p < 0.05), the model was further evaluated. The estimate, bootstrap confidence interval using 1000 simulations, and p value of the coefficients for each of the measurement directions were then reported, with the reference category of posterior direction. The posterior orientation was chosen as the reference category as this is the standardized measurement direction for unidirectional solid-state manometry [1].
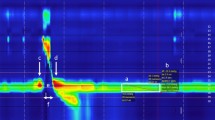
Comparison of unidirectional and circumferential measures
An averaged circumferential measure of the four unidirectional LRM recording directions (C-LRM) was devised and similarly compared to HRM measures of corresponding sensors within each volunteer, as shown in Fig. 2. C-LRM data was obtained by randomly selecting one swallow waveform from each of the directions. The four swallow waveforms (one per direction) were then aligned using the manually selected onset points. The average duration, calculated as the mean duration of the four selected swallows, was used as the end point for subsequent analysis. A point-by-point average was calculated obtaining the C-LRM signal. This process was repeated five times, obtaining five axially averaged C-LRM swallowing pressure traces. All statistical methods were replicated as discussed in previous section. However, comparisons of posterior-LRM and C-LRM were made to standard HRM recordings.
Results
Inter-rater reliability
Inter-rater reliability was acceptable, with measures achieving the a priori standard ICC coefficients (as discussed above) on duration measures for both LRM and HRM. Results revealed a mean ICC for the posterior direction of 0.85 [standard deviation (SD) 0.18], which was similar for the other directions including anterior (mean 0.75, SD 0.21), lateral left (mean 0.84, SD 0.17), lateral right (mean 0.92, SD 0.05) and HRM (mean 0.75, SD 0.06).
Model fitting
Visual inspection of residual plots revealed no deviations from homoscedasticity or normality. By-subject random slopes for the effect of direction was included for duration and amplitude as F-tests of the likelihood ratio were significant for all cases (p < 0.05).
Radial symmetry
Descriptive statistics for the four radial LRM directions are contained in Table 1.
Results from likelihood ratio tests are as follows:
-
1.
For measures of amplitude, there was no significant effect of radial direction across sensors [Sensor 1: χ2 (3) = 3.90, p = 0.27; Sensor 2: χ2 (3) = 7.16, p = 0.07; Sensor 3: χ2 (3) = 4.21, p = 0.24].
-
2.
Duration measurements revealed no significant effect of radial direction for Sensor 2 [χ2 (3) = 4.42, p = 0.22] and Sensor 3 [χ2 (3) = 5.78, p = 0.12] but an effect was found for Sensor 1 [χ2 (3) = 8.52, p = 0.04].
-
3.
Similarly, mCV was not significantly different as a function of radial direction for Sensor 1 [χ2 (3) = 1.6, p = 0.66], Sensor 2 [χ2 (3) = 3.38, p = 0.34], or Sensor 3 [χ2 (3) = 3.76, p = 0.29].
The duration measurement was further evaluated at the level of Sensor 1. When comparing anterior and lateral directions to posterior, there were no significant differences noted for the lateral directions [posterior: 0.55 s (95% CI 0.63, 0.47); lateral left: − 0.01 s (95% CI − 0.05, 0.04), p = 0.86; lateral right: − 0.02 s (95% CI − 0.08, 0.04), p = 0.63]; however, a significant difference was found between anterior and posterior directions, with a lower duration in the anterior direction [− 0.04 s (95% CI − 0.06, − 0.01), p = 0.03].
Comparison of unidirectional and circumferential measures
Descriptive statistics for the C-LRM and HRM recording directions are contained in Table 2.
Results from the likelihood ratio tests are as follows:
-
1.
There was a difference in amplitude measures across recording directions for all sensors [Sensor 1: χ2 (2) = 12.98, p < 0.01; Sensor 2: χ2 (2) = 23.48, p < 0.01; Sensor 3: χ2 (2) = 19.19, p < 0.01].
-
2.
An effect of recording direction for duration was found across all sensors [Sensor 1: χ2 (2) = 8.03, p = 0.02; Sensor 2: χ2 (2) = 11.29, p < 0.01; Sensor 3: χ2 (2) = 8.59, p = 0.01].
Amplitude and duration for all sensors (Tables 3, 4; Fig. 3) were further evaluated. The average and bootstrap confidence interval, for the posterior and C-LRM recording directions as compared to C-HRM are reported below.
Discussion
Despite widespread use of HRM following its development, this is the first study to measure and compare within-subject pressures between unidirectional and circumferential solid-state sensors using an LRM catheter and an HRM catheter, respectively. Comparisons were also made between recording directions (e.g., posterior to anterior and lateral directions), as there is a paucity of data regarding consensus or validation between axial directions, despite the posterior direction being the standard direction of measurement for LRM. We found no significant differences between directional variability across the four radial directions (i.e., mCV). Further, amplitude of pressure across the radial directions showed no significant differences, although there was increased duration for the upper-pharyngeal region. These results conflict with a previous study [7], which reported a higher pressure in the posterior direction. However, this study averaged across sensors to calculate the maximum which may differ from the present sensor-level analysis. Further, as discussed earlier, differences in amplitude measures can also result from different instruments and catheter diameters. For example, McConnel et al. [9] and Sears et al. [10] evaluated radial symmetry using a custom-built LRM catheter with an outer diameter of 3.4 and 4.5 mm, respectively. This increased diameter may exacerbate subtle differences in radial symmetry not identified with the narrow 2.1-mm-diameter catheter used in the present study.
The overall consistency of maximum pressure generation across the four radial directions contrasts with the substantial differences seen between the amplitude of LRM and HRM recordings. While some HRM sensors demonstrated higher amplitudes compared to LRM and C-LRM, Fig. 3 indicates the substantial differences between HRM, C-LRM and conventional posterior-LRM. These differences are reflected in existing normative data [20]. Of particular interest are the differences seen in UES recordings. HRM indicated longer UES relaxation durations and higher amplitudes than LRM in the same subjects. For example, the posterior-LRM Sensor 3 indicated, on average, UES pressures 12.8 mmHg lower than HRM. This is clinically important as manometry is uniquely able to evaluate UES function and clarify differential diagnoses in patients with dysphagia [16, 21, 22].
It is of interest to note that HRM indicates higher pressures than the other recording directions. Furthermore, as HRM indicates averaged pressures from multiple circumferential sensors, such pressures should be lower or equal to the posterior direction, as was seen in our C-LRM values from averages of 4 radial pressures. With the advent of novel technologies, including the three-dimensional HRM catheter, access to individual recording direction data will allow direct simultaneously comparison for each direction to further explore these observed differences in values.
The present study has some limitations. A primary issue is the comparison of measured data across swallows, rather than within a single swallow. This arose from the need for catheter repositioning and thus non-simultaneous data collection in LRM. However, the results from our study were derived from a standard catheter, which facilitates generalization of our results to improved understanding and practical use of this technique. While the low- and high-resolution catheters were of similar diameter, they were not identical at 2.10 and 2.75 mm, respectively. The larger HRM catheter was found to have higher amplitude and longer duration of UES relaxation. This is consistent with research indicating similar changes in swallowing biomechanics which are evident during ingestion of larger boluses, potentially mimicked with the presence of a larger catheter [23]. Yet, it is unclear if the difference of 0.65 mm is substantial enough to have an effect on swallowing biomechanics. Further, posterior orientation of the three sensors was confirmed by monitoring unidirectional markers on the external portion of the catheter and based on prior studies indicating rotational stability [1]. Importantly, however, sensor position and rotation were assumed in the present study and should be evaluated with simultaneous imaging modalities (such as videofluoroscopy or endoscopy) in future research. In addition, the distance along the catheter was used to ensure the pressure location for both the LRM and HRM catheters were the same at rest. However, catheter stiffness may have impacted the amount of catheter movement during swallowing due to palatal elevation, resulting in unaligned sensors at the peak of the swallowing response. Differences in the dimension of sensor recording surface (especially vertical) may have also contributed to the differences found. A study with a larger number of participants and simultaneous imaging instrumentation could further help characterization of differences in manometric recordings and contribute to statistical interpretation of differences between the radial directions.
Conclusion
The key findings reveal that alterations in unidirectional sensor recording direction have minimal effect in measurements of timing and magnitude and variability of pharyngeal pressures. Further, circumferential HRM was found to measure a longer UES relaxation duration and higher amplitudes than posterior-LRM within the same subjects. This is important as manometry is uniquely positioned to evaluate UES function and clarify differential diagnoses in patients with dysphagia. Ongoing research is indicated to further explore these differences and validate the measurements obtained by LRM and HRM in practice.
References
Salassa JR, DeVault KR, McConnel FM (1998) Proposed catheter standards for pharyngeal manofluorography (videomanometry). Dysphagia 13(2):105–110
Olsson R, Castell JA, Castell DO, Ekberg O (1995) Solid-state computerized manometry improves diagnostic yield in pharyngeal dysphagia: simultaneous videoradiography and manometry in dysphagia patients with normal barium swallows. Abdom Imaging 20(3):230–235
Pauloski R, Rademaker A, Lazarus C, Boeckxstaens G (2009) Relationship between manometric and videofluoroscopic measures of swallow function in healthy adults and patients treated for head and neck cancer with various modalities. Dysphagia 292(3):342–351
Pandolfino J (2010) High-resolution manometry: is it better for detecting esophageal disease? Gastroenterol Hepatol (NY) 6(10):632–634
Dodds W, Kahrilas P, Dent J, Hogan W (1987) Considerations about pharyngeal manometry. Dysphagia 214:209–214
Desuter G, Beguin C, Piessevaux H, Goncette L, Van Parijs V, Van den Bergh P (2009) Physiologic variables for videofluoromanometric assessment of dysphagia: an exploratory study. Acta Gastroenterol Belg 72(3):312–320
Rosen SP, Jones CA, Mcculloch TM (2017) Pharyngeal swallowing pressures in the base-of-tongue and hypopharynx regions identified with three-dimensional manometry. Laryngoscope 127(9):1989–1995
Pursnani KG, Oeffner C, Gideon RM, Castell DO (1997) Comparison of lower oesophageal sphincter pressure measurement using circumferential vs unidirectional transducers. Neurogastroenterol Motil 9(3):177–180
McConnel FM, Guffin TN, Cerenko D (1991) The effect of asymmetric pharyngoesophageal pressures on manofluorographic measurements. Laryngoscope 101(5):510–515
Sears VW, Castell JA, Castell DO (1991) Radial and longitudinal asymmetry of human pharyngeal pressures during swallowing. Gastroenterology 101(6):1559–1563
Castell JA, Castell DO (1993) Modern solid state computerized manometry of the pharyngoesophageal segment. Dysphagia 8(3):270–275
Robertson EV, Lee YY, Derakhshan MH, Wirz A, Whiting JRH, Seenan JP, Connolly P, Mccoll KE (2012) High-resolution esophageal manometry: addressing thermal drift of the manoscan system. Neurogastroenterol Motil 24(1):61–64
Lamvik K, Guiu Hernandez E, Jones R, Huckabee M-L (2016) Characterization and correction of pressure drift in the ManoScan TM high-resolution manometry system: in vitro and in vivo. Neurogastroenterol Motil 28(5):732–742
Huckabee M-L, Lamvik K, Jones R (2014) Pharyngeal mis-sequencing in dysphagia: characteristics, rehabilitative response, and etiological speculation. J Neurol Sci 343(1–2):153–158
Brasseur J, Dodds W (1991) Interpretation of intraluminal manometric measurements in terms of swallowing mechanics. Dysphagia 6(2):100–119
Knigge MA, Thibeault S, Mcculloch TM (2014) Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia 29(1):2–16
Lamvik K, Jones R, Sauer S, Erfmann K, Huckabee M-L (2015) The capacity for volitional control of pharyngeal swallowing in healthy adults. Physiol Behav 152(Pt A):257–263
R Foundation for Statistical Computing (2017) R: a language and environment for statistical computing. Vienna, Austria
Bates D, Mächler M, Bolker BM, Walker SC (2015) Fitting linear mixed-effects models using lme4. J Stat Softw 2015:67
Takasaki K, Umeki H, Enatsu K, Tanaka F, Sakihama N, Kumagami H, Takahashi H (2008) Investigation of pharyngeal swallowing function using high-resolution manometry. Laryngoscope 118(10):1729–1732
Jones CA, Hammer MJ, Hoffman MR, Mcculloch TM (2014) Quantifying contributions of the cricopharyngeus to upper esophageal sphincter pressure changes by means of intramuscular electromyography and high-resolution manometry. Ann Otol Rhinol Laryngol 123(3):174–182
Hammer MJ, Jones CA, Mielens JD, Kim CH, Mcculloch TM (2014) Evaluating the tongue-hold maneuver using high-resolution manometry and electromyography. Dysphagia 29(5):564–570
Kahrilas PJ, Logemann J, Krugler C, Flanagan E (1991) Volitional augmentation of upper esophageal sphincter opening during swallowing. Am J Physiol 260(3 Pt 1):G450–G456
Acknowledgements
The authors thank Kerstin Erfmann and Katharina Winiker for their collaboration in data collection and inter-rater reliability. The authors acknowledge the Canterbury Medical Research Foundation for its support of this research. EGH provided technical expertise in MATLAB software program and KG conducted the studies. All authors contributed to the research study design, analysis, and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Guiu Hernandez, E., Gozdzikowska, K., Jones, R. et al. Comparison of unidirectional and circumferential manometric measures within the pharyngoesophageal segment: an exploratory study. Eur Arch Otorhinolaryngol 275, 2303–2310 (2018). https://doi.org/10.1007/s00405-018-5019-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-5019-z