Abstract
Objective
To investigate the voice quality impairments in patients with laryngopharyngeal reflux (LPR) according to the gender.
Design
Controlled multi-center study.
Materials and methods
80 LPR patients (40 males and 40 females) with reflux finding score (RFS) > 7 and reflux symptom index (RSI) > 13 were included and clinically compared according to gender. To be considered as LPR patients, subjects responded to an empiric therapeutic trial based on pantoprazole intake and diet recommendations for 3 months or had positive pH/Impedance metry. Voice Handicap Index (VHI); Short Form Healthy Survey 36 (SF36), blinded Grade, Roughness, Breathiness, Asthenia, Strain and Instability (GRBASI); aerodynamic and acoustic measurements were assessed in all patients and compared with 80 healthy controls (40 males and 40 females) according to gender.
Results
The most common reasons for the consultation were, respectively, globus sensation in males (22.5%) and dysphonia (27.5%) in female who complained more of breathing difficulties and choking episodes related to LPR than males (p = 0.024). From a quality of life standpoint, female had increased significant impact of LPR disease on vitality and mental health than male. Compared to healthy subjects, both LPR male and female patients had stronger values of G, R, B, S, I, VHI, percent jitter, percent shimmer, and soft palate index than controls. In addition, LPR female had stronger values of lowest fundamental frequency and all aerodynamic measurements than controls.
Conclusion
As showed in many other laryngeal conditions, voice quality of female could be more impaired by LPR than male. Some anatomical, histological and functional factors can be suspected and need additional future researches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laryngopharyngeal reflux (LPR) is an inflammatory condition that is defined as the back flow of gastric contents into the laryngopharynx, where these contents come in contact with the tissues of the upper aerodigestive tract [1]. According to some clinical studies, LPR affects 4–30% of outpatients visiting ear, nose, and throat (ENT) departments and up to 50% of patients in voice centers [2, 3]. Hoarseness seems to be a common symptom found in 71–79% of patients [4, 5] and can typically affect patient communication and quality of life [6]. Despite increasing interest in LPR over the past three decades, only a few publications have studied the occurrence of dysphonia in LPR disease. Hence, there have been only 25 trials that discussed dysphonia in LPR disease, and among these, only five controlled studies that compared healthy subjects with LPR patients reported mixed results and unclear conclusions [7,8,9,10,11].
Reflux of the gastric content into the laryngeal mucosa is known to be associated with the development of chronic laryngitis and dysphonia. Many mechanisms explaining dysphonia related to LPR have been proposed and include microtraumas and alterations of both Reinke’s space as well as lubrication of the free edge of the vocal folds. The mucosa alterations of the vocal folds related to LPR may increase the risk for developing benign lesions of the vocal folds, including nodules, polyps, contact laryngeal ulcers, granulomas, or pseudosulcus [12, 13]. Many reports have found that these lesions are more prevalent in females than males, also contributing to the fact that females make more frequent voice center visits than males [14,15,16]. However, a recent paper supported that the easier onset of voice disorders in females could be a result of anatomical, histological, and physiological gender differences that lead to a high susceptibility of developing microtraumas and some vocal fold tissue alterations [17].
The purpose of this study is to investigate clinical complaints, laryngeal findings, and voice quality impairments in patients with LPR disease according to gender and with regard to our data as well as to explore whether females have more severe LPR dysphonia and quality of life impairments than males.
Materials and methods
Ethical considerations
This study was approved by the local ethics committee (ref.2015/99-B707201524621).
Subject recruitment and clinical evaluations
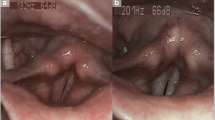
From September 2013 to April 2016, we prospectively recruited 122 outpatients with LPR-related symptoms in the ENT Departments of both EpiCURA Hospitals and Liege University Hospital. The suspicion of a LPR diagnosis was based on the utilization of Reflux Symptom Index (RSI) > 13 and Reflux Finding Score (RFS) > 7 [18,19,20]. RFS was evaluated using videolaryngostroboscopy (StrobeLED-CLL-S1, Olympus Corporation, Hamburg, Germany) at 0, 3, and 6 months in a blind manner regarding patient complaints (RSI). Because hoarseness can be related to many other conditions [21] and because of the lack of a gold standard for its diagnosis, subjects with the following cofactors were excluded to obtain the purest population of LPR patients: neurological disease affecting the voice, psychiatric illness, upper respiratory tract infections within the last month, antacid treatment already started (i.e., proton pump inhibitor(s) (PPI(s)), gastroprokinetic, or antihistamine), previous history of cervical surgery or radiotherapy, laryngeal trauma, vocal fold paralysis/paresis, benign vocal fold lesions, pharyngolaryngeal malignancy, seasonal allergies, chronic obstructive pulmonary disease, PPI hypersensitivity, untreated thyroid disease, prior antireflux surgery, or chemical exposure causing laryngitis. Moreover, active smokers, alcoholics and pregnant and lactating women were also excluded regarding the risk of laryngopharyngeal complaints [22, 23]. Regarding the aerodynamic assessments, we also calculated the Tiffeneau Index for each patient to exclude asthma. Patients with inhaled corticosteroids were also excluded. According to the American recommendations [24, 25] and with regard to our inclusion and exclusion criteria, to be considered LPR patients, subjects had to be cured (RSI < 13 and RFS < 7) after 3 or 6-month treatments of twice-daily proton pump inhibitors (PPIs) as well as diet and behavioral changes. Only resistant patients received additional examinations, i.e., esophagoduodenoscopy and/or pH/impedance measurements, to be defined as LPR patients. We did not systematically use pH/impedance monitoring for the LPR diagnosis at baseline because it is expensive and inconvenient for the patient. To improve patient care, we used a clinically validated protocol [24, 25] for the management of LPR patients (Fig. 1). In addition, to identify direct or indirect signs of laryngitis associated with dysphonia, we analyzed the relationship between the symptoms and signs in each LPR group according to gender.
Flow chart describing the algorithm for assessment and management of patients and the recruitment of healthy subjects. Patients with LPR symptoms (RSI > 13) and signs (RFS > 7) were recruited and assessed at baseline and treated by PPIs and diet advices during 3–6 months. Patients with RSI ≤ 13 and RFS ≤ 7 were considered as responder and LPR patients. Non-responder benefited from additional examinations (i.e., esogastroduodenoscopy, pH metry and manometry) to confirm the LPR diagnosis. Both LPR and healthy subjects were compared on voice quality assessments
80 healthy subjects matched for gender and age were recruited for the control groups. Each subject received an ENT examination and filled out RSI, which was less than 13. They were not assessed for RFS. Naturally, healthy subjects were included after the same exclusion criteria evaluation as that for LPR patients.
Subjective voice assessments
Because there are substantial physiological differences between males and females, particularly regarding the normative acoustic measurement values [26, 27] and perceptual voice quality [28], subjective and objective voice quality analyses were performed separately for each gender using the control group. Patients and controls completed the French version of the Voice Handicap Index (VHI) [29]. A perceptual voice evaluation [Grade, Roughness, Breathiness, Asthenia, Strain and Instability (GRBASI scale)] of subjects was performed by two experienced laryngologists (> 15 years of experience) who were blinded concerning the subject’s state. There were good intra- and interrater reliabilities between the two laryngologists. Moreover, to study the impact of LPR on overall quality of life according to gender, LPR patients completed the French version of Short Term Health Survey 36 (SF-36) [30].
Aerodynamic and acoustic measurements
Maximum phonation time (MPT) and phonatory quotient (PQ) were measured using a calibrated spirometer, taking into account the age, sex, height, and ethnicity of the subject (Spiro-USB100; Medical Electronic Construction, Brussels, Belgium) [31].
To measure the acoustic parameters, subjects were asked to produce the /a/ vowel sound three times at a comfortable pitch and intensity, holding the utterance as long as possible. Both in LPR patients and healthy subjects, voice recordings were performed by the same practitioner during the consultation in a sound-treated room with a high-quality microphone (Sony PCM-D50; NY, USA) placed at a distance of 30 cm from the patient’s mouth. The following acoustic parameters were measured over the entire signal using MDVP® software (KayPentax®, Montvale, NJ, USA): Mean fundamental frequency (MF0), Lowest F0 (Flo), Highest F0 (Fhi), Jitter percent (Jitt), Shimmer percent (Shim), Noise Harmonic Ratio (NHR), Voice Turbulence Index (VTI), and Soft Phonation Index (SPI).
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences for Windows (SPSS v22.0; IBM Corp., NY, USA). To compare various items according to group, the Mann–Whitney test was used. A correlation study between symptoms and signs in each gender group was conducted using Spearman’s correlation test. The evolution of RSI and RFS along the treatment was assessed with Wilcoxon test. A level of significance of 0.05 was adopted.
Results
From the 122 recruited patients, a total of 80 completed the study (40F, 40M) and 42 were excluded for the following reasons: aerodigestive tract infections during the last month before the posttreatment consultation (N = 10); absence from the medical appointment 3 months after treatment initiation (N = 27); negative results from an additional examination (not confirming LPR diagnosis) (N = 2), stopping treatment during the treatment period (N = 1), diagnosis of illness(es) associated with dysphonia during treatment (N = 1), and intake of neuroleptics during the last month (N = 1). Fifty-nine patients were cured after the treatment period, and 21 were considered to be LPR resistant patients (10 females, 11 males) according to additional examinations. There were 40 females (50%) and 40 males (50%), with median ages of 55.0 [standard deviation (SD) = 16.4] and 47.58 (SD = 3.5) years, respectively.
80 healthy controls were recruited outside the hospital, including 40 females and 40 males. They were matched for gender and age. The median ages of both healthy females and males were 47.1 (SD = 2.8) and 50.9 (SD = 3.0) years old, respectively. Both healthy males (p = 0.10) and females (p = 0.45) were comparable to LPR males and females according to age (Mann–Whitney test). In addition, the mean ages of both LPR males and females were comparable (p = 0.08; Mann–Whitney test).
Clinical findings according to gender
The main reasons for an ENT consultation of LPR patients are described in Table 1. The most common reasons were globus sensation in males and dysphonia in females. According to the RSI scores, we found that females complained more of choking episodes and breathing difficulties compared to males (Table 2). As expected, irrespective of gender, LPR patients had a higher RSI score than healthy subjects for all of the items of the questionnaire (p = 0.01). According to Wilcoxon test, both initial RSI and RFS scores significantly improved after 3 months of treatment in female (RSI = 9.1 ± 5.3; RFS = 4.5 ± 2.7; p < 0.01) and in male groups (RSI = 8.8 ± 7.0; RFS = 5.3 ± 3.6; p < 0.01). There was no significant difference between groups.
Concerning RFS, males had higher scores for laryngeal hyperemia and erythema than females (p = 0.02). The correlation analyses between signs and symptoms according to gender are available in Table 3.
Quality of life according to gender
The scorings for each item of SF-36 according to gender are provided in Table 4. Females had overall lower scores compared with males, but only vitality and the scores describing the impact of the disease on mental health were significantly more severe in the female group.
Subjective voice quality
The scores of the VHI components were significantly lower in healthy subjects compared with LPR patients in both genders (Table 5). From the blinded perceptual evaluations of our experienced laryngologists, significantly lower scores of dysphonia, roughness, breathiness, strain, and instability were found in controls compared with LPR patients in both gender groups.
Aerodynamic and acoustic measures
The aerodynamic measurements (i.e., MPT, PQ and VC) were significantly better in healthy females in comparison with LPR females.
We did not find a significant difference between healthy and LPR males (Table 6).
Concerning the acoustic parameters, MF0 and Fhi did not differ between healthy and LPR subjects in either gender group.
However, LPR females had more impaired values of Flo than the controls (Table 7).
With regard to the frequency and intensity short-term perturbation parameters, both healthy males and females had significantly better scores of the percent jitter, percent shimmer, NHR, and SPI, than LPR patients (Table 8).
Discussion
Laryngopharyngeal reflux is a causative factor of chronic laryngitis and dysphonia. To date, only five controlled studies have been conducted to compare voice quality between LPR patients and controls; these studies reported unclear conclusions (Table 9). All studies had an evidence-based level of IIb and were monocentric controlled studies. In summarize, these studies showed that patients with LPR-related symptoms and signs had significant impaired subjective and/or objective voice quality than controls but they did not reach to precisely characterize the most impaired measurements related to LPR [7,8,9]. Among these studies, Akiyldis et al. interested to the voice quality impairments in LPR patients according to gender. As found in the second part of the present research, they highlighted that both clinically suspected LPR males and females had stronger values of noise-related measurements and percent shimmer than those of healthy subjects. Moreover, these authors observed that only healthy females had better NHR and percent jitter values than LPR females, supporting the fact that females could have more severe acoustic impairments and, potentially, voice impairments than males [10]. While this is the only study to consider patient gender in the voice quality assessment, they did not assess the other components of voice quality, i.e., subjective self-assessment as well as perceptual and aerodynamic measurements, according to gender. Indeed, it is, therefore, recommended to assess both subjective (i.e., self-assessment and perceptual evaluations) and objective (at least acoustic and aerodynamic measurements) voice quality to obtain the best possible evaluation of a patient’s voice. Furthermore, only one study described aerodynamic measurements. Kumar et al. measured better values of MPT and vital capacity in healthy subjects compared to LPR patients, but finally, both groups were comparable regarding phonatory quotient [11].
Overall, these five previous trials found a better voice quality in healthy subjects than clinically suspected LPR patients but were not able to specify which measurements identify the specific difference. The differences between studies, particularly in the acoustic field, are most likely related to the myriad of methods used to make the LPR diagnosis and perform voice quality evaluations. The heterogeneity of both the diagnosis and methods used to measure the acoustic parameters are highlighted in Table 8. Among the four controlled studies that aimed to compare the objective voice quality (precisely acoustic cues) between LPR patients and controls, the authors used four different methods to perform acoustic measurements; this may lead to differences in results and unclear conclusions. From an acoustic point of view, this is particularly important since we recently demonstrated that depending on the selection of the time interval over which the acoustic parameters are measured, the potential effect of a treatment may or may not be statistically demonstrated [32]. In our study, we chose to measure the acoustic parameters over the entire signal of three sustained vowels produced by the subject. Thus, we did not want to use the 1, 2, or 3 most stable seconds of the signal because we believe that these selected parts of the signal do not represent the patient voice during the phonation task in comparison with the entire signal because it may substantially vary from one second to another.
The first strength of this study is that we performed a multi-parametric voice quality assessment that included subjective self-assessments, perceptual evaluations, and objective measurements on patients with a high probability of LPR disease. With regard to our evaluations, we found that both LPR males and females had impaired voice quality compared to healthy subjects. As proposed in a recent multifactorial model of LPR etiology and pathophysiology, reflux of the gastric content (i.e., acid, pepsin and pancreatic enzymes) into the laryngopharyngeal mucosa leads to the development of several macroscopic and microscopic histopathological changes in the mucosa of the vibratory margin of the vocal folds, such as epithelial cell dehiscence, microtraumas, inflammatory infiltrates, Reinke’s space dryness, mucosal drying, and epithelial thickening [33]. These changes may lead to modifications of the biomechanical properties of the vocal fold tissue which is characterized by aerodynamic impairments, and, as found in acoustic measurements, alterations of the periodicity of the vibration cycle and glottic closure. The lack of change in F0 and MF0 is probably due to some compensatory mechanisms (such as muscular forcing) that broadly preserve the mean F0 as well as increasing the instability of the vibratory process. Indeed, both F0 and mean F0 are measured on an entire signal without regard to these variations from second to second, which are measured with percent jitter and shimmer. Thus, both impaired percent shimmer and jitter and normal F0 and MF0 are consistent with initial modifications of the biomechanical properties of the vocal fold tissue.
Compared to the previously conducted case-control trials, our study is the only study to compare LPR patients according to gender. We demonstrated that females had more primary complaints about dysphonia than males. Moreover, females had lower scores of quality of life and, overall, greater voice quality disorders exhibited by more severe values of aerodynamic measurements and comparable impairments of acoustic parameters to those in males. However, this gender difference was suspected (with more severe acoustic measurements in female than male groups) by Akyildis et al., but was not demonstrated with a multi-parametric voice quality assessment [10]. These differences in gender-related susceptibility to LPR could be explained by anatomical, histological and functional differences. First, it is probable that the shorter and thinner female vocal folds are more easily fully impaired by gastric content leading to faster assessable alterations of the smaller vibrating surface of the female vocal folds [17]. Another hypothesis concerns the Reinke space gender differences. Thus, it has been suspected that the female vocal folds could be characterized by a smaller amount of hyaluronic acid in the superficial layer of the lamina propria [34] that could weaken the vocal fold tissue against gastric content aggression. With regard to some recent hypotheses supporting that the development of LPR voice disorder could be partly related to a Reinke’s space dryness [33, 35], we suspect the involvement of this possible gender anatomical difference in the higher female susceptibility to LPR. The potential dryness of the Reinke space could also modify the biomechanical properties of the vocal folds and could degrade the compliance and the vibration quality of the cordal cover. Following this hypothesis, the limited quantity of hyaluronic acid with additional dryness might induce a reduction of the efficiency of the healing system, promoting vibratory trauma of phonation and epithelial alterations [16, 36]. It is also possible that voicing behavior of women (forcing) can also increase the risk of vocal folds microtraumas. Second, the gender differences in the vibratory alterations related to LPR could be explained by naturally different laryngeal biomechanics and vibratory patterns between genders. Based upon this hypothesis, the membranous and cartilaginous glottal gap, maximal glottal space, and opening pattern of the vocal folds vary from males to females [37]. Thus, studies using high-speed cameras also showed that females frequently had a posterior glottal gap, triangular glottal space and posterior-to-anterior opening pattern of the vocal folds [37]. Dejonckere et Kob reported that females have a more important glottal space leading to a higher subglottic pressure threshold which is needed to initiate the vibration of the vocal folds. Any disease modifying the glottal gap space can lead to the development of a voice disorder and a difference in aerodynamic measurements, such as the phonatory quotient and estimated subglottal pressure, especially in female subjects who had a less adduction [38]. These gender differences can be related to the combination of muscular specific behavior promoting a posterior glottal low adduction and a strong anterior glottal adduction in women [38]. Yet, a sustained oral vowel sound requires a glottal space that is not too small and not too broad. Irritation related to LPR could easily disrupt this glottal gap’s proper balance, especially in females, leading to voice disorders that are manifested by voice perceptual instability and aerodynamic alterations. Hence, we suspect that our aerodynamic results in females can be partly explained by these functional differences. Interestingly, glottal space alterations have already been observed in LPR without particular attention to gender differences [7]. Moreover, Patel et al. reported the existence of a relationship between the development of a glottal insufficiency and chronic symptoms, such as ‘throat clearing’, ‘breathing difficulties’, ‘choking episodes’, and ‘throat mucus secretion’ [39]. However, in our correlation study, we found significant correlations in the female group between some signs and symptoms, especially between a globus sensation and both diffuse laryngeal edema and erythema. In addition, females with sticky laryngeal mucus had higher throat clearing and coughing after lying down scores. These correlations are explained by the pathophysiology of LPR; irritation by the gastric content in the laryngopharyngeal space induces chronic edema, inflammation of the mucosa, and increased secretion of sticky/dehydrated mucus, which is associated with a globus sensation and throat clearing. Interestingly, we did not observe a correlation between edema of the vocal folds and objective voice measurements that supports recent research that claimed that dysphonia related to LPR is not simply the result of edema of the vocal folds [3, 33, 35, 40].
The second strength of this study concerns the very strict inclusion and exclusion criteria in the context of the lack of pH impedance metry even if some factors still remains very difficult to control (daily fluid intake and even mouth breathing or snoring). Indeed, pH/impedance monitoring, which is still considered to be the gold standard by many authors, has been shown to have a variably reported sensitivity of 17.5–78.8% for the diagnosis of LPR, respectively, and the reports were found to be controversial [8, 41,42,43]. In summary, to date, there is no gold standard for LPR diagnosis since pH/impedance measurements fail to impose a reliable diagnosis method for many reasons (i.e., high false-positive and false-negative rates, interpretation difficulties, and inconsistency between pH findings and signs and symptoms) [44, 45]. In this context, we focused on the selection of patients with important and binding exclusion criteria. If a patient had one cofactor that was able to bias the diagnosis, he was immediately excluded. To be included, each patient was required to have a complete response to the empirical treatment or positive results to additional examinations in the case of uncompleted response. Although the response to the empirical treatment is not perfect regarding the risk of placebo effect, and although it is clear that the addition of pH impedance metry at baseline could improve our diagnosis method; we have chosen our approach because it is cost effective, relatively reliable [24, 25] and quite competitive to the direct use of pH/impedance monitoring [46]. Using this approach, we clearly did not recruit a high number of patients, but selected patients with a high probability of LPR without external conditions that were able to bias the LPR clinical expression.
The main weakness of this study is the lack of use of a validated tool to assess and report the findings from videolaryngostroboscopy because, in addition to the anatomical differences, it is possible that the functional voice behavior discrepancies could be involved in the faster development of voice impairments in females. Currently, the only tool available to assess laryngeal findings related to LPR (RFS) does not take into account many LPR signs (i.e., keratosis, ulceration, thickening, etc.) and did not integrate the vocal fold vibration pattern. Moreover, other aerodynamic measurements could be made in the future such as subglottal pressure and lowest intensity (allowing the calculation of dysphonia severity index). Future studies are needed to explore the gender effect on LPR presentation and evolution throughout empirical treatment with standardized tool assessing vibratory findings from videostroboscopy.
Conclusion
Our study suggests that there are some gender differences in the clinical and voice quality presentation of LPR disease, especially regarding the reason for consultation and aerodynamic measurements. These results may indirectly lead to the higher susceptibility of females developing dysphonia related to LPR compared to males. Future studies are needed to precisely evaluate laryngeal signs associated with LPR disease and the stroboscopic pattern of LPR patients according to gender. To provide the comparability of acoustic studies, these studies will need to adopt a standardized method to measure acoustic parameters to allow reliable comparisons between studies.
References
Koufman JA, Aviv JE, Casiano RR, Shaw GY (2002) Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg 127(1):32–35
Sen P, Georgalas C, Bhattacharyya AK (2006) A systematic review of the role of proton pump inhibitors for symptoms of laryngopharyngeal reflux. Clin Otolaryngol 31(1):20–24 (discussion 24)
Jin BJ, Lee YS, Jeong SW, Jeong JH, Lee SH, Tae K (2008) Change of acoustic parameters before and after treatment in laryngopharyngeal reflux patients. Laryngoscope 118(5):938–941
Lee YS, Choi SH, Son YI, Park YH, Kim SY, Nam SY (2011) Prospective, observational study using rabeprazole in 455 patients with laryngopharyngeal reflux disease. Eur Arch Otorhinolaryngol 268(6):863–869
Lechien JR, Finck C, Huet K, Khalife M, Fourneau AF, Delvaux V, Piccaluga M, Harmegnies B, Saussez S (2017) Impact of age on laryngopharyngeal reflux disease presentation: a multi-center prospective study. Eur Arch Otorhinolaryngol 274(10):3687–3696
Koufman JA (1991) The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope 101(4 Pt 2 Suppl 53):1–78
Ross JA, Noordzji JP, Woo P (1998) Voice disorders in patients with suspected laryngo-pharyngeal reflux disease. J Voice 12(1):84–88
Pribuisiene R, Uloza V, Kupcinskas L, Jonaitis L (2006) Perceptual and acoustic characteristics of voice changes in reflux laryngitis patients. J Voice 20(1):128–136
Oguz H, Tarhan E, Korkmaz M et al (2007) Acoustic analysis findings in objective laryngopharyngeal reflux patients. J Voice 21(2):203–210
Akyildiz S, Ogut F, Varis A, Kirazli T, Bor S (2012) Impact of laryngeal findings on acoustic parameters of patients with laryngopharyngeal reflux. ORL J Otorhinolaryngol Relat Spec 74(4):215–219
Kumar R, Bhat JS (2008) Aerodynamic analysis of voice in persons with laryngopharyngeal reflux. Online J Health Allied Scs 7(4):5
Naunheim MR, Carroll TL (2017) Benign vocal fold lesions: update on nomenclature, cause, diagnosis, and treatment. Curr Opin Otolaryngol Head Neck Surg 25(6):453–458
Kantas I, Balatsouras DG, Kamargianis N, Katotomichelakis M, Riga M, Danielidis V (2009) The influence of laryngopharyngeal reflux in the healing of laryngeal trauma. Eur Arch Otorhinolaryngol 266(2):253–259
Martins RH, do Amaral HA, Tavares EL, Martins MG, Gonçalves TM, Dias NH (2016) Voice Disorders Etiol Diagn. J Voice 30(6):761.e1–761.e9
Herrington-Hall BL, Lee L, Stemple JC, Niemi KR, McHone MM (1988) Description of laryngeal pathologies by age, sex, and occupation in a treatment-seeking sample. J Speech Hear Disord 53(1):57–64
Van Houtte E, Van Lierde K, Claeys S (2011) Pathophysiology and treatment of muscle tension dysphonia: a review of the current knowledge. J Voice 25(2):202–207
Zhukhovitskaya A, Battaglia D, Khosla SM, Murry T, Sulica L (2015) Gender and age in benign vocal fold lesions. Laryngoscope 125(1):191–196
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the reflux finding score (RFS). Laryngoscope 111(8):1313–1317
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the reflux symptom index (RSI). J Voice 16(2):274–277
Lechien JR, Huet K, Finck C, Khalife M, Fourneau AF, Delvaux V, Piccaluga M, Harmegnies B, Saussez S (2017) Validity and reliability of a French version of reflux symptom index. J Voice 31(4):512.e1–512.e7
Lechien JR, Harmegnies B, Saussez S (2018) Reply to the letter “Laryngopharyngeal reflux disease in the elderly”. Eur Arch Otorhinolaryngol 275(1):317–318
Lin CC, Wang YY, Wang KL, Lien HC, Liang MT, Yen TT, Wang JP, Liu SA, Wang CC (2009) Association of heartburn and laryngopharyngeal symptoms with endoscopic reflux esophagitis, smoking, and drinking. Otolaryngol Head Neck Surg v141(2):264–271
Chen L, Lai Y, Dong L, Kang S, Chen X (2017) Polysaccharides from Citrus grandis L. Osbeck suppress inflammation and relieve chronic pharyngitis. Microb Pathog 113:365–371
Ford CN (2005) Evaluation and management of laryngopharyngeal reflux. JAMA 294(12):1534–1540
Gupta N, Green RW, Megwalu UC (2016) Evaluation of a laryngopharyngeal reflux management protocol. Am J Otolaryngol 37(3):245–250
Berg M, Fuchs M, Wirkner K, Loeffler M, Engel C, Berger T (2017) The speaking voice in the general population: normative data and associations to sociodemographic and lifestyle factors. J Voice 31(2):257.e13–257.e24
Xue SA, Fucci D (2000) Effects of race and sex on acoustic features of voice analysis. Percept Mot Skills 91(3 Pt 1):951–958
Gorham-Rowan MM, Laures-Gore J (2006) Acoustic-perceptual correlates of voice quality in elderly men and women. J Commun Disord 39(3):171–184
Woisard V, Bodin S, Puech M (2004) The Voice Handicap Index: impact of the translation in French on the validation. Rev Laryngol Otol Rhinol (Bord) 125(5):307–312
Perneger TV, Leplège A, Etter JF, Rougemont A (1995) Validation of a French-language version of the MOS 36-Item Short Form Health Survey (SF-36) in young healthy adults. J Clin Epidemiol 48(8):1051–1060
Braun L (2005) Spirometry, measurement, and race in the nineteenth century. J Hist Med Allied Sci 60(2):135–169
Lechien JR, Delvaux V, Huet K et al (2017) phonetic approaches of laryngopharyngeal reflux disease: a prospective study. J Voice 31(1):119.e11–119.e20
Lechien JR, Saussez S, Harmegnies B, Finck C, Burns JA (2017) Laryngopharyngeal reflux and voice disorders: a multifactorial model of etiology and pathophysiology. J Voice 31(6):733–752
Butler JE, Hammond TH, Gray SD (2001) Gender-related differences of hyaluronic acid distribution in the human vocal fold. Laryngoscope 111(5):907–911
Lechien JR, Finck C, Costa de Araujo P et al (2017) Voice outcomes of laryngopharyngeal reflux treatment: a systematic review of 1483 patients. Eur Arch Otorhinolaryngol 274(1):1–23
Roy N, Tanner K, Gray SD, Blomgren M, Fisher KV (2003) An evaluation of the effects of three laryngeal lubricants on phonation threshold pressure (PTP). J Voice 17(3):331–342
Yamauchi A, Yokonishi H, Imagawa H et al (2014) Age- and gender-related difference of vocal fold vibration and glottal configuration in normal speakers: analysis with glottal area waveform. J Voice 28(5):525–531
Dejonckere PH, Kob M (2009) Pathogenesis of vocal fold nodules: new insights from a modelling approach. Folia Phoniatr Logop 61(3):171–179
Patel AK, Mildenhall NR, Kim W, Carroll TL (2014) Symptom overlap between laryngopharyngeal reflux and glottic insufficiency in vocal fold atrophy patients. Ann Otol Rhinol Laryngol 123(4):265–270
Lechien JR, Huet K, Khalife M, Fourneau AF, Delvaux V, Piccaluga M, Harmegnies B, Saussez S (2016) Impact of laryngopharyngeal reflux on subjective and objective voice assessments: a prospective study. J Otolaryngol Head Neck Surg 45(1):59
Beaver ME, Stasney CR, Weitzel E, Stewart MG, Dono- van DT, Parke RB Jr, Rodriguez M (2003) Diagnosis of laryngopharyngeal reflux disease with digital imaging. Otolaryngol Head Neck Surg 128:103–108
Wiener GJ, Koufman JA, Wu WC, Cooper JB, Richter JE, Castell DO (1989) Chronic hoarseness secondary to gastroesophageal reflux disease: documentation with 24-H ambulatory pH monitoring. Am J Gastroenterol 84:1503–1508
Shaw GY, Searl JP, Young JL, Miner PB (1996) Subjective, laryngoscopic, and acoustic measurements of laryngeal reflux before and after treatment with omeprazole. J Voice 10:410–418
Noordzij JP, Khidr A, Desper E, Meek RB, Reibel JF, Levine PA (2002) Correlation of pH probe-measured laryngopharyngeal reflux with symptoms and signs of reflux laryngitis. Laryngoscope 112(12):2192–2195
Sataloff RT, Hawkshaw MJ, Gupta R (2010) Laryngopharyngeal reflux and voice disorders: an overview on disease mechanisms, treatments, and research advances. Discov Med 10(52):213–224
Wan Y, Yan Y, Ma F et al (2014) LPR: how different diagnostic tools shape the outcomes of treatment. J Voice 28(3):362–368
Acknowledgements
American Journal Expert for the proofreading of the manuscript. This research has been subsidized by the ARC No. AUWB-2012-12/17-UMONS convention from Communauté Française de Belgique.
Funding
This research has been subsidized by the ARC No. AUWB-2012-12/17-UMONS convention from Communauté Française de Belgique.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Lechien, J.R., Huet, K., Khalife, M. et al. Gender differences in the presentation of dysphonia related to laryngopharyngeal reflux disease: a case-control study. Eur Arch Otorhinolaryngol 275, 1513–1524 (2018). https://doi.org/10.1007/s00405-018-4951-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4951-2