Abstract
Although several researchers have tried various canalith repositioning procedures for lateral canalolithiasis, a standard treatment has not been established. We adopt 120° rotation, which is anatomically appropriate because the principle of cure may be the fixing of pathological debris to the dark cells of the utricle. The aims of this study were to clarify the efficacy rate of the affected-ear-up 120° maneuver and to elucidate the appearance rate of lying-down nystagmus in patients with lateral canalolithiasis. The subjects were 31 patients (26 females, 5 males) who revealed transient direction-changing geotropic positional nystagmus. After determining the involved side, we performed the canalith repositioning procedure immediately. To perform this maneuver: (1) Place the patient in the supine position. (2) Rotate the head toward the healthy side until facing downward 120° from supine. (3) Sit up. (4) Ask the patient to remain upright with the chin down until going to bed. Twenty-nine patients (94%) became symptom free by only one maneuver. However, one patient converted to ipsilateral posterior cupulolithiasis, and another required a second maneuver. Lying-down nystagmus was found in 29 patients (94%), the transient type in 23 (74%), and the persistent type in 6 (19%). The direction of transient (not persistent) lying-down nystagmus was mostly toward the healthy side. These results suggest that the affected-ear-up 120° maneuver is effective and that lying-down nystagmus appears at a high rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Benign paroxysmal positional vertigo is classified into two types, a posterior semicircular canal type and a lateral semicircular canal type. Patients with the posterior canal type reveal torsional/vertical nystagmus in the Dix–Hallpike test [1]. The pathophysiology of transient torsional/vertical nystagmus is canalolithiasis (moving debris), while that of persistent torsional/vertical nystagmus is cupulolithiasis (heavy cupula) [2,3,4]. Positional nystagmus of the lateral canal type is classified as direction-changing apogeotropic horizontal nystagmus (APO) or direction-changing geotropic horizontal nystagmus (GEO). APO is always persistent and its pathophysiology is cupulolithiasis [5, 6]. GEO is classified as a persistent type or a transient type. Persistent GEO, which lasts more than 1 min, is thought to be a light cupula [7,8,9,10], and canalolithiasis accounts for transient GEO [11, 12].
Several researchers have tried various kinds of canalith repositioning procedures for lateral canalolithiasis [13,14,15]. However, a standard treatment has not been established. We have carried out the affected-ear-up 120° maneuver for 10 years and are convinced of its effectiveness. The principle of cure may be the fixing of debris to the dark cells of the utricle because positional vertigo and GEO disappear dramatically just after treatment in some cases. Therefore, we ask patients to remain upright until going to bed after the treatment. The first aim of this study was to clarify the efficacy rate of the affected-ear-up 120° maneuver.
In the posterior canal type, the affected side is the direction of the torsional component (not the horizontal component) in the head-hanging position [16]. When the superior pole of the eyeball moves toward the right ear of the patient in a quick-phase, the affected ear is the right. In patients with lateral canalolithiasis, it is not always easy to determine the lesion side. Why is this? The reason is that the right lateral canal lies in the same plane as the left lateral canal. The direction of right stimulatory nystagmus is the same as that of left inhibitory nystagmus. We cannot determine the involved ear by only observing the nystagmus direction. According to Ewald’s second law, stimulation (ampullopetal deflection of the lateral canal cupula) provokes a greater response than inhibition (ampullofugal deflection). Therefore, in patients with canalolithiasis, head turning toward the affected ear produces stronger nystagmus. However, it is not always easy to visually discern the difference of intensity.
Koo et al. [17] introduced the value of lying-down nystagmus. They reported that 43% of patients revealed lying-down nystagmus and it mostly beat toward the healthy side. We had formerly carried out the supine head roll test after keeping the patient at rest in the supine position for several minutes. However, this method cannot detect lying-down nystagmus and we reviewed the test procedure 3 years ago. First, the patient is seated to bring the lateral canal earth-horizontal. After confirming no nystagmus, the position is transformed to supine. This procedure is very important because the gravity produces a sinking of dense particles and an additional pressure to the cupula in canalolithiasis patients. The second aim of this study was to elucidate the appearance rate of lying-down nystagmus.
Materials and methods
Subjects
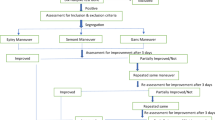
The subjects were 31 patients (26 females, 5 males, mean age of 52.4 years) with lateral canalolithiasis who were diagnosed and prospectively treated from January 2014 to December 2016 at our institution. Group 1 (Patient no. 1–25) consisted of 25 patients who revealed transient GEO the first time. Group 2 (Patient no. 26–31) consisted of 6 patients who changed to transient GEO from APO during a supine head roll test (Fig. 1).
Nystagmus testing
Nystagmus testing was performed in the dark with the patient’s eyes open using an infrared charge-coupled device camera. First, the patient is seated to bring the lateral canal earth-horizontal. After the observation of nystagmus in the sitting position, the examiner reclines the seat so that the lateral canal becomes earth-vertical. Lying-down nystagmus is a finding with this procedure. If lying-down nystagmus was elicited, we confirmed whether it was transient or persistent by keeping the patient in the supine position for 1 min. Afterward, the head was turned toward the right and kept in the right-ear-down position for 1 min to confirm whether the nystagmus was transient or persistent and vice versa (supine head roll test).
Inclusion criteria
-
1.
No nystagmus in the sitting position.
-
2.
In the right-ear-down position, after a brief latency, horizontal nystagmus toward the right occurs, then decays and stops within 1 min.
-
3.
When the head is rotated to the left side, after a brief latency, horizontal nystagmus toward the left occurs, then decays and stops within 1 min.
-
4.
There are no cochlear symptoms related to vertigo and no central nervous system disorder.
Determining the affected side
Group 1 (transient GEO)
The affected side was found by comparing the intensity of nystagmus. If leftward nystagmus is stronger than rightward nystagmus, the affected side is the left. In cases where nystagmus is symmetric, we detected the affected side by the direction of transient lying-down nystagmus. If lying-down nystagmus is toward the right, the affected side is the left.
Group 2 (transient GEO from APO during a supine head roll test)
The side of the neutral position [18] of APO is the affected side.
Treatment
After determining the involved side, we performed affected-ear-up 120° maneuver immediately (Fig. 2). To perform this maneuver:
-
1.
Place the patient in the supine position.
-
2.
Rotate the head toward the healthy side until facing downward 120° from the supine.
-
3.
Sit up.
-
4.
Ask the patient to remain upright with the chin down until going to bed.
Success was defined as symptom free by only one maneuver.
Results
Data on the 31 patients are shown in Table 1. Movie for Patient no. 10 is shown in Supplemental data.
Success rate
The affected-ear-up 120° maneuver was successful in 29 patients (94%). Patient no. 7 transformed to heavy cupula of the ipsilateral posterior canal 2 days after, and positional vertigo continued for seven more days. Patient no. 9 revealed transient GEO at the second visit (4 days after), and the affected-ear-up 120° maneuver was done again. Positional vertigo continued for seven more days. These two patients (6%) were judged as ineffective.
Lying-down nystagmus
29 patients (94%) revealed lying-down nystagmus, the transient type in 23 (74%), and the persistent type in 6 (19%).
Onset time
In 14 patients, vertigo occurred during sleep, in 15 patients at the time of rising. Patient no. 10 felt vertigo just after hanging the laundry at 9 pm. Patient no. 11 felt a spinning sensation at the time of lying down after going to the bathroom at midnight.
Discussion
Our results suggest that the affected-ear-up 120° maneuver is an effective treatment for lateral canalolithiasis. Why is it effective? The main reason may be the function of vestibular dark cells. Several researchers reported that the dark cells of the utricle are engaged in the absorption and demineralization of otoconia [19, 20]. Therefore, we adopt 120° rotation which is anatomically appropriate. Although 270° and 360° maneuvers are effective [14, 15], 120° maneuver has an advantage that we can perform it in a short time. Making patients (especially stout old ladies) prone is surprisingly hard. In addition, less than 180° rotation can avoid transforming canalolithiasis (moving debris) into the cupulolithiasis (heavy cupula). To settle a pathological debris in the utricle, post-maneuver instruction (upright position with the chin down until going to bed) is important, and we recommend the patient sleep with the upper body elevated (Fowler’s position). However, the success rate is not 100%. Patient no. 7 converted to heavy cupula of the ipsilateral posterior canal 2 days after treatment, and Patient no. 9 revealed transient GEO again at the second visit. We speculate that the reason for the ineffectiveness is no adhesion of debris to the dark cells.
Lateralization is not always easy in patients with lateral canalolithiasis. Measuring nystagmus duration is inappropriate because nystagmus toward the lesion side does not last longer than toward the healthy side [11, 21]. Although we compare the intensity of nystagmus in accordance with Ewald’s second law, it is not always easy to visually recognize a stronger direction. Some show almost symmetrical transient GEO. An ideal method is quantitative measurement of maximum slow-phase velocity using real-time electronystagmography; however, this is challenging in practice. The secondary valuable information is lying-down nystagmus. When we encounter it, the point to note is whether it is transient or persistent. If this determination is uncertain, persistent GEO is misdiagnosed as lateral canalolithiasis [17]. Persistent GEO is due to a light cupula. After transforming the patient’s position from sitting to supine, observing the decay of nystagmus for 1 min is very important.
Lying-down nystagmus appears at a high rate. Most transient lying-down nystagmus is toward the healthy side. This phenomenon means that unwanted debris locates in the lateral side of the canal (Fig. 3a). Firstly, debris is not a coming-in particle. Ichijo [22] proposed a micro-otoconia accumulation theory in which the pathological debris is an aggregate of micro-otoconia over a long time period, and it begins to slide by its own weight during sleep. According to this theory, the deposit grows in the lateral side of the long arm. In many cases, moving debris may stay there because the patients instinctively avoid moving the head after the onset. If pathological debris stays at the posterior edge of the lateral canal, no lying-down nystagmus occurs (Fig. 3b). In this case, we need to judge the lesion side by the laterality of transient GEO. Infrequently, lying-down nystagmus is toward the affected side (stimulatory nystagmus), because pathological debris locates in the medial side of the canal. There are some exceptions.
In cases of APO with persistent lying-down nystagmus, some show transformation to transient GEO after the affected-ear-down position [23,24,25]. These phenomena indicate that the attached debris got unstuck and entered the long arm, and the size of the moving pathological particle is almost the same as the size of the debris, which causes cupulolithiasis (Fig. 4). Furthermore, moving debris may not be multiple, but single. Although House and Honrubia [26] predicted that moving debris is much smaller (lighter) than the attached otoconia on the cupula, these theoretical models are unreliable.
At the first visit of patients, we need to confirm whether APO transforms to transient GEO or not by keeping the patient in the affected-ear-down position for 1 min. Animal studies have shown that the surface of the cupula is sticky [27, 28]. We speculate that small (light) particles never get unstuck because of an adhesive power, and big (heavy) debris sometimes falls off the cupula and enters the long arm.
As mentioned above, lying-down nystagmus and the supine head roll test are valuable for lateralization. Examiners need to observe patient’s eye movements in the sitting position and while reclining carefully, before performing the Dix–Hallpike test. If horizontal nystagmus is elicited by the supine head roll test, the examiner needs to pay attention to the direction, intensity and decay. When transient GEO is elicited and the lesion side determined, the affected-ear-up 120° maneuver should be performed immediately.
Conclusion
The affected-ear-up 120° maneuver is effective in patients with lateral canalolithiasis. It is easier to perform compared to other maneuvers. Lying-down nystagmus appears at a high rate, and it is valuable for lateralization. The direction of transient (not persistent) lying-down nystagmus is mostly toward the healthy side.
References
Dix MR, Hallpike CS (1952) The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol 61:987–1016
Imai T, Takeda N, Ito M et al (2009) 3D analysis of benign positional nystagmus due to cupulolithiasis in posterior semicircular canal. Acta Otolaryngol 129:1044–1049
Ichijo H (2013) Cupulolithiasis of the posterior semicircular canal. Am J Otolaryngol 34:458–463
Cupulolithiasis (heavy cupula) of the left posterior semicircular canal. https://www.youtube.com/watch?v=D3qpATkJp2s. Accessed 5 July 2017
Baloh RW, Yue Q, Jacobson KM et al (1995) Persistent direction-changing positional nystagmus: another variant of benign positional nystagmus? Neurology 45:1297–1301
Bisdorff AR, Debatisse D (2001) Localizing signs in positional vertigo due to lateral canal cupulolithiasis. Neurology 57:1085–1088
Hiruma K, Numata T (2004) Positional nystagmus showing neutral points. ORL J 66:46–50
Ichijo H (2012) Persistent direction-changing geotropic positional nystagmus. Eur Arch Otorhinolaryngol 269:747–751
Kim CH, Kim MB, Ban JH (2014) Persistent geotropic direction-changing positional nystagmus with a null plane: the light cupula. Laryngoscope 124:15–19
Seo T, Shiraishi K, Kobayashi T et al (2016) Clinical course of persistent geotropic direction-changing positional nystagmus with neutral position-Light cupula. Acta Otolaryngol 136:34–37
McClure JA (1985) Horizontal canal BPV. J Otolaryngol 14:30–35
Baloh RW, Jacobson K, Honrubia V (1993) Horizontal semicircular canal variant of benign positional vertigo. Neurology 43:2542–2549
Epley JM (1995) Positional vertigo related to semicircular canalithiasis. Otolaryngol Head Neck Surg 112:154–161
Lempert T, Tiel-Wilck K (1996) A positional maneuver for treatment of horizontal-canal benign positional vertigo. Laryngoscope 106:476–478
Escher A, Ruffieux C, Maire R (2007) Efficacy of the barbecue manoeuvre in benign paroxysmal vertigo of the horizontal canal. Eur Arch Otorhinolaryngol 264:1239–1241
Ichijo H (2013) Asymmetry of positioning nystagmus in posterior canalolithiasis. Acta Otolaryngol 133:159–164
Koo JW, Moon IJ, Shim WS et al (2006) Value of lying-down nystagmus in the lateralization of horizontal semicircular canal benign paroxysmal positional vertigo. Otol Neurotol 27:367–371
Ichijo H (2016) Neutral position of persistent direction-changing positional nystagmus. Eur Arch Otorhinolaryngol 273:311–316
Yamane H, Imoto T, Nakai Y et al (1984) Otoconia degradation. Acta Otolaryngol Suppl 406:263–270
Harada Y, Takumida M (1990) Functional aspects of the vestibular dark cells in the guinea pig: morphological investigation using ruthenium red staining technique. Auris Nasus Larynx 17:77–85
Ichijo H (2011) Positional nystagmus of horizontal canalolithiasis. Acta Otolaryngol 131:46–51
Ichijo H (2017) Onset time of benign paroxysmal positional vertigo. Acta Otolaryngol 137:144–148
Shigeno K (2015) Positional treatments for lateral semicircular canal benign paroxysmal positional vertigo. Equilib Res 74:191–198
Curious positional nystagmus. https://www.youtube.com/watch?v=IJMkkW6DOMQ&t=6s. Accessed 5 July 2017
Appiani GC, Catania G, Gagliardi M et al (2005) Repositioning maneuver for the treatment of the apogeotropic variant of horizontal canal benign paroxysmal positional vertigo. Otol Neurotol 26:257–260
House MG, Honrubia V (2003) Theoretical models for the mechanisms of benign paroxysmal positional vertigo. Audiol Neurootol 8:91–99
Otsuka K, Suzuki M, Furuya M (2003) Model experiment of benign paroxysmal positional vertigo mechanism using the whole membranous labyrinth. Acta Otolaryngol 123:515–518
Valli P, Botta L, Zucca G et al (2008) Simulation of cupulolithiasis and canalolithiasis by an animal model. J Vestib Res 18:89–96
Acknowledgements
We thank Dr. Kazunori Futai for preparing some of the figures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
None.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ichijo, H. Affected-ear-up 120° maneuver for treatment of lateral semicircular canal benign paroxysmal positional vertigo. Eur Arch Otorhinolaryngol 274, 3351–3357 (2017). https://doi.org/10.1007/s00405-017-4663-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4663-z