Abstract
The aim of this study is to show differences between a modified facelift incision (MFI) for partial parotidectomy versus a bayonet-shaped incision (BSI). 24 patients presenting with a parotid tumor were surgically treated with a partial parotidectomy using a MFI. We generated a “matched pair control group” regarding age, tumor size and gender, who received a BSI. A questionnaire was sent to all patients and relevant data reviewed. The cosmetic satisfaction on a VAS with a MFI was 9.74 (±0.47) compared to BSI with 7.63 (±2.44, p = 0.004). The scoring in the two subgroups “visible scar” and “people noticed my surgery” was significantly better in the MFI group The postoperative skin numbness, skin depression, facial nerve function postoperatively showed no statistical differences. The MFI for parotid tumors has a better outcome than the BSI regarding cosmetic satisfaction and visible scarring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 7 % of the head and neck neoplasms are salivary gland tumors, 75–80 % affecting the parotid gland. Around 80 % of these neoplasms are considered benign [1]. The treatment of choice in these neoplasms is the surgical removal performing a partial or total parotidectomy. The standard incision for parotidectomy is a cervicomastoidal bayonet-shaped incision (BSI) also known as Blair’s incision, which can lead to visible cervical scarring, sometimes causing patient dissatisfaction. The use of a modified facelift incision (MFI) for a parotidectomy was mentioned by Lotte in 1967/1968 and later published by Jost [2, 3]. Appiani also mentioned a modified facelift incision in 1967 and later in 1984 [4]. The purpose of this approach is to move the incision posterior into the hairline and thus avoid a cervical visible scar [3, 5–7]. The implementation of the facelift incision is described in the literature [3–11]. This facelift incision was used in selected patients if particular cosmetic claims were made preoperatively. The aim of this study is to show differences in the patients’ view between a MFI for partial parotidectomy versus the conventional BSI using a visual analog scale.
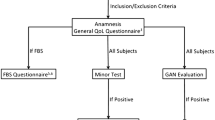
Patients and methods
Surgical technique
The incision and surgical steps are outlined in Fig. 1. MFI begins in the skin area in front of the root of the helix. It is then taken behind the tragus, following the earlobe fold and b ends behind the pinna. It is taken up to the level of the outer ear canal and runs horizontally until it reaches the hairline. The incision is then beveled (trichophytic incision). The skin overlying the parotid gland is then elevated preserving the superficial musculoaponeurotic system SMAS anteriorly until the anterior margin of the gland is visualized. The skin is lifted downwards from the sternocleidomastoid muscle, while preserving the greater auricular nerve. The posterior belly of the digastric muscle and the sternocleidomastoid muscle are separated from the gland. The procedure is then carried out in standard fashion. Illumination by a microscope can be helpful and long retractors are necessary to reach the anterior part of the parotid gland. Furthermore, the pre-auricular incision may be extended superiorly and anteriorly behind the hairline to gain more exposure.
The facial nerve was dissected under magnification and preserved in all cases. A suction drain is placed and the skin is closed in two layers with a 6.0 nylon running suture.
From 2005 to 2013, 24 patients (20 females, 4 males), presenting with a parotid tumor were surgically treated with a partial parotidectomy using a modified facelift incision. All tumors were benign, except one acinic cell carcinoma. High-grade malignancies were excluded in this study. None of our patients received a neck dissection. The histopathology of the MFI group showed 14 pleomorphic adenomas (58.3 %), 3 adenolymphomas (Warthin) (12.5 %), 2 parotideal lymph nodes (8.3 %), one circumscribed chronic parotitis (4.2 %), 1 sarcoidosis (4.2 %), 1 toxoplasmosis (4.2 %), 1 hemangioma (4.2 %) and 1 pT1 acinic cell carcinoma (4.2 %), R-0 resected. The histopathology in the BSI group revealed 9 pleomorphic adenomas (37.5 %), 5 adenolymphomas (Warthin) (20.8 %), 4 parotideal lymph nodes (16.7 %), 2 basal cell adenomas (8.3 %), 2 circumscribed chronic parotitis (8.3 %), 1 hemangioma (4.2 %) and 1 oncocytoma (4.2 %).
The age at time of surgery ranged from 19 to 67 years (mean 43). 80 % of these patients were female. We generated a “matched pair control group” regarding age, tumor size and gender, who received a conventional cervicomastoidal bayonet incision for partial parotidectomy. All patients [modified facelift incision (n = 24) and matched pair control group (n = 24)] were operated by the same surgeon (senior author P. A. F.). Our median follow-up time was 97 months.
The outcome of the patients who received a conventional BSI was compared to those with a MFI regarding cosmetic satisfaction, numbness of ear/skin, depression of the skin, facial nerve function immediately postoperatively, 6 months after surgery and visible scarring. Two additional items were asked: “people noticed my surgery” and “visible scarring is important to me.” A questionnaire using a visual analog scale (Table 1) and other relevant data, along with the surgery time, were collected. For question number one and three (cosmetic satisfaction and depression of the skin) the visual analog scale ranged from “0” indicating not satisfied at all to “10” highly satisfied. For question number two (numbness) “0” indicated “total numbness” to “10” “no numbness.” For question number 4A and 4B (facial nerve function immediately postoperatively and 6 months after surgery) “0” indicated “no function” and “10” “completely functioning.” For question number 5A “visible scar” “0” indicated clearly visible and “10” invisible. Question 5B regarding “people noticed my surgery” “0” indicated everybody noticed to “10” nobody noticed. The sixth and last question concerning “visible scar is important to me:” “0” indicated “very important” and “10” “not important” (Table 1).
Paired t tests were used to compare these two groups; while Χ 2 test were used for analysis of categorical data. p values <0.05 were regarded as statistically significant. Additionally Wilcoxon–Mann–Whitney test was performed to find statistical differences in both groups.
We received 9 answers (38 %) from the modified facelift incision group versus 8 answered questionnaires (33 %) from the matched pair control group.
Data were analyzed using SPSS Statistics vers 22.0 (SPSS Inc., Chicago, IL, USA). This study was approved by the institutional review board (ethic commission/S-097/2015).
Results
The average time of a partial parotidectomy via modified facelift incision was 162 (median 158) min compared to 143 (median 135) min with a bayonet-shaped incision. The difference in surgery time was statistically not significant (p = 0.2). In average, the modified facelift incision took 19 min longer. The size of gland resection in the MFI group showed an average of 29 cm3 (median 21)—versus 31 cm3 (median 28) resection in the BSI group, with no statistical differences in comparison.
One patient in each group needed revision surgery during his hospitalization due to hematoma. No skin necrosis or fistulas occurred. During our follow-up, none of our patients suffered from symptomatic Frey’s syndrome. Minor’s test is only offered in symptomatic patients.
The cosmetic satisfaction on a VAS with a MFI was 9.74 (±0.47) compared to the classical bayonet-shaped incision with 7.63 (±2.44, p = 0.004).
The postoperative numbness with a MFI showed 8.42 (±1.59) versus 8.36 (±2.17, p = 0.81) with a bayonet-shaped incision. Both subgroups showed a nearly intact sensitivity.
The skin depression postoperatively was rated 8.54 (±1.95) in the MFI group versus 6.19 (±3.64, p = 0.16) with a bayonet-shaped incision, showing no significance in both subgroups.
In the MFI group the self reported score for facial nerve function immediately postoperatively was rated 6.18 (±4.16) and 6 months after surgery 8.98 (±2.13) versus 7.89 (±2.45) and 6 months later 8.59 (±2.43) in the classical incision group. Statistically, the difference in both groups was not significant (immediately postoperatively p = 0.96, 6 months after surgery p = 0.54).
One patient in each subgroup (each 4.2 %) showed a temporary paresis of the marginal branch immediately postoperatively. No permanent facial palsy was found in both groups.
There was no statistically significance between MFI and BSI in the subgroups “skin depression” and “sensitivity” using the Wilcoxon–Mann–Whitney test.
The scoring in the two subgroups “visible scarring” (MFI 9.26 ± 1.62 vs BSI 6.88 ± 2.97) and “people noticed my surgery” was significantly better in the modified facelift incision group (MFI 9.24 ± 1.63 vs BSI 6.13 ± 4.14).
There was no statistically difference in the subgroup “visible scarring is important to me” (MFI 5.34 ± 3.7 vs BSI 5.93 ± 3.6) (Figs. 2, 3).
Discussion
Surgical time has been formally analyzed in four studies [6, 7, 10, 12, 13]. The reported average time ranged from 2.5 to 3.25 h for a modified facelift incision. Terris et al. [6] even showed a decreased surgery time for modified facelift incision compared to Blair’s incision. To et al. [13] and Lin et al. [12] reported an increased surgical time by 0.08 and 0.09 h. In our study, the surgery with a conventional incision took 2.34 versus 2.70 h for a facelift incision approach, resulting in an increase of 0.36 h with MFI. The difference in surgery time was statistically not significant (p = 0.2). Due to a more challenging technique, the surgery time using a MFI can be prolonged compared to BSI. In our study, surgery time using a MFI decreased with the surgeon's experience with this approach.
Frey’s syndrome is reported as a complication in up to 27 % in parotidectomies, mostly dependent on the extent of resection [6, 8, 9, 12, 14, 15]. Different reconstructions using superficial musculoaponeurotic system (SMAS) or sternocleidomastoid flaps were discussed to avoid this complication, but remain controversial. There are no statistical significant data in the literature indicating a higher percentage of Frey’s syndrome using a MFI [6, 8, 9, 12, 14, 15]. During our follow-up (median 97 months), we did not experience this complication, which may be due to our limited number of patients. In terms of postoperative complication, one patient in each group (each 4.2 %) needed revision surgery due to a postoperative hematoma. Several authors show similar revision rates due to postoperative complications including postoperative hematoma [6, 8, 9, 12, 14, 15].
In this study, statistically significant differences in outcome between MFI and BSI were shown in three subgroups: “overall cosmetic satisfaction,” “visible scar” and “people noticed my surgery.” The MFI group was more satisfied with the cosmetic outcome, the scar was graded as less visible, and fewer people noticed the surgery according to patient reporting.
Several authors reported on patient satisfaction regarding MFI versus a classical incision [7] for partial parotidectomy.
Wasson et al. [15] is the only study showing a higher scar satisfaction score in 20 patients with Blair’s incision compared to a modified facelift incision using a VAS score, the difference not being statistically significant [7]. Bianchi et al. [8] and Lee et al. [14] also compared a VAS to assess cosmetic outcomes, both reporting a better outcome with MFI, which is in line with our findings. Bianchi et al. [8] also reported statistical significant differences between MFI versus Blair’s incision when rated by an independent person (other than the surgeon or the patient).
Other authors report on subjective outcomes either from the surgeons’ or the patients’ point of view [5, 10, 12, 13, 16], ranging from “all satisfied,” “all excellent,” to “no concerns with scar.” In our questionnaire we asked our patients “if people noticed my surgery” showing a statistically significant differences. Less people noticed the MFI.
It should be mentioned that other authors described alternative incisions, including a smaller incision than the BSI with an extracapsular resection of the parotid tumor, as described by Iro et al. [17, 18].
No statistical significant differences between MFI and BSI were shown regarding skin depression, postoperative numbness of the skin, immediate postoperative facial nerve function, 6 months postoperative facial nerve function. To our knowledge, this study is the first one to show no significant differences between the two surgical groups on a visual analog scale for postoperative numbness of the skin. Several authors reported on a reconstruction of the resection defect using SMAS, the superior part of the sternocleidomastoid muscle or a combination of those two [5, 7, 9, 12, 16]. Neither in our MFI nor in our control BSI group did we use a reconstruction of the surgical site, yet with a high VAS score in cosmetic outcomes in both subgroups. In our study the size of gland resection in the MFI group showed an average of 29 cm3 (median 21)—versus 31 cm3 (median 28) resection in the BSI group, with no statistical significant differences in comparison. In our opinion, filling the defect in partial parotidectomy is not always needed, but can be helpful depending on the amount of gland resection and should be determined individually.
A great concern for patients in our experience is the question of potential additional risk to the facial nerve with a MFI. There was no statistical significance in both groups. The VAS score for facial nerve function 6 months after surgery also does not show a difference in both groups. Wasson et al. [15], Bianchi et al. [8] and To et al. [13] even reported a decrease in facial nerve palsy with a MFI compared to Blair’s incision. Other studies reported [6, 10] no facial nerve damage in both groups. There is only one study suggesting a slight increase in facial nerve palsy after MFI compared to Blair’s incision, with no statistical significance in both groups [12].
In our experience, the landmarks to identify and preserve the facial nerve are equally approachable. In addition to the studies mentioned above, we state that the MFI is in terms of postoperative facial nerve function equal to the conventional incision.
Although most patients in the modified facelift incision group explicitly asked for a “more plastic” approach preoperatively, there was no significant difference to the question “a visible scar is important to me,” comparing MFI and BSI. The most likely reason and at the same time a weakness of this study is the retrospective aspect of this question. Patients who answered this question, where according to their VAS already satisfied with the cosmetic outcome of their surgery. On the other hand, as there is no statistical significance in both subgroups to this question, one might presume that the better VAS results of the overall cosmetic satisfaction and “visible scarring” are reliable.
Nearly all studies and data looking at differences between a MFI and BSI are of retrospective design and therefore limited. The limitations of this study are the low response rate, the limited number of patients and the retrospective nature of this study. However, the response rate was similar in both groups. Further prospective studies with quality of life questionnaires are needed for further evaluation of this surgical approach.
Conclusion
The modified facelift incision for parotidectomy is a safe procedure with a significantly better outcome than the conventional bayonet-shaped incision regarding cosmetic satisfaction and visibility of the scar. There is no significant statistical difference in postoperative skin numbness, skin depression, and immediate- and 6 months postoperative facial nerve function. Because of the somewhat more demanding technique and meticulous skin closure, the surgery time using a modified facelift incision can be slightly prolonged. MFI is a safe procedure.
References
Baumann I et al (2009) Development and validation of the Parotidectomy Outcome Inventory 8 (POI-8). Measurement of quality of life after parotidectomy in benign diseases. HNO 57(9):884–888
Jost G, Legent F, Baudelot S (1968) Filling of residual depressions after parotidectomy by a sterno-cleido-mastoid flap. Ann Chir Plast 13(3):187–191
Jost G, Guenon P, Gentil S (1999) Parotidectomy: a plastic approach. Aesthet Plast Surg 23(1):1–4
Appiani E, Delfino MC (1984) Plastic incisions for facial and neck tumors. Ann Plast Surg 13(4):335–352
Meningaud JP, Bertolus C, Bertrand JC (2006) Parotidectomy: assessment of a surgical technique including facelift incision and SMAS advancement. J Craniomaxillofac Surg 34(1):34–37
Terris DJ, Tuffo KM, Fee WE Jr (1994) Modified facelift incision for parotidectomy. J Laryngol Otol 108(7):574–578
Grover N, D’Souza A (2013) Facelift approach for parotidectomy: an evolving aesthetic technique. Otolaryngol Head Neck Surg 148(4):548–556
Bianchi B et al (2011) Improving esthetic results in benign parotid surgery: statistical evaluation of facelift approach, sternocleidomastoid flap, and superficial musculoaponeurotic system flap application. J Oral Maxillofac Surg 69(4):1235–1241
Honig JF (2004) Facelift approach with a hybrid SMAS rotation advancement flap in parotidectomy for prevention of scars and contour deficiency affecting the neck and sweat secretion of the cheek. J Craniofac Surg 15(5):797–803
Lohuis PJ et al (2009) Superficial parotidectomy via facelift incision. Ann Otol Rhinol Laryngol 118(4):276–280
Amin A et al (2011) Parotidectomy for benign parotid tumors: an aesthetic approach. J Egypt Natl Canc Inst 23(2):67–72
Lin TC et al (2011) Intra-auricular modification of facelift incision with sternocleidomastoid flap–a cosmetic approach for parotidectomy: how we do it. Clin Otolaryngol 36(4):375–379
To EW, Pang PC, Chu GM (2000) The use of modified rhytidectomy for parotidectomy. Br J Plast Surg 53(1):80
Lee SY et al (2011) The extended indication of parotidectomy using the modified facelift incision in benign lesions: retrospective analysis of a single institution. World J Surg 35(10):2228–2237
Wasson J et al (2010) Cervicomastoidfacial versus modified facelift incision for parotid surgery: a patient feedback comparison. Ann R Coll Surg Engl 92(1):40–43
Zhi K et al (2011) Face-lift incision combined with sternomastoid muscular flap in parotidectomy. Aesthet Plast Surg 35(4):558–562
Iro H et al (2013) Follow-up of parotid pleomorphic adenomas treated by extracapsular dissection. Head Neck 35(6):788–793
Mantsopoulos K et al (2015) Evolution and changing trends in surgery for benign parotid tumors. Laryngoscope 125(1):122–127
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Bulut, O.C., Plinkert, P. & Federspil, P.A. Modified facelift incision for partial parotidectomy versus bayonet-shaped incision: a comparison using visual analog scale. Eur Arch Otorhinolaryngol 273, 3269–3275 (2016). https://doi.org/10.1007/s00405-015-3878-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3878-0