Abstract
Binaural sound reception has advantages over unilateral perception, including better localization and sound quality as well as speech and tone reception in both quiet and noisy environments. Up to now, most active middle ear implant (AMEI) users have been unilaterally implanted, but patient demand for an implant on the other side is increasing. Ten bilaterally-AMEI implanted native German-speaking adults were included in the study. The Oldenburg sentence test was used to measure speech reception thresholds in noise. The subject’s signal-to-noise ratio (SNR) at a speech reception score of 50 % was calculated for different noise conditions. SRT was measured as a function of noise condition (nc) and listening condition (lc)—for example, SRT (lc, nc), with nc from S0N0, S0N-90, or S0N90 and lc from left, right or both. For each noise condition, the squelch effect and the binaural summation effect were calculated. Patients in this study demonstrated improvement with bilateral AMEIs compared to right or left AMEI only in all three tested listening conditions. Statistical significance was found in the S0N0 condition to favor usage of bilateral AMI versus either the right or left side only. The benefits of binaural hearing are well known, also in normal-hearing individuals. In the future every bilateral implantation should be a part of the clinical routine. Bilateral implantation can help to reduce problems in background noise and restore directional hearing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Correctly understanding and differentiating conversational speech from background noise of varying complexity, loudness and direction is one of the most complex and integral hearing tasks even for people with perfect hearing in both ears. However, for the hearing impaired, it becomes a primary measure of efficacy for the assistive hearing device they choose. Aided sound perception that most closely mimics natural hearing is dependent on factors such as localization, range of frequencies across which hearing can be effectively aided, and quality of sound, particularly when listening to music.
It is generally accepted that binaural sound reception has advantages over unilateral perception, including better localization and sound quality as well as speech and tone reception in both quiet and noisy environments. Bilateral benefits have been shown for the use of hearing aids [1] as well as for cochlear implants.
However, minimal data exist for the active middle ear implant (AMEI) Vibrant Soundbridge (VSB), which is used for patients with sensorineural, conductive and mixed hearing loss who are unable to use a conventional hearing aid due to audiological or medical reasons. Up to now, most AMEI patients have been implanted unilaterally.
Saliba et al. [2] found that binaural hearing provided by a VSB in the more damaged ear and a hearing aid in the contralateral ear significantly improved warble tone threshold reception as compared with thresholds obtained with only the unilateral implant. A recent multicenter study involving 15 VSB middle ear implant users with symmetrical hearing loss who were bilaterally implanted over a period of time between 15 and 67 months found results similar to Saliba. Garin et al. [3] showed that implantation in both ears provided advantages in speech intelligibility both in quiet at low presentation levels (40 dB) and in noise, with word recognition of close to 60 % at SNR 0 (competing background noise at same level as speech). In addition, they noted an approximately 18 % improvement in word recognition scores at SNR −5 for both ears vs. single ears in the aided condition. However, the ceiling effect (even unilateral word recognition was close to 100 % in quiet) prevented further differentiation of the results and the authors found that a more sensitive test was needed.
Three primary effects on perception have been identified in binaural hearing: the head shadow effect, the binaural summation effect and the binaural squelch effect [4].
The aim of our study was to retrospectively assess everyday speech perception of 10 subjects, and to determine whether or not a positive effect in sound localization and a difference in summation/squelch effect may be seen in bilateral VSB users with mild to moderate sensorineural, conductive or mixed hearing loss, as compared to the same group of patients before they received the second VSB implant. The binaural squelch effect occurs when noise and speech are spatially separated resulting in two different inputs in both ears, in contrast to the summation effect, where the noise and the speech are coming from one direction.
To our knowledge, the results presented in our study represent the first single-center analysis of speech discrimination in bilaterally VSB-aided subjects as measured by signal-to-noise ratios for 50 % correct understanding of words in sentences.
Materials and methods
Subjects
Ten native German-speaking adults (3 female, 7 male) ranging in age from 38 to 84 years (mean 62.7) were included in the study. All of them were implanted with a Vibrant Soundbridge bilaterally with a mean timeframe of 6 months (range 3–14 months) between the two surgeries. The majority of hearing loss (HL) types treated were sensorineural cases (n = 14). In addition there were two cases of conductive and 4 cases of mixed HL treatments in the study. All patients had symmetrical hearing loss (≤10 dB difference between ears, measured by pure tone average at the frequencies of 500, 1000, 2000 and 4000 Hz). Patient demographics are presented in Table 1.
All of the patients were advised to wear a conventional hearing aid for a minimum of 3 months before implantation. If they were not satisfied with the HA, they then became an AMEI candidate. This is a routine procedure for all of the hearing impaired people in our clinic. 6 of our 14 SNHL cases suffered from chronic otitis externa (COE), so they were not able to wear a conventional hearing aid for a period of time. The other patients, who had sudden hearing loss, barotrauma and presbyacusis, had no benefit from a conventional hearing aid due to audiological reasons (distortion, high frequency hearing loss, bad speech understanding in background noise, occlusion).
All subjects used MED-EL Vibrant Soundbridge implants with an AP404 audio processor and had at least 1 month of experience with their most recently implanted VSB implant system. Eight subjects had a classic fixation of the FMT (Vibroplasty) at the long process of the incus. One subject had an incus Vibroplasty in one ear and a stapes Vibroplasty in the other ear. Another subject had a round window Vibroplasty in one ear and a stapes Vibroplasty in the other ear.
Selection criteria
All patients were implanted by the last author and fitted with the VSB between 2008 and 2010 at the Department of Otorhinolaryngology, Head and Neck Surgery, Medical University Innsbruck.
For inclusion they had to be 18 years or older with mild to severe hearing loss. All patients fulfilled the selection criteria for mixed and conductive hearing loss as stated by the device manufacturer. This was defined as bone conduction thresholds at or better than 45–65 dB HL; the sensorineural hearing loss patients needed monosyllabic word recognition scores with well-fit hearing aids of greater than 50 % at 65 dB or at the most comfortable level using earphones. Before inclusion, all subjects were told about the implications of being involved in the study and were required to sign an informed consent form. The study was approved by the local ethics committee.
Device and device settings
The VSB is an active middle ear implant (AMEI) that supports ossicular and cochlear function by transmitting vibrational energy gathered from the external processor and implanted receiver to a floating mass transducer (FMT) placed in the middle ear. Depending on the patient’s indication and individual anatomy, the FMT can either be connected to a middle ear structure to augment the natural function of the ossicles or it can circumvent a damaged ossicular chain and transfer additional vibrational energy to the inner ear through the round window membrane or the oval window/stapes footplate. It is used to treat a wide variety of sensorineural, conductive, or mixed hearing impairments in cases where hearing aids cannot be used or an implantable solution is desired. All subjects used AP404 audio processors. The audio processors were programmed using standard methods between 6 and 8 weeks after surgery with CONNEXX and Symfit software.
Surgical procedure
Using a retroauricular approach, a mastoidectomy and posterior tympanotomy was performed under general anesthesia. The receiver of the VSB was placed into an implant bed drilled into the mastoid area of the temporal bone, and the FMT was then affixed to a structure in the middle ear, depending on the patient’s individual anatomy. For fixation to the stapes or incus, the FMT was attached with a titanium clip or coupler, while placement at the round window (RW) niche took place after the RW membrane was covered with a silicon patch. The development of these different surgical strategies has been detailed and evaluated elsewhere [5, 6].
Test set-up
Tests were performed in a square anechoic chamber measuring 6.4 m by 6.4 m, with a floor-to-ceiling height of 6.78 m. The chamber is equipped with a steel mesh floor and 1-m wedges lining the walls, floor and ceiling. Three WESTRA audiometry speakers were mounted on a 2 m-diameter steel ring at a height of 1.2 m above the floor at −90°, 0° and 90° positions. Subjects were positioned on an adjustable chair in the center of the semicircle of loudspeakers. The height of the chair was adjusted until the subject’s ears were level with the middle of the loudspeakers. The hardware for generating the signals and for data acquisition was placed in a control room outside of the chamber. The experimenter and the subject could communicate through a bidirectional line and the experimenter monitored the subject using a video surveillance system.
Test material
The Oldenburg sentence test was used to measure speech reception thresholds in noise. The subject’s signal-to-noise ratio (SNR) at a speech reception score of 50 % was calculated for different noise conditions. The Oldenburg test consists of 40 lists of 30 sentences each [7, 8]. Each sentence contains 5 words and is generated by permutations of 50 words. Speech signals were presented from WAV files (sampling rate: 44.1 kHz) through a 16-bit sound card. The levels were adjusted by means of two programmable attenuators (Tucker-Davies Technologies, PA4) and connected to the appropriate loudspeaker using a custom-built programmable 2-to-12 multiplexer.
Procedure
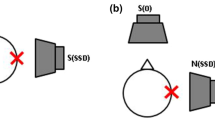
Speech tests were performed for three different noise conditions. The speech signal was always presented from the front (0° azimuth). The noise signal was presented from either the front (S0N0), from the left (−90° azimuth, S0N-90), or from the right (90° azimuth, S0N90). For each noise condition, three different listening conditions were tested: the left VSB alone, the right VSB alone, and both VSBs. In the unilateral listening conditions, the contralateral ear was not blocked or masked, because this would be an unnatural hearing situation. The sequence of the measurement conditions (noise and listening conditions) and the test lists was quasi-randomized.
The noise signal was presented at a constant level of 65 dB SPL, measured in the free field at the center of the subject’s head. The speech signal level was varied to achieve a score of 50 % correct, calculated from the last 20 sentences of each list. The initial speech level was 70 dB SPL; this corresponds with an initial SNR of 5 dB. The subject was instructed to look straight at the front loudspeaker during the tests. Head movements were not allowed and were prevented by the use of a headrest. After each presentation, the subject’s response was recorded and the signal level was adjusted according to the number of words understood correctly, as specified in the Oldenburg sentence test. For example, 5 words correctly understood leads to a 2 dB reduction of the SNR; 4 words, −1 dB; 1 word +1 dB; and 0 words correct leads to an increase of 2 dB. The SNR is kept constant when 2 or 3 words are understood correctly. The tests were presented using only sound, and no feedback as to correct or incorrect responses was given. All subjects were familiar with the sentence test, so only one training list was used prior to testing.
Implant fitting
The goal of the study was to assess a subject’s everyday speech perception. Thus, all subjects were tested using their audio processor’s normal everyday program. These programs were obtained during clinical device fitting, at which time the implants are usually fitted for the first time on each side individually.
Data processing
For each Oldenburg sentence test, the speech reception threshold (SRT) was calculated by averaging the signal levels of the last 20 sentences in each list and subtracting the noise level of 65 dB SPL, as specified in the Oldenburg test manual. SRT was measured as a function of noise condition (nc) and listening condition (lc)—for example, SRT(lc, nc), with nc out of S0N0, S0N-90, or S0N90 and lc out of left, right or both. In the following sections, the terms ipsilateral/contralateral refer to the noise source and the audio processor being on the same side/opposite side of the head, respectively. For example, listening condition “left” (left VSB only), combined with noise condition S0N-90 would be ipsilateral. From the estimated SRTs, two effects were calculated as described below.
For each noise condition (nc) with lateral noise presentation (S0N-90, S0N90), the squelch effect (SQ) is calculated by subtracting the SRT when listening with both audio processors from the SRT when listening with the contralateral implant only [9].
SQ describes the benefit resulting from the spatial separation between the signal source and the noise source. SQ is also referred to as binaural intelligibility difference.
For each listening condition (lc; either left or right), the binaural summation effect (SU) is calculated by subtracting the SRT obtained with both implants from the SRT obtained with one implant in the S0N0 condition:
SU refers to the advantage of hearing with two AMEI with identical signals arriving at both sides of a patient’s head. Note that for all measures, positive values express a beneficial effect on speech perception.
Graphs and calculations were generated using Microsoft Excel 2010 and GraphPad Prism 6.0. The graphs depict all available data; for statistical analysis only the valid data pairs were analyzed. Missing values have not been replaced by imputation methods. Data distribution was tested using the D’Agostino & Pearson omnibus normality test. Significance was accepted at p ≤ 0.05 and was determined using paired two-sided t tests, or one sample t test comparison against a hypothetical value of 0 (=no effect).
Results
Pure tone audiometry
All patients presented with bilateral hearing loss meeting the indication criteria for AMEI implantation as designated by the manufacturer. Pre- and postoperative pure tone audiometry (Table 2) was available in 17 cases for BC and in 14 cases for AC testing. Bone conduction thresholds for both ears did not change significantly when compared pre-, to post-operatively; threshold shifts observed were between 0.8 and 5 dB across the tested frequencies, with a mean of 2.0 dB. For air conduction thresholds a significant shift occurred at the 1 and 4 kHz frequencies. These differences of 5.7 and 7.1 dB, respectively, were not considered as clinically relevant since they were within the accepted test–retest variability range of 10 dB for audiometric testing. The mean threshold difference for AC was 4.1 dB across all tested frequencies.
Free field (FF) testing
Warble tones in the free field were analyzed for the left and right side separately. The mean post-op FF threshold was similar for both sides, with a mean of 36.6 dB HL (SD ± 9.8 dB) on the right side and 37.8 dB HL (SD ± 9.9 dB) on the left side. (Figure 1).
Measurements for one subject’s left side were not available.
Binaural/bilateral effects
Bilateral input with signal and noise presented from the front resulted in a SNR of −0.9 dB (SD ± 2.5 dB), and was significantly different than the mean SNR with the left AMEI only (0.2 dB SNR SD ± 3.1 dB, p = 0.026) and the right AMEI only (0.4 dB SNR, SD ± 2.9 dB, p < 0.001) (Fig. 2). The calculated summation effect was 1.1 (±1.3, left vs. both VSB/s) and 1.3 (±0.7, right vs. both VSB/s) dB SNR (Fig. 3).
The listening condition with separated signal and noise sources resulted in a SNR of −1.5 (SD ± 4.3) dB using the left AMEI only and −2.6 (SD ± 4.1) dB SNR using both AMEIs (p = 0.04), tested with noise from the right side (S0N90). With noise originating from the left (S0N-90), an SNR of −1.7 dB (SD ± 3.5 dB) was found on the right side, bilateral AMEI use resulted in an SNR of −2.7 dB (SD ± 3.0, p = 0.002) (Fig. 4). The mean squelch effect was 1.1 dB (SD ± 1.4 dB) in the S0N90 condition and 1.1 dB (SD ± 0.8 dB) in the S0N-90 condition (Fig. 5).
Surgical complications and adverse events
One patient suffered from a postoperative seroma in the area of the mastoid. The patient was put on oral antibiotics for 10 days to avoid a superinfection of the seroma. In addition, a pressure head bandage was applied for 4 days. The seroma disappeared after 5 days without surgical intervention.
The standard audio processor magnet was too strong for two patients, who complained about uncomfortable pressure under the AP. These patients were advised not to use the AP for 1 week in order to allow the irritated skin over the implant to heal, at which time the patients switched to a weaker AP magnet.
Discussion
Some patients with mild to severe hearing loss do not benefit from conventional hearing aids. Since these patients often have high-frequency hearing loss, occlusion and distortion can limit the amount of improvement they experience with their HA. Other patients have medical problems such as stenosis, recurrent infection in the external auditory canal, chronic otitis media or excessive cerumen. The AMEI offers an approach to help such patients. Although many patients who have been implanted with an AMEI report great satisfaction with the device, some of them express the desire for a second implant if they have similar problems in the other ear. Additionally, these patients describe difficulty with their hearing in everyday listening conditions including sound localization or listening in background noise.
The benefits of binaural hearing are well known, also in normal-hearing individuals. However, hearing-impaired subjects need a better signal-to noise ratio relative to that required by normal-hearing subjects for the same level of speech comprehension. Speech intelligibility in noise remains one of the most accurate measures of efficacy. Speech tests with well-developed protocols such as the Oldenburg sentence test can provide sensitive measurement of the speech intelligibility advantage provided by a particular device. This type of test mimics the challenges of everyday listening situations and thus can provide an accurate predictor of the hearing benefit offered by a given treatment.
Our results show that the patients in this study demonstrated improvement with bilateral AMEI as compared to use of either the right or left AMEI only in all three tested listening conditions (S0N0, S0N90, S0N-90). Statistical significance was found in the S0N0 condition to favor usage of bilateral VSB versus either the right or left side only.
Garin et al. tested 15 bilateral VSB implantees with sensorineural hearing loss, and found that their speech intelligibility in quiet at presentation levels of 40 dB with both ears aided was significantly better than with just the poorer-hearing ear aided [3]. At higher levels the binaural effect could not be determined due to the ceiling effect (even with only the worse ear aided, scores were close to 100 % correct). Their study also concluded that speech intelligibility in noise was better, although statistical significance could not be fully established. They postulated that a more sensitive speech in noise test might be able to establish a more definitive conclusion. The patients in the study by Garin et al. underwent a mean duration of 37 months between implantations. In contrast, our patients had a mean of 6 months between AMEI implantations.
Saliba et al. investigated the use of a VSB together with a contralateral digital hearing aid [2]. They found improved functional gain and speech perception thresholds in quiet, especially when the sound was presented from the front. However, they concluded that the use of the VSB middle ear implant together with a contralateral conventional hearing aid did not significantly improve hearing in noise. According to the patients’ responses to the APHAB (Abbreviated Profile of Hearing Aid Benefit test), most of the improvement was seen in the “ease of communication” score, which aims to identify problems in overall communication ability in good listening conditions.
Noble and Gatehouse found that in more challenging speech hearing contexts (multi-stream and rapidly switching speech streams), bilateral hearing aids offered more subjective benefit than unilateral. Patients who used two HAs aids also reported improved perception of distance as well as movements of objects and people. In addition, the subjects observed that listening required less effort when using two hearing aids compared with just one [10].
In a review of subjective benefit in regard to unilateral and bilateral fitting, Noble also reported that the patients preferred bilateral hearing aid usage [11].
Furthermore, Wolframm et al. evaluated speech understanding in noise by comparing signal-to noise ratios for 50 % correct word understanding using an omnidirectional and a directional microphone audio processor (AP) in four different noise conditions. They then compared the patients’ subjective speech comprehension, spatial hearing abilities and qualitative performance with the 2 different APs [12]). They observed immediate benefit and significantly improved speech comprehension in noise with the directional microphone AP when compared with the omnidirectional AP.
To date, bilateral AMEI have not been widely promoted largely due to the additional cost of the second implant as well as lack of published evidence to document necessity. This study serves to provide an initial glimpse into the benefit that can be offered to patients with conductive, mixed or sensorineural hearing impairment through bilateral implantation with an AMEI, although long-term analysis with a larger subject pool is warranted.
Conclusion
Globally there has been an increasing trend over the last two decades toward bilateral implantation for patients with severe to profound hearing loss. More than 25 % of children implanted younger than 3 years have received bilateral implants worldwide [13].
Bilateral hearing aids are particularly recommended for elderly people who suffer from presbyacusis. Holmes concluded that improved speech perception and localization abilities, increased relief from tinnitus and prevention of auditory deprivation are strong arguments for fitting two hearing aids [14].
AMEIs such as the VSB help patients with high-frequency hearing loss, occlusion or distortion problems, as well as other medical problems preventing permanent hearing aid usage. Bilateral VSBs can help to reduce problems in background noise and restore directional hearing.
Since the initial conclusion of this study, 20 more patients have been bilaterally implanted with the VSB in our center. We plan to publish long-term results with the inclusion of these patients in the future. The fact that our patients who have been implanted on one side request a second VSB shows us that they are very satisfied with their amplification. It seems that they miss the bilateral hearing effect. Long-term results may point to bilateral implantation as a routine part of clinical practice.
References
Ricketts T, Lindley G, Henry P (2001) Impact of compression and hearing aid style on directional hearing aid benefit and performance. Ear Hear 22:348–361
Saliba I, Calmels MN, Wanna G et al (2005) Binaurality in middle ear implant recipients using contralateral digital hearing AIDS. Otol Neurotol 26:680–685
Garin P, Schmerber S, Magnan J et al (2010) Bilateral vibrant soundbridge implantation: audiologic and subjective benefits in quiet and noisy environments. Acta Otolaryngol 130:1370–1378
Stern RM Jr, Colburn HS (1978) Theory of binaural interaction based in auditory-nerve data. IV. A model for subjective lateral position. J Acoust Soc Am 64:127–140
Boheim K, Mlynski R, Lenarz T et al (2012) Round window vibroplasty: long-term results. Acta Otolaryngol 132:1042–1048
Beleites T, Neudert M, Beutner D et al (2011) Experience with vibroplasty couplers at the stapes head and footplate. Otol Neurotol 32:1468–1472
Wagener K, Brand T, Kollmeier B (1999) Enwicklung und evaluation eines Satztests für die deutsche Sprache 38(2):44–56
Wagener K, Brand T, Kollmeier B (1999) Enwicklung und evaluation eines Satztests für die deutsche Sprache 38(3):86–95
Bronkhorst AW, Plomp R (1988) The effect of head-induced interaural time and level differences on speech intelligibility in noise. J Acoust Soc Am 83:1508–1516
Noble W, Gatehouse S (2006) Effects of bilateral versus unilateral hearing aid fitting on abilities measured by the Speech, Spatial and Qualities of Hearing Scale (SSQ). Int J Audiol 45(2):172–181
Noble W (2006) Bilateral hearing aids: a review of self-reports of benefit in comparison with unilateral fitting. Int J Audiol 45(1):S63–S71
Wolframm MD, Giarbini N, Streitberger C (2012) Speech-in-noise and subjective benefit with active middle ear implant omnidirectional and directional microphones: a within-subjects comparison. Otol Neurotol 33:618–622
Peters BR, Wyss J, Manriqe M (2010) Worldwide trends in bilateral cochlear implantation. Laryngoscope 120:17–44. doi:10.1002/lary.20859
Holmes AE (2003) Bilateral amplification for the elderly: two aids better than one? Int J Audiol 42:2S63–2S67
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors disclose that there is no conflict of interest.
Financial disclosure
All authors declare that neither financial interests nor financial support by companies exists. Furthermore, there are no financial interests the author may have in companies or other entities that have an interest in the information in the Contribution. All authors declare that the manuscript has not been published previously nor is it under review by another journal. The paper has not been presented to any professional society.
Rights and permissions
About this article
Cite this article
Wolf-Magele, A., Koci, V., Schnabl, J. et al. Bilateral use of active middle ear implants: speech discrimination results in noise. Eur Arch Otorhinolaryngol 273, 2065–2072 (2016). https://doi.org/10.1007/s00405-015-3783-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3783-6