Abstract
Retrospective analysis on 312 patients, operated for thyroid nodules between 2014 and 2015, was conducted to evaluate the impact of frozen section analysis on the strategy of thyroid nodule surgery. One hundred and ninety-three patients were included. They all underwent preoperative US, fine needle aspiration cytology (FNAC), per operative frozen section (FS) and post operative definitive pathological analysis. Se, Sp, VPP and VPN of FNAC and FS were calculated and compared (McNemar’s test). Multivariate analysis was performed to identify independent factor of good results. Se of FS and FNAC were, respectively, 86.1 and 81% with significant superiority of FS (p = .0352). Sp of FS and FNAC were, respectively, 100 and 72% with significant superiority of FS (p = .0156). A strategy based only on FNAC would have led to a 3.6% rate of unnecessary total thyroidectomy vs. 0% using FS. Overall rate of second procedure after lobectomy would have been significantly greater 28.9% without (28.9%) than with (10.3%) FS (p = .018). Overall rate of undone one-stage central neck dissection concurrent to total thyroidectomy for MNG would not have been significantly different without (9.4%) and with (2.1%) FS (.058). FNAC alone is unable to determine the extent of thyroid nodule surgery whatever the Bethesda subtype may be. FS significantly decreases the risk of two-stage procedure. For one-stage total thyroidectomy for MNG, the gain with FS is scarce.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Nodular thyroid disease is a common pathology, whose prevalence is 5–10% for women and 1–2% for men [1, 2]. Radiologic assessments by US raise it up to 67% by discovering subclinical nodules [3, 4]. Malignancy rate ranges from 5 to 13% [5]. Many patients, thus, undergo surgery for benign nodules.
The aim of US and fine needle aspiration cytopathology (FNAC) assessment is to select patients with nodules suspicious of malignity that require surgery. Frozen section (FS) allows peroperative decision for total thyroidectomy and/or a central neck dissection to avoid a two-stage procedure.
A trend in medical demography decrease leads to less availability of FS. As an example, in our institution, pathologists are reducing indication for MNG, and analysis is no longer performed by thyroid-specialized pathologists [6]. Moreover, optimization of operating time also limits its use. FNAC has gain in accuracy with Bethesda system and it has been advocated that it could replace FS in some cases. Some European countries have already limited FS to Bethesda subgroup.
The objective of this study was to evaluate the contribution of FS compared to FNAC in the peroperative strategy and its capacity to avoid unjustified total thyroidectomy and to limit two-stage procedure.
Materials and methods
Study design
A retrospective bicentric study was realized from a series of 312 patients who undergone a thyroidectomy between January 2014 and July 2015 in the head and neck department of two different institutions. Agreement from ethical committee was obtained from each institution.
Inclusion criteria were as follow:
-
Patient that undergone total thyroidectomy or lobectomy,
-
A US imaging for pre-operative assessment,
-
At least one pre-operative FNAC,
-
A peroperative FS,
-
A definitive and complete pathological analysis.
Exclusion criteria were:
-
Basedow disease,
-
Hashimoto disease.
Population
According to these criteria, 193 patients were included with a mean age of 48 years and 73.1% female. The average body mass index (BMI) was 24.9. A unilateral lobectomy was performed in 53.9% and a total thyroidectomy in 46.1% of the cases. The average size of the main nodule was 2.5 cm at final pathological analysis.
Methods
Techniques
According to recommendation, FNAC was performed for nodules bigger than 2 cm, or than 0.7 cm in case of US malignant features. A trained radiologist under US guidance always performed it and pathologists of the two different centers analyzed the samples. Results were always expressed according to the 2008 NCI/Bethesda cytopathology system [7,8,9].
US was always performed by a trained radiologist, and expressed according to the TI-RADS classification in 148 cases [10, 11]. Thyroid with more than two nodules was defined as multi-nodular and size was given in three perpendicular planes.
For FS, tumor blocks were transported by pneumatic tube transport system from the operating room to the pathologist laboratory for one of the two centers and analyzed in the operative room for the other. Results were given orally to the surgeon as follows: benign, malign, diagnosis pending. Histologic subtype was specified when possible. After thawing and fixation in 10% formaldehyde, specimens were included in paraffin for definitive diagnosis on HES staining [12].
Definitive pathological analysis described tumor sizes, malignancy or not, histological subtype in case of carcinoma and nodule capsular invasion, adjacent tissues invasion, and lymph node metastasis. The size of the greater axis was considered for further analysis.
Data recording–statistical analysis
Medical records were consulted based on operating schedules in each center. All data were filed in Excel file including: ID number, date of birth, age, gender, BMI, number and results of thyroid FNAC, US features, multi-nodularity, surgical technique (lobo-isthmectomy or total thyroidectomy), FS result, definitive pathological description including, capsular invasion, adjacent tissue invasion, lymph nodes metastasis, and need for a second surgical procedure.
FNAC results were gathered for statistical analysis in two groups: Bethesda I, II, III and IV under “nonmalignant” group and Bethesda V and VI under “malignant” group. FS results were also gathered in two groups: benign and indeterminate were in the “nonmalignant” group and malignant in the “malignant group”. Results were considered as “good diagnosis” if FNAC or FS were “malignant” and definitive histologic diagnosis malignant, or if FNAC or FS was “nonmalignant” and definitive histologic diagnosis benign. All others results were considered as “bad diagnosis”.
Sensibility (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV) were calculated for FS and for FNAC. Quantitative parameters were described as follows: mean ± SD (min-Q1-median-Q3-maximum). Univariate analysis evaluating the risk factor of “bad diagnosis” for FS and FNAC was realized using the student’s t test and chi-squared test. Sample size allowed only a two-criteria-based multivariate analysis. Analysis of qualitative paired variables was done with the exact test of Fisher.
SAS 9.4 software was used for the statistical analysis with the control of a biostatistician from the clinical research center of our institution.
Results
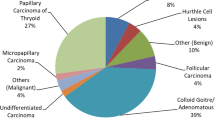
In this study, the global carcinoma rate on the definitive histological analysis was 25.9% including 13 microcarcinomas (T1a).
US
TI-RADS 3 concerned 61 patients; among them, 85.5% (n = 53) had a benign definitive histologic diagnosis. TI-RADS 4A concerned 56 patients; among them, 78.2% (n = 43) had a benign definitive histologic diagnosis. TI-RADS 4B concerned 24 patients, and 50% had a benign definitive histologic diagnosis. TI-RADS 4C concerned two patients and one had a benign definitive histologic diagnosis. TI-RADS 5 concerned five patients and all of them had a malignant definitive histologic diagnosis.
FNAC (Table 1)
FNAC Se was 81%, Sp 72%, PPV 95.1%, and NPV 36%.
Among Bethesda I patients (39 patients), 74.3% (29 patients) have had only 1 FNAC. Recommendations are followed in 25.7% of the cases. 23% (9 patients) had a thyroid carcinoma on the definitive histologic diagnosis. 7.5% had a BMI above 30 (p = .25); obesity was not a risk factor of non-diagnosis for the FNAC. 38.4% (15 patients) had a nodule size less than 2 cm.
Among Bethesda II patients (58 patients), 77.6% (45 patients) have had only 1 FNAC; therefore, recommendations are followed in only 22.4% of the cases. 6.9% (4 patients) had a thyroid carcinoma on the definitive histologic diagnosis and 3 over 4 were classified as multi-nodular T1 (respectively, 8, 11, 14 mm).
Among Bethesda III patients (42 patients), 11 have had more than 1 FNAC. 21.4% of the patients (9 patients) had a thyroid carcinoma. 5 were classified as T1 and 4 over 5 were microcarcinomas.
Among Bethesda IV patients (30 patients), 8 have had more than 1 FNAC. 33.3% of the patients (10 patients) had a thyroid carcinoma; 7 of them were classified as T1.
Among Bethesda V patients (23 patients), 2 have had more than 1 FNAC. 73.9% of the patients (17 patients) had a thyroid carcinoma. 2 among them had a “nonmalignant” FS and, therefore, had a second surgical time needed. 7 patients had finally benign tumor; for half of them, the FS could not be concluded.
One patient had a Bethesda VI FNAC, definitive histologic diagnosis was a thyroid carcinoma, and in that case, the FS misdiagnosis “nonmalignant”.
False-negative (FN) (n = 23) were small tumor, 62% (n = 15) were T1 and 39.1% (n = 9) were multi-nodular goiter (MNG). A univariate analysis was performed and FNAC had worst performance for small tumors (less than 2 cm) (p = .007). Multi-nodularity was not a risk factor of bad diagnosis (p = .0529).
Multivariate analysis was not performed because only one parameter was found significant with univariate analysis.
FS (Table 1)
FS Se was 86.1%, Sp 100%, PPV 100%, and NPV 54%.
A hundred and sixty-six patients had a “nonmalignant” FS; among them, 13 were diagnosis pending. In 86.7% of the cases (144 patients), the definitive histologic diagnosis was benign. 27 patients had a “malignant” FS; in 100% of the cases, the definitive histologic diagnosis was malignant: 23 PC, 3 MTC, and 1 VC.
FN (n = 22) were also small tumor (less than 2 cm) for 68.1% of them (n = 15) and it was mostly isolated tumor (n = 15) and papillary carcinoma (n = 18). Univariate analysis was performed and FS had worst performance for small tumors (p = .0087). The multi-nodularity was not a risk factor of bad diagnosis (p = .1264).
No multivariate analysis was performed because only one parameter was found significant with univariate analysis.
Histologic variant of papillary carcinoma was diagnosed in 4.6% of the cases (n = 9).
FNAC and FS comparison (Table 2)
FS Se was significantly higher than FNAC Se (p = .0352) with FS correctly ranked 54% of the patients (27/50) and FNAC only 36% (18/50).
FS Sp was significantly higher than FNAC Sp (p = .0156) with FS correctly ranked 100% of the patients (143/143) and FNAC 95.1% of them (136/143).
Surgical strategy and need for two-stage procedure
In eleven patients with initial lobo-isthmectomy (5.7%), a second surgical procedure was required because definitive malignant diagnosis was made for tumors bigger than 1 cm (8 T2, 3 T1b bigger than 1.5 cm).
For one of them, second procedure was justified by failure of response of inferior laryngeal nerve monitoring. The remaining 10 cases were FS false-negative. In one case, FNAC was Bethesda V, and in 81.8% (n = 9), FNAC was “nonmalignant”.
Completion of the thyroidectomy was performed in all the cases, and for two patients, a central neck dissection was associated. No second procedure was realized for central neck dissection alone.
Among the 23 false-negatives of FS, 13 were microcarcinomas and did not need a completion of thyroidectomy.
All the FNAC false-positives (n = 7) were correctly classified by FS. Five among them were carcinomas over 1 cm and would have been treated by unnecessary total thyroidectomy in absence of FS analysis (3.6% of the cohort). Among the 32 FNAC false negatives, 15 patients would have needed a two-stage procedure in the absence of FS analysis (7.7% of the cohort).
Unnecessary total thyroidectomy and two-stage procedure overall rate would have been 3.6 and 7.7% without FS vs 0 and 5.2% with FS. In patient initially treated with lobo-isthmectomy, the rate of two-stage procedure would have been significantly higher without FS (28.9%) vs with FS (10.3%) (p = .0018). In patient initially treated with total thyroidectomy for bilateral MNG, 9.4% would not have undergone a central neck dissection without FS vs 2.1% with FS (p = .058).
Discussion
Malignancy of a thyroid nodule diagnosis is based on definitive histologic analysis. The aim of US, FNAC and FS is to diagnose malignancy during the surgical procedure to avoid two-stage procedure for completion of thyroidectomy.
For bilateral MNG, FS is still recommended to determine malignancy and a central neck dissection is performed in a one-stage procedure. At least, an ipsilateral central neck dissection is recommended in this case since it is relevant for stratification and the disease control even if no benefit in survival has been demonstrated nor can it be [13,14,15]. In case of definitive malignancy, second-stage procedure for central neck dissection is not recommended regarding to higher risk of complications. For isolated nodules or unilateral MNG, peroperative diagnosis of malignancy allows completion of thyroidectomy and central neck dissection in one-stage procedure.
The recent evolution of pathologists demography [6] and increasing difficulties of organization in operating schedule led us to question the need of FS. The quality improvement of FNAC and US according to the 2008 NCI/Bethesda cytopathology system led to a decrease in interest for FS.
Some authors had advocated that FS is interesting only in case of suspicions of malignancy on FNAC to confirm the necessity of a completion of thyroidectomy and a central neck dissection [16, 17]. Other authors even conclude that FS does not change surgical strategy. In a retrospective study on 252 patients, Guevara and al reported that FS had a worse Se than FNAC and did not impact surgical strategy [18]. In a meta-analysis from 22 studies, Stanciu-Pop et al. found that 66% of authors considered that FS benefits only to patients with nodules suspicious of malignancy or malignant, because in those cases, it allows central neck dissection [19]. In an American prospective non-randomized study, Udelsman et al. compared two groups of thirty patients with and without FS. They did not find any significant difference between the two groups in terms of two-stage surgery but an additional cost of 12,470$ due to FS. However, results of this study should be taken with caution because the cost of a second procedure and the complications have not been studied. Furthermore, health costs are not stackable from a country to another [20]. Lang et al. even suggests that despite the higher loco-regional recurrence risk, half of the patients are undergoing a completion of thyroidectomy after a lobectomy. Initial lobectomy would be a more cost-effective long-term option for isolated nodules form 1 to 4 cm [21]. We could add that Kim et al. showed after a study on 11,569 patients in 20 years that prophylactic central neck dissection does not decrease the risk of loco-regional recurrences and it increased significantly surgical morbidity [22]. Those studies highlight the fact that FS could be useless.
However, the results of our study suggest that FS can change peroperative strategy favorably and independently to FNAC. Se and Sp were higher for FS than for FNAC. FS had less FN. Among the 23 FN of FS, only 10 (5.2%) had undergone a two-stage surgery for isolated macrocarcinoma. Only one of them had an FNAC “malignant”. FS had no FP; thus, no unnecessary total thyroidectomy was performed. Unnecessary total thyroidectomy and two-stage surgery rates would have been, respectively, 3.6 and 7.7% without FS vs 0 and 5.2% with FS. Other studies also suggest the superiority of FS compared to FNAC. In their meta-analysis, Stanciu-Pop et al. found that FS decreases the rate of two-stage surgery [19]. In a retrospective study on 91 patients, Lee et al. found Se and Sp of FNAC of 60 and 100% vs 82 and 100% for FS. For the authors, the low Se of FNAC does not permit its use as a tool to guide surgery but only as a pre-operative screening tool [23]. In another retrospective study on 163 patients, Boutin, P. et al. found Se and Sp of FNAC of 40 and 100% vs 73 and 99% for FS. They suggest that FS should be always performed whereas FNAC is of poor interest in bilateral MNG and nodules bigger than 2 cm [24]. In a retrospective study on 662 patients Chang and al found that FS is a better assessment than FNAC. In discordance cases, FS led to good diagnosis in 78.9% and FNAC in only 21.1%. They suggest that FNAC should be used only to select patients that need definitive histologic diagnosis, and FS is the only assessment that can limit the rate of two-stage surgery and unnecessary total thyroidectomy [25]. In a retrospective study on 703 patients over 17 years, Heyman et al. found an FNAC Se and Sp of 50 and 92.4% leading to an exclusive use for pre-operative screening [26]. In a recent study, Lee et al. showed the interest of prophylactic central neck dissection and, therefore, of FS: a lymph node ration ≥0.26 was an independent predictor of regional lymph node recurrence in papillary thyroid cancer patients [27].
In our study, size was the only independent predictive factor of FS and FNAC accuracy with more FN for nodules smaller than 2 cm. For nodules smaller than 1 cm, total thyroidectomy is no longer recommended. In a retrospective study on 119 patients with Bethesda III and IV nodule, age under 30 was the only predictive factor of malignancy. Gender, nodule size and US features were non-significant [28]. Therefore, except for infra-centimetric nodules, size is not a criterion to select patients that require peroperative FS.
In bilateral MNG subgroup, the rate of one-stage central neck dissection was higher with than without FS but non-statistically significant difference was found (p = .058). In that subgroup, only the interest of FS seemed imitated.
Conclusion
The results of our study suggest that the diagnosis of malignancy cannot be based on FNAC alone. In our experience, FS should always be performed for supra-centimetric isolated nodules because only FS can improve the surgical strategy in those cases. FNAC selects patients that require definitive histological diagnosis. For isolated macro-nodules, FS significantly decreases two-stage surgery rate, whereas in bilateral MNG subgroup, its benefit is very limited because thyroidectomy is always total and there is no significant difference in the rate of central neck dissection performed with and without FS.
Gain to avoid a two-stage surgery should be balanced with the cost of systematic FS. A medico-economic prospective study comparing surgical strategy with or without FS for isolated nodules could answer that question.
References
Tunbridge WM, Evered DC, Hall R, Appleton D, Brewis M, Clark F et al (1977) The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf). 7(6):481–493
Vander JB, Gaston EA, Dawber TR (1968) The significance of nontoxic thyroid nodules. Final report of a 15-year study of the incidence of thyroid malignancy. Ann Intern Med 69(3):537–540
Tan GH, Gharib H (1997) Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. Ann Intern Med 126(3):226–231
Datta RV, Petrelli NJ, Ramzy J (2006) Evaluation and management of incidentally discovered thyroid nodules. Surg Oncol 15(1):33–42
Hegedus L (2004) Clinical practice. The thyroid nodule. N Engl J Med 351(17):1764–1771
Kafe H, Hassoun J, Adotti F, Gosselin B (2001) Medical demography: pathology’s portrait in France. Ann Pathol 21(1):21–28
Cibas ES, Ali SZ (2009) The Bethesda system for reporting thyroid cytopathology. Thyroid. 19(11):1159–1165
Heller MT, Gilbert C, Ohori NP, Tublin ME (2013) Correlation of ultrasound findings with the Bethesda cytopathology classification for thyroid nodule fine-needle aspiration: a primer for radiologists. AJR Am J Roentgenol 201(3):W487–W494
Deniwar A, Hambleton C, Thethi T, Moroz K, Kandil E (2015) Examining the Bethesda criteria risk stratification of thyroid nodules. Pathol Res Pract 211(5):345–348
Russ G (2016) Risk stratification of thyroid nodules on ultrasonography with the French TI-RADS: description and reflections. Ultrasonography. 35(1):25–38
Russ G, Royer B, Bigorgne C, Rouxel A, Bienvenu-Perrard M, Leenhardt L (2013) Prospective evaluation of thyroid imaging reporting and data system on 4550 nodules with and without elastography. Eur J Endocrinol 168(5):649–655
Franck B BN, Cabaret V, Coudray C, Dubernet, Espie M, Froment N (1997) Examen anatomo-pathologique dans les pathologies mammaires et thyroidienne recommandation professionnelle ANAES
Carling T, Udelsman R (2014) Thyroid cancer. Annu Rev Med 65:125–137
Chan AC, Lang BH, Wong KP (2013) The pros and cons of routine central compartment neck dissection for clinically nodal negative (cN0) papillary thyroid cancer. Gland Surg. 2(4):186–195
Lee DY, Oh KH, Cho JG, Kwon SY, Woo JS, Baek SK et al (2015) The benefits and risks of prophylactic central neck dissection for papillary thyroid carcinoma: prospective Cohort study. Int J Endocrinol. 2015:571480
Haymart MR, Greenblatt DY, Elson DF, Chen H (2008) The role of intraoperative frozen section if suspicious for papillary thyroid cancer. Thyroid. 18(4):419–423
Lumachi F, Borsato S, Tregnaghi A, Marino F, Polistina F, Basso SM et al (2009) FNA cytology and frozen section examination in patients with follicular lesions of the thyroid gland. Anticancer Res 29(12):5255–5257
Guevara N, Lassalle S, Benaim G, Sadoul JL, Santini J, Hofman P (2015) Role of frozen section analysis in nodular thyroid pathology. Eur Ann Otorhinolaryngol Head Neck Dis. 132(2):67–70
Stanciu-Pop C, Pop FC, Thiry A, Scagnol I, Maweja S, Hamoir E et al (2015) Controverse concernant le benefice et les limites de l’examen extmeporané dans les pathologies thyroidiennes An Evidence-Based Assessment. Rev Med Liege 70(12):638–643
Udelsman R, Westra WH, Donovan PI, Sohn TA, Cameron JL (2001) Randomized prospective evaluation of frozen-section analysis for follicular neoplasms of the thyroid. Ann Surg 233(5):716–722
Lang BH, Wong CK (2016) Lobectomy is a more cost-effective option than total thyroidectomy for 1 to 4 cm papillary thyroid carcinoma that do not possess clinically recognizable high-risk features. Ann Surg Oncol 23(11):3641–3652
Kim SK, Woo JW, Lee JH, Park I, Choe JH, Kim JH et al (2016) Prophylactic central neck dissection might not be necessary in papillary thyroid carcinoma: analysis of 11,569 cases from a single institution. J Am Coll Surg 222(5):853–864
Lee JC, Siow JK (2002) Thyroid surgery—the Tan Tock Seng Hospital otolaryngology experience. Ann Acad Med Singapore 31(2):158–164
Boutin P, Bozorg Grayeli A, Terrada C, Rondini-Gilli E, Mosnier I, Julien N et al (2003) Resultats de la cytoponction, de l’examen extemporanée et de l’anatomopatholgie definitve dans les pathologies thyroidienne. sur 163 cas. Rev Laryngol Otol Rhinol (Bord) 124(1):59–63
Chang HY, Lin JD, Chen JF, Huang BY, Hsueh C, Jeng LB et al (1997) Correlation of fine needle aspiration cytology and frozen section biopsies in the diagnosis of thyroid nodules. J Clin Pathol 50(12):1005–1009
Heyman S, Pirenne Y, Van Elst F, Vervloessem D, Vanderveken M, Willemsen P (2014) Is FNAC (fine needle aspiration cytology) a useful tool in detection of malignancy in thyroid surgery? A single institution experience. Acta Chir Belg 114(2):115–117
Lee YC, Na SY, Park GC, Han JH, Kim SW, Eun YG (2016) Occult lymph node metastasis and risk of regional recurrence in papillary thyroid cancer after bilateral prophylactic central neck dissection: a multi-institutional study. Surgery. doi:10.1016/j.surg.2016.07.031
Iskandar ME, Bonomo G, Avadhani V, Persky M, Lucido D, Wang B et al (2015) Evidence for overestimation of the prevalence of malignancy in indeterminate thyroid nodules classified as Bethesda category III. Surgery. 157(3):510–517
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study has no conflict of interest.
Rights and permissions
About this article
Cite this article
Estebe, S., Montenat, C., Tremoureux, A. et al. Limitation of intraoperative frozen section during thyroid surgery. Eur Arch Otorhinolaryngol 274, 1671–1676 (2017). https://doi.org/10.1007/s00405-016-4398-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4398-2