Abstract
Purpose
To improve the diagnoses of the salivary gland tumors, a dynamic-enhanced MRI (dMRI) was investigated.
Methods
We conducted a retrospective chart review of 93 cases of salivary gland tumors. The histological diagnoses were obtained from all patients using a surgical specimen and/or an open biopsy specimen. The dMRI as well as fine-needle aspiration cytology (FNAC) and intraoperative frozen section (IFS) were analyzed. This study focused on the time-intensity curve (TIC) after injection, peak time (Tpeak), washout ratio (WR) as well as the gradient of enhancement and washout profile.
Results
The histological diagnoses included pleomorphic adenoma (PMA) in 53 cases, the Warthin tumors (WT) in 14 cases and malignant tumors (MT) in 26 cases. Incorrect diagnosis rate of FNAC and IFS were 5.2 and 8.3%, respectively. The TIC revealed differences among the three types of tumors. Tpeak as well as WR also revealed significant differences (p < 0.001). Tpeak were lower in order of WT, MT, PMA, respectively. WR of TICs at 30, 45 and 105 s after Tpeak were higher in order of WT, MT, PMA, respectively (p < 0.001). The gradient of increment and washout in the TIC curve was also an important parameter to distinguish the three types of tumors. In MT, the rapid enhancement pattern was found in high or intermediate histological grade tumors, whereas the slow enhancement pattern was exhibited in low grade tumors.
Conclusions
Our findings indicate that using Tpeak and WR, it is possible to distinguish between WT, PMA and MT. Additionally, a rapid enhancement pattern may be a potential marker for these tumors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Salivary gland tumors (SGTs) are approximately 3–6% of all head and neck tumors and the annual incidence throughout the world ranges from 0.05 to 2 cases per 100,000 individuals [1]. Pleomorphic adenoma (PMA) and Warthin’s tumors (WT) are the most common SGTs among benign tumors [2]. SGTs are classified into 22 different histological types among the malignant tumors (MT) [3].
Surgery is standard treatment for SGTs, however, the surgical procedures of these tumors varies. Complete extirpation is needed not only for MT but also for PMAs due to their malignant transformation potential and recurrence. WTs, on the other hand, have a low incidence of malignant transformation allowing for enucleation or conservative management of the tumor [4, 5]. The surgical treatment strategy for the extirpation of MT and PMA depends on the histological grade and histology of the particular tumor. The facial nerve or its branches are often sacrificed at surgery in high-grade MT, but, can be preserved in cases of low-grade MT as well as in PMAs.
Accurate diagnosis of the type of SGT is important in the creation of a surgical plan. These tumors are usually diagnosed synthetically by the mixture of clinical course, physical findings, imaging and cytological examination. Fine-needle aspiration cytology (FNAC) is useful for diagnosis of these tumors [6, 7], however, false positives and false negatives of MTs can be a problem due to their complicated pathologies [7, 8].
Recently, advanced MRI techniques such as diffusion-weighted MR imaging (DWI), apparent diffusion coefficient (ADC) [9, 10] and dynamic-enhanced MRI (dMRI) [8, 9] have been shown to be effective for the diagnosis of SGTs. A dMRI can estimate the histological diagnosis by time-intensity curve (TIC), however, the efficacy of dMRI for diagnosis of parotid tumors is still unclear [11, 12] and needs further investigation. Here, we analyzed the role of dMRI for pretreatment diagnosis of SGTs retrospectively as well as via a review of recent literature.
Materials and methods
Subjects
We conducted a retrospective chart review of 93 cases of SGTs which underwent a dMRI before treatment at the Tohoku University Hospital. The Institutional Review Board has approved this study [Approved no. 2016-1-754 (Tohoku University Graduate School of Medicine)]. The procedures followed were in accord with the Helsinki Declaration. The histopathological diagnoses were obtained from all patients using a surgical specimen and/or an open biopsy specimen. Histologically, there were 53 PMAs, 14 WTs and 26 MTs (six mucoepidermoid carcinomas, three carcinomas ex pleomorphic adenoma, two squamous cell carcinomas, four salivary duct carcinomas, two malignant lymphomas, two adenocarcinomas, one basal celladenocarcinoma, one epithelial–myoepithelial carcinoma, one true carcinosarcoma, one acinic cell carcinoma, one myoepithelial carcinoma, and two metastatic carcinomas). Neither recurrent nor secondary tumors were observed in the study group. High, intermediate and low-grade MTs were diagnosed by previous criteria [1, 3].
MRI technique
MR examinations were performed using a 1.5 T MR imager (Signa Horizon LX CVi; GE Medical Systems, Milwaukee, WI, USA) with either quadrature head neck vascular or surface coil. Postcontrast transverse T1-weighted images (TR/TE/number of signal acquisitions 460–646 ms/12–15 ms/1) were obtained using a spin-echo sequence with a scanning delay time of 133–189 s after dynamic study, field of view (FOV) 210 mm, slice thickness 5 mm, slice gap 1 mm, and acquisition matrix size 320 × 256. For dynamic contrast-enhanced studies, transverse T1-weighted images (TR/TE/number of signal acquisition 135 msec/8 msec/1) were obtained using a turbo spin-echo sequence, FOV 280 mm, slice thickness 5 mm, slice gap 1 mm, and acquisition matrix size of 256 × 128. Gadolinium (Magnevist; Bayer Health Care, Osaka, Japan) was injected intravenously at a dose of 0.2 mL/kg body weight. In each patient, eight scans were obtained at an interval of 15 s. MR images were sequentially obtained 0, 15, 30, 45, 60, 75, 90, and 105 s after contrast medium injection initiation. Gd-DTPA was administered at the beginning of the first scan and is designated as time 0. One (or Two) author(s) (M. S. and T. M.) manually drew regions of interest (ROIs) to avoid the vessels and cystic parts of the tumors, in reference to contrast-enhanced transverse T1-weighted images. We plotted the signal intensity within the ROI against time, and TICs were constructed by modified increment ratios where \(({\text{IR}})=\frac{{(({\text{signal}}\;{\text{intensity}}) - ({\text{pre-enhancement}}\;{\text{signal}}\;{\text{intensity}}))~ \times ~100}}{{{\text{pre-enhancement}}\;{\text{signal}}\;{\text{intensity}}}}\) as has been reported previously [13].
MR factor analysis
MR images were interpreted retrospectively by three readers T. M., M. S. and I. K. before histological diagnoses. Based on the TICs, the MR factor analysis such as the time to peak enhancement (Tpeak) and the washout ratio (WR) (%):
were analyzed.
The gradient of IR and WR in TIC curve was also analyzed as a role of parameter to divide three types of tumors at 15 s after injection or peak time. The rapid enhancement was defined when
was more than 100. WR15s was calculated by the following formula;
WR15s was also divided as rapid (more than + 10%), plateau (− 10 to + 10%) and negative (peak time was 105 s).
These dMRI factors as well as FNAC and IFS were compared among PMA, WT, low- and high-grade MT.
Statistical analysis
We used the Kruskal–Wallis rank sum test to compare continuous variates among three groups, adding the Holm test as post hoc analysis. To quantify the accuracy of diagnosis, we drew the receiver operator characteristic (ROC) curve, in which we defined cut-off values by Youden index. We also calculated positive predictive value (PPV), negative predictive value (NPV), and accuracy with the above cut-off values. A p value < 0.05 was considered significant, and all tests were two tailed. All statistical analyses were performed with R for Windows (version 2.0-3) and EZR (version 1.36) [14].
Result
Patient characteristics
Patient characteristics were shown in Table 1. The cases included 43 males and 50 females, aged from 16 to 89 years (median age 63 years). The histological diagnoses included PMA in 53 cases, WT in 14 cases and MT in 26 cases. Most PMA and WT patients were in the 0s, while MT patients were in their 70 s.
Accuracy of FNAC and IFS
FNAC was performed in 77 cases (Table 2). Among them, insufficient materials were found in seven cases. One case of PMA was diagnosed as adenoid cystic carcinoma and three cases of MT (acinic cell carcinoma, low-grade mucoepidermoid carcinoma and diffuse large B cell lymphoma) were diagnosed as benign by FNAC. IFS was performed in 48 cases (Table 2). Among them, four cases of MT (low-grade mucoepidermoid carcinoma, low grade basal cell adenocarcinoma, epithelial–myoepithelial carcinoma and true carcinosarcoma) were diagnosed as benign tumors. As such, prior to any histological examination, the incorrect diagnosis rate of FNAC and IFS, with respect to malignancy, was 5.2 and 8.3%, respectively.
Dynamic-enhanced MRI analysis
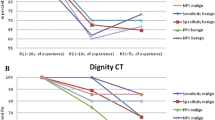
Dynamic-enhanced MRI was performed in all 93 cases. The representative cases with MT, PMA and WT are shown in Fig. 1. TIC patterns were different between solid and cystic parts of the same salivary duct carcinoma (Fig. 1a), thus, for diagnosis, cystic and vessel parts were excluded by drawing ROIs as indicated on the contrast-enhanced transverse T1-weighted images. The raw TICs of all cases are shown in Fig. 2. The TICs presented characteristic findings according to histologic type. IR at 15, 45, 75 and 105 s revealed differences between each histologic type as well. Tpeak was lower in order of PMA (median 105 s, mean 96.2 ± 14.5 s), MT (median 45 s, mean 51.4 ± 30.5 s) and WT (median 21.4 s, mean 15 ± 7.7 s), with statistical significance (p < 0.001) (Fig. 3a and supplementary Fig. 1). ROC curve of each histologic type by peak time was also shown in Fig. 3. Area under the curve (AUC) of MT, PMA and WT were 0.739, 0.925 and 0.939, respectively. Cut-off value by peak time was calculated with 75 s for MT (sensitivity 80.8, specificity 67.2%, PPV 48.8%, NPV 90.0%, accuracy 71.0%), 60 s for PMA (sensitivity 100%, specificity 72.5%, PPV 82.8%, NPV 100%, accuracy 88.8%) and 30 s for WT (sensitivity 100%, specificity 86.1%, PPV 56.0%, NPV 100%, accuracy 88.2%), respectively. WR at 30, 45 and 105 s after peak were ranked from high to low in the order WT, MT and PMA with a statistically significant difference (p < 0.001) (Fig. 4 and supplementary Fig. 2). The ROC curve of each histologic type by washout ratio at 45 s after peak time is shown in Fig. 4. The 45 s mark was chosen because the washout ratio after Tpeak exhibited the lowest p value (p = 1.03 × 10−13). The AUC of MT, PMA and WT were 0.661, 0.88 and 0.976, respectively. Cut-off value by WR was calculated with 5.4% for MT (sensitivity 69.2%, specificity 73.1%, PPV 48.6%, NPV 85.7%, accuracy 71.0%), 4.3% for PMA (sensitivity 92.5%, specificity 80%, PPV 85.7%, NPV 86.5%, accuracy 86.0%) and 11.1% for WT (sensitivity 100%, specificity 86.1%, PPV 56.0%, NPV 100%, accuracy 88.2%).
MRI images and TICs of SGTs. a Salivary duct carcinoma (SDC), asterisks indicate tumor. Four ROIs (#1, 3, 4 and 5) in TIC indicated the typical MT patterns while only one ROI (#2) of the cystic component indicated no enhancement. b PMA, c WT. Asterisks indicate tumor. ROIs of normal gland (#2) were not shown
We observed that the TIC divided into six patterns of enhancement and washout. Of the six patterns observed, three patterns emerged as predictors of tumor type, shown in Table 3. 10 of the 14 WTs (71.4%) showed rapid enhancement—rapid washout. 48 of 53 PMAs (90.6%) showed the slow enhancement—plateau or negative washout pattern (Fig. 5). For MTs, rapid or slow enhancement—plateau washout pattern in 18 of the 26 cases (69.3%). Table 4 showed the enhancement pattern among histological grade of MTs. Rapid enhancement showed in 2 cases (33.3%) of low grade MTs, 3 cases (75%) of intermediate and 12 cases (75%) of high-grade MTs. Slow enhancement observed in four cases (66.7%) of low-grade MTs, one case (25%) of intermediate and three cases (25%) of high-grade MTs (p = 0.252).
Literature review
The sensitivity, specificity, PPV, NPV and accuracy of dMRI from the previous literature are summarized in Table 5. Accuracy was higher in order of WT (91.4–97.9%), MT (81.3–97.7%) and PMA (77.4–93%).
Discussion
Pretreatment diagnosis of SGTs can be difficult. FNAC is considered the gold standard for the diagnosis of SGTs with an overall accuracy of 95%, however, false negatives of MTs [7] and false positive of PMA [7] and WT [8] sometimes occur. In this study, in the absence of any histological analysis, the incorrect diagnosis rate of FNAC was 5.2% where one case of PMA without malignant transformation was diagnosed as adenoid cystic carcinoma as diagnosed by FNAC and three cases consisted of acinic cell carcinoma, low-grade mucoepidermoid carcinoma and diffuse large B cell lymphoma diagnosed as class I or II (benign tumors) by FNAC.
It has been previously reported that, using conventional MRI techniques, it is possible to distinguish malignant from benign tumors. For example, tumors with well-defined borders tend to be benign as is the case for PMAs and WTs [24]. In addition, high signal intensity on T2-weighted images are typical of PMAs [25], whereas low signal intensity is a sign of malignancy [25]. However, because low T2 signal intensity is also present with WTs, determination of tumor type can remain uncertain [26]. Using dMRI results, Hisatomi et al. have reported characteristic TIC patterns of SGTs [27, 28]. Their research indicates that rapid increase, low Tpeak, and high WR are recognized as a characteristic pattern of WTs and high Tpeak with low WR as a characteristic pattern of PMAs. Asseli et al. also examined the efficacy of dMRI for pretreatment diagnoses from the previous literature [19] and despite the use of several different cut-off values, Tpeak and WR were shown to also be useful parameters to distinguish various SGTs.
In this study, using the TIC of dMRI, a histologically specific pattern emerged. Of the total six enhancement/washout patterns observed, three patterns were determined to be predictors of SGT type. In addition, by examining the AUC of Tpeak and the WR, unique cut-off values for MT and PMA were observed. Unfortunately, these cut-off values were too close to each other to be useful. Previous data as well as this study have shown that WTs are likely the best candidate for the use of dMRI since it has the highest accuracy among three histological types. In fact, the WT pattern was clearly highlighted with a Tpeak < 105 s and WR ≥ 30% in this study giving it an accuracy of 91.4%. To distinguish MT from PMA, this study indicated that a rapid enhancement pattern along with Tpeak and WR values could be potential markers. It should be noted that the enhancement pattern depends on the histological grade of MTs, with slow enhancement in low-grade MTs and rapid enhancement in intermediate and high-grade MTs. These results seem to be helpful in that high-grade MT can be distinguished from low-grade MT/PMA from the viewpoint of facial nerve preservation and WT can be distinguished from the other SGT for observational strategies. It has been reported that Tpeak correlates closely with tumor vascularity and the washout ratio accurately reflected the cellularity-stromal grade [16], as such, rapid enhancement as well as short Tpeak may be influenced by high tumor vascularity.
According to the literature review, accuracy was higher in the order of WT (91.4–97.9%), MT (81.3–97.7%) and PMA (77.4–93%). Our study also followed this same order of accuracy. Furthermore, since it is reported that addition of the ADC value to the Tpeak leads to improved differentiation of MT from PMA [9, 23], especially with new diagnostic algorithms [12] and a multiparametric approach based on a combination of parameters [29], ADC and dMRI could become a future screening method.
Since this was a limited retrospective study, a prospective study is, therefore, considered to be necessary to further validate our hypothesis and that more patients should be enrolled to obtain a stronger statistical significance for these results.
Conclusion
Our results indicate that dMRI can be a useful quantitative preoperative tool in the treatment of salivary gland tumors, especially WTs. To distinguish MT from PMA, this study indicates that a rapid enhancement pattern as well as Tpeak and WR could be potential markers for these tumors.
References
Guzzo M, Locati LD, Prott FJ, Gatta G, McGurk M, Licitra L (2010) Major and minor salivary gland tumors. Crit Rev Oncol Hematol 74:134–138
Lin CC, Tsai MH, Huang CC, Hua CH, Tseng HC, Huang ST (2008) Parotid tumors: a 10-year experience. Am J Otolaryngol 29:94–100
Brandwein-Gensier M, Bell D, Inagaki H et al (2017) Tumours of salivary glands. In: El-Naggar AK, Chan JK, Grandis JR, Takata T, Slootweg PJ (eds) WHO classification of head and neck tumours, 4th edn. IARC, Lyon, pp 160–202
Reddy VM, Thangarajah T, Castellanos-Arango F, Panarese A (2008) Conservative management of Warthin tumour. J Otolaryngol Head Neck Surg 37:744–749
Teymoortash A, Werner JA (2005) Tissue that has lost its track: Warthin’s tumour. Virchows Arch 446:585–588
Veder LL, Kerrebijn JD, Smedts FM, den Bakker MA (2010) Diagnostic accuracy of fine-needle aspiration cytology in Warthin tumors. Head Neck 32:1635–1640
Gudmundsson JK, Ajan A, Abtahi J (2016) The accuracy of fine-needle aspiration cytology for diagnosis of parotid gland masses: a clinicopathological study of 114 patients. J Appl Oral Sci 24:561–567
Ogawa T, Suzuki T, Sakamoto M et al (2012) Correct diagnosis of Warthin tumor in the parotid gland with dynamic MRI. Tohoku J Exp Med 227:53–57
Yabuuchi H, Fukuya T, Tajima T, Hachitanda Y, Tomita K, Koga M (2008) Parotid gland tumors: can addition of diffusion-weighted mr imaging to dynamic contrast enhanced MR imaging improve diagnostic accuracy in characterization? Radiology 249:909–916
Yuan Y, Tang W, Tao X (2016) Parotid gland lesions: separate and combined diagnostic value of conventional MRI, diffusion-weighted imaging and dynamic contrast-enhanced MRI. Br J Radiol 89(1060):20150912
Stefanovic X, Al Tabaa Y, Gascou G et al (2017) Magnetic resonance imaging of parotid gland tumors: dynamic contrast-enhanced sequence evaluation. J Comput Assist Tomogr 41:541–546
Mikaszewski B, Markiet K, Smugała A, Stodulski D, Szurowska E, Stankiewicz C (2017) Diffusion- and perfusion-weighted magnetic resonance imaging—an alternative to fine needle biopsy or only an adjunct test in preoperative differential diagnostics of malignant and benign parotid tumors? J Oral Maxillofac Surg 75:2248–2253
Eida S, Ohki M, Sumi M, Yamada T, Nakamura T (2008) MR factor analysis: improved technology for the assessment of 2D dynamic structures of benign and malignant salivary gland tumors. J Magn Reson Imaging 27:1256–1262
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl 48:452–458
Wang J, Takashima S, Takayama F et al (2001) Head and neck lesions: characterization with diffusion-weighted echoplanar MR imaging. Radiology 220:621–630
Yabuuchi H, Fukuya T, Tajima T, Hachitanda Y, Tomita K, Koga M (2003) Salivary gland tumors: diagnostic value of gadolinium-enhanced dynamic MR imaging with histopathologic correlation. Radiology 226:345–354
Eida S, Sumi M, Sakihama N, Takahashi H, Nakamura T (2007) Apparent diffusion coefficient mapping of salivary gland tumors: prediction of the benignancy and malignancy. Am J Neuroradiol 28:116–121
Eida S, Sumi M, Nakamura T (2010) Multiparametric magnetic resonance imaging for the differentiation between benign and malignant salivary gland tumors. J Magn Reson Imaging 31:673–679
Assili S, Fathi KA, Aghaghazvini L, Saligheh RHR, Pirayesh IJ (2015) Dynamic contrast magnetic resonance imaging (DCE-MRI) and diffusion weighted MR imaging (DWI) for differentiation between benign and malignant salivary gland tumors. J Biomed Phys Eng 5:157–168
Hisatomi M, Asaumi J, Yanagi Y et al (2007) Diagnostic value of dynamic contrast-enhanced MRI in the salivary gland tumors. Oral Oncol 43:940–947
Aghaghazvini L, Salahshour F, Yazdani N et al (2015) Dynamic contrast-enhanced MRI for differentiation of major salivary glands neoplasms, a 3-T MRI study. Dentomaxillofac Radiol 44:20140166
Lam PD, Kuribayashi A, Imaizumi A et al (2015) Differentiating benign and malignant salivary gland tumours: diagnostic criteria and the accuracy of dynamic contrast-enhanced MRI with high temporal resolution. Br J Radiol 88(1049):20140685
Tao X, Yang G, Wang P et al (2017) The value of combining conventional, diffusion-weighted and dynamic contrast-enhanced MR imaging for the diagnosis of parotid gland tumours. Dentomaxillofac Radiol 46:20160434
Thoeny HC (2007) Imaging of salivary gland tumours. Cancer Imaging 7:52–62
Christe A, Waldherr C, Hallett R, Zbaeren P, Thoeny H (2011) MR imaging of parotid tumors: typical lesion characteristics in MR imaging improve discrimination between benign and malignant disease. Am J Neuroradiol 32:1202–1207
Okahara M, Kiyosue H, Hori Y, Matsumoto A, Mori H, Yokoyama S (2003) Parotid tumors: MR imaging with pathological correlation. Eur Radiol 13(Suppl 4):L25–L33
Hisatomi M, Asaumi J, Konouchi H, Yanagi Y, Matsuzaki H, Kishi K (2002) Assessment of dynamic MRI of Warthin’s tumors arising as multiple lesions in the parotid glands. Oral Oncol 38:369–372
Hisatomi M, Asaumi J, Yanagi Y et al (2003) Assessment of pleomorphic adenomas using MRI and dynamic contrast enhanced MRI. Oral Oncol 39:574–579
Patella F, Franceschelli G, Petrillo M et al (2018) A multiparametric analysis combining DCE-MRI- and IVIM -derived parameters to improve differentiation of parotid tumors: a pilot study. Future Oncol. https://doi.org/10.2217/fon-2017-0655
Acknowledgements
We are grateful to Miles Kuperus for editorial work in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study. The Institutional Review Board has approved this study [Approved no. 2016-1-754 (Tohoku University Graduate School of Medicine)].
Electronic supplementary material
Below is the link to the electronic supplementary material.
405_2018_4965_MOESM1_ESM.pptx
Supplementary material 1 Supplementary fig. 1: The box and whisker plot of TICs. a: 15 sec, b: 45 sec, c: 75 sec, d:105 sec. Maximum number, 25% percentile, median, 75% percentile and minimum number were shown in box and whisker plot. *: p<0.01, * *: p<0.05. Supplementary fig. 2: WR of TICs. a: 30 sec, b: 45 sec, c: 105 sec after Tpeak. *: p<0.001 (PPTX 119 KB)
Rights and permissions
About this article
Cite this article
Ogawa, T., Kojima, I., Ishii, R. et al. Clinical utility of dynamic-enhanced MRI in salivary gland tumors: retrospective study and literature review. Eur Arch Otorhinolaryngol 275, 1613–1621 (2018). https://doi.org/10.1007/s00405-018-4965-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4965-9