Abstract
Excision has been the treatment of choice in benign non-tumorous obstructive disorders of the major salivary glands, when symptoms persisted in spite of conservative measures. Unfortunately surgical resection has been associated with a relatively high rate of adverse effects. To meet the need for a less invasive treatment modality for benign obstructive non-tumorous disorders (i.e., salivary stones or stenosis), sialendoscopy has been developed and implemented in several countries here among Denmark. This study is a 13-year retrospective registry-based study using The Danish National Patient Register. ICD-10 codes used for non-tumorous obstructive disease of the salivary glands were identified and used to extract patients potentially eligible for sialendoscopy in order to compare sialendoscopic surgery and extirpations of salivary glands. In 2012 sialendoscopy accounted for almost 20 % of all surgical interventions on the major salivary glands due to benign non-tumorous disease. Nationally and regionally the total number of resected major salivary glands due to benign obstructive disease also decreased significantly during the study period. A positive outcome, like the ones described here, will inspire further development and dissemination of gland preserving techniques, to great benefit for the patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
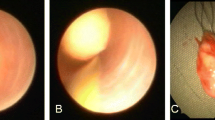
Excision has been the treatment of choice in benign non-tumorous obstructive disorders of the major salivary glands, when symptoms persisted in spite of conservative measures. Unfortunately surgical resection has been associated with a relatively high rate of adverse effects (Table 1) [1–4]. It is important to retain function of the major salivary glands, as saliva is essential for oral health, speech, digestion and quality of life [5]. To meet the need for a less invasive treatment modality for benign obstructive non-tumorous disorders (i.e., salivary stones or stenosis), sialendoscopy has been developed and implemented in several countries over the past 20 years [6, 7]. The method has been refined and improved; the results have been encouraging, as the rate of adverse effects is very low and patients satisfaction high [6, 8, 9]. The procedure was introduced in Denmark in 2004, and can be combined with surgical incision of the salivary duct when indicated; a so-called combined approach. To assess the impact on the number of excised salivary glands a large registry-based study was carried out. In other words, we wanted to know how many salivary glands were possibly saved using these gland preserving techniques.
Methods
Every Danish citizen is at birth provided with a unique social security number enabling valid data collection to the Danish registries and even cross linkage between Danish civil registration systems [10]. This study is a 13-year retrospective registry based study using The Danish National Patient Register (‘Landspatientregisteret’). The registry includes information on hospital discharges (since 1977) and on outpatient visits (since 1995) from hospitals in Denmark (population 5.5 million). Patient-specific data include departments, contact dates, hospital names and diagnoses coded according to the Danish version of the International Classification of Diseases (ICD), 8th revision from 1977 to 1993 and 10th revision from 1994 onwards. Furthermore all surgical procedures are coded in the registry using a Danish version of “Nordic Classification of Surgical Procedures (NCSP)” also called NOMECO. This coding system, however, does not contain information on which gland was operated on using sialendoscopy. In this study, we collected data on males and females of all ages in the period from 2000 to 2012. The ICD-10 codes used for non-tumorous obstructive disease of the salivary glands were identified and used to extract patients potentially eligible for sialendoscopy to compare sialendoscopic surgery and extirpations of salivary glands (Table 2). Patients suffering from malignant disease were excluded.
Regarding sialendoscopy, the study focused both on the whole country, and on the areas where the nearest Department of Oto-Rhino-Laryngology introduced sialendoscopy in the study period.
In Denmark registration of the above mentioned data from every hospital is required to receive reimbursement from the state. Thus, the data are reliable.
Microsoft Excel for Windows 8 and STATA version 13 were used for data analysis. A p value <0.05 was considered statistically significant. Two-sample t test with equal and unequal variances was used for comparative statistics.
Ethics statement
This study was approved by the Danish Data Protection Agency [11]. In Denmark, registry studies need not be approved by an ethics committee. The study was conducted according to the principles expressed in the Declaration of Helsinki [12].
Results
In the study period 2000–2012, the total number of surgical procedures performed on the major salivary glands—with all indications excluding malignant disease—increased by 31 %. However, the proportion of surgical interventions due to flow problems (i.e. stone or stenosis) remained stable around 20–25 % (Fig. 1). Sialendoscopy was introduced in Denmark in 2004. From 2004 to 2012, the total number of endoscopic interventions of the major salivary glands steadily increased to 143 per year. In 2012, sialendoscopy accounted for almost 20 % of all surgical interventions on the major salivary glands due to benign non-tumorous disease (Fig. 2). Eight hospitals implemented sialendoscopic surgery in the study period. Looking specifically at these, it is observed that the decrease in average number of excised glands per year is highly significant; from 2004 to 2012 a 26 % reduction compared to the previous five years was observed (p = 0.0149, CI 7.583–43.116). This means that in those eight hospitals more than 200 salivary glands were potentially preserved due to sialendoscopy and other minimally invasive techniques. Nationally the total number of resected major salivary glands due to non-tumorous obstructive disease also decreased significantly during the study period—dropping from a mean of 158 resected glands per year in 2000–2004, to a mean of 117 glands per year in 2005–2012 (p = 0.0004, CI 22.915–59.884). This extrapolates to a total of 329 major salivary glands spared nationally since sialendoscopy and other gland sparing techniques were introduced in Denmark. It was primarily submandibular gland resections that contributed to the over-all decrease both regionally and nationally (Fig. 3). However, a significant decrease in partial or total resections of the parotid gland was also observed (p = 0.017, CI −2.1709 to −0.2183). The mean number of resected glands was 11 in the pre-sialendoscopy period and 7 after the introduction of sialendoscopy. Therefore, the contribution to the decrease is rather low.
The decrease of excised submandibular and parotid glands due to benign non-tumorous obstructive pathology and the increase of sialendoscopic procedures in Denmark in the study period. The decrease of the average number of excised glands per year before and after introduction of sialendoscopy is highly significant. To illustrate the effect of the introduction of sialendoscopy, the specific decrease in number of excised glands has been shown for the Copenhagen region, where the procedure was first introduced and still is most prevalent
To illustrate the effect of the introduction of sialendoscopy in a single hospital, the decrease in resected major salivary glands has been shown (Fig. 3). The number of excised submandibular glands decreased with 73 % and the number of excised parotid glands decreased with 87.5 %. The decrease in excised submandibular glands matches that of the nationwide decrease (74.3 %), but in Copenhagen region the decrease in excised parotid glands was much more prominent (87.5 %) than nationwide (67.2 %).
The number of endoscopic salivary stone removals increased in the period; however, in 2011–2012 we observed a decrease in endoscopic stone fragmentation (Fig. 4). The number of conventional stone removals (dilatation and slitting of the first part of the salivary duct to a maximum of 2.5 cm without the use of the sialendoscope) was stable in the study period. Thus, the overall stone removal rate of the major salivary glands increased in Denmark over the past 13 years.
With regard to the overall rise in surgery on the major salivary glands (benign indications), the procedures mainly contributing to the increase were extirpations due to non-malignant tumors (i.e., Warthins tumor and pleomorphic adenoma) and biopsies on the salivary glands. Both procedures are unrelated to sialendoscopy and will not be discussed in detail.
Discussion
Obstructive diseases of the major salivary glands have long been a challenge to the otolaryngologist and his patients. The natural history of a patient suffering from salivary stones was vividly described by an American surgeon in 1904. The patient in this 14 pages long case report suffered from multiple salivary stones of a submandibular gland over a course of 28 years. He ended up with an extensive neck infection. In a rather risky surgical procedure, the surgeon removed the submandibular gland dissecting his way through much scar tissue. In the process, he came across the marginal nerve causing reversible nerve damage [13]. In the last paragraph, the surgeon outlines the treatment regimen for salivary stones, which has been standing until about 20 years ago; “…submaxillary or sublingual gland (…) must be reached from the outside. If a single calculus is found (…) the calculus can be removed and the gland left. If the calculi are multiple and difficult to remove (…), it is well to extirpate the gland. In case of calculus of the parotid gland, incision, removal of the calculus and drainage are, of course, all that could be done” [13]. However, as illustrated well in this reference and in more recent papers, the excision of salivary glands holds a noticeable risk of causing adverse effects, i.e., nerve damage, scar tissue problems and dry mouth, so a new approach was urgently needed [1, 2, 14].
Some of the first endoscopic procedures in otolaryngology area were reported in scientific journals around 1920 and ever since then, the techniques have been evolving fast [15]. In the mid-nineties a new diagnostic and interventional method—sialendoscopy—was developed; it proved more gentle on the salivary gland tissue, and could in some cases be performed using local anesthetics [7, 16]. Ever since, the method has been improving. More miniature surgical instruments (i.e., baskets, forceps, high-quality fiberoptic endoscopes, laser probes and guidewires) have been introduced and the method is more widespread [3, 16, 17]. Results are promising and patient satisfaction is high [18–20]. In Denmark, the unique social security number enables scientists to track patients through different public registries in a valid way, and extract patient groups of a certain interest. Doing just that we have found that in the study period from 2000 to 2012, there has been an overall increase of surgical procedures on the major salivary glands; especially with regard to partial and total resection of the parotid gland due to non-malignant tumors. We ascribe this to an increased awareness of ‘tumors’ as potential cancers, rendering patients with, i.e., Warthins tumors less likely to want an observational strategy rather than a surgical one. The main objective of this study is to assess whether the introduction of the gland sparing concept has saved any major salivary glands from excision. This is indeed the case, as a decrease in excision rate of 26 % was observed in the study period. In 2011 and 2012, the lowest number of submandibular glands was excised since 2000. Hopefully this development will continue (Fig. 3). Both on a national and regional basis, the decrease in excised glands was significant. This shows that hospitals which do not perform sialendoscopy locally, to some extent refer patients to hospitals that do, instead of excising the affected gland in-house.
Usually the parotid gland will not be resected due to flow problems (i.e., stone or stenosis), as the risk of facial nerve damage during this procedure is significant. This is also reflected in our data, but a significant decrease in parotidectomy was noted even though the total number of resections were rather low (Fig. 3). Patients suffering from benign obstructive non-tumorous pathology of the parotid gland now have an efficient and gland preserving treatment option in sialendoscopy with fewer complications. Fine results in this patient category have been noted in the literature, both using sialendoscopy alone and in combination with surgical incision [20–22]. The above-described results should, however, not be over-interpreted. The introduction of sialendoscopy is not the only explanation of the noted decrease in resected salivary glands. The tendency in otorhinolaryngology has generally changed towards a less invasive strategy to benefit the patient, and this should not be understated. The whole development of the sialendoscopic area is a witness of this changed approach. Furthermore studies regarding quality of life in patients, who have undergone removals of the large salivary glands, has emerged and underlined the need for more minimally invasive measures. Also our data suggest room for improvement, as there are still a substantial number of salivary glands excised throughout the country due to pathology which might be treated with sialendoscopy or other stone removing modalities such as transoral incision in the submandibular duct or hilus, or sialendoscopic assisted removal of stones in the parotid duct through the parotid gland. A large study from Iro et al. shows that salivary gland resection due to salivary stones can be reduced to as little as 3 % [23]. The gland sparing concept is still not implemented in all Danish Departments of Otorhinolaryngology and not all surgeons have a lot of experience with the procedure. This might hold some of the explanation to why the higher number of excised glands (Table 3).
The number of conventional stone removals has not significantly decreased in the study period. Patients managed by conventional means usually present with smaller anteriorly located salivary stones, which could easier be removed by dilatation and duct slitting. However, this means, that the total number of stone removals thus increased with the introduction of sialendoscopy and other gland preserving techniques; this is interpreted as being closely connected to the decline in salivary gland excisions, as these patients previously would have had their salivary glands excised due to large, multiple and/or posterior located stones. The number of endoscopic stone fragmentations decreased in 2011 and 2012, the reason for this might be a more frequent use of a combined approach using the sialendoscope to locate the salivary stone and then surgically remove the stone through an intra-oral incision [24]. This method is considered safe and is, in our experience, much less time consuming and considerable more successful than endoscopic stone fragmentation using laser [21, 24–26]. To our knowledge no other studies have been carried out to assess whether the introduction of sialendoscopy decreases the number of excised salivary glands. Thus, it is a true alternative to a more radical surgical approach to obstructive pathology of the major salivary glands. Multiple studies have proved the method safe and effective, rendering patients satisfied also on a long term basis [8, 27]. In our opinion, it is very important to further study whether sialendoscopy and the combined approach in reality saves the major salivary glands on a national basis in other countries. A positive outcome, like the ones described here, will inspire further development and dissemination of the method. This would be of great benefit to the patients and decrease the number of adverse effects caused by gland excision (Table 4).
Conclusion
The introduction of sialendoscopy and combined approach in Denmark has significantly contributed to the decreased number of excisions of the major salivary glands due to benign, non-tumorous obstructive pathology both regionally and nationally. This seems so far to have saved more than 300 submandibular glands from excision, and thus the patients have avoided possible concomitant adverse effects such surgical procedures might have.
References
Springborg LK, Møller MN (2013) Submandibular gland excision: long-term clinical outcome in 139 patients operated in a single institution. Eur Arch Otorhinolaryngol 270:1441–1446. doi:10.1007/s00405-012-2175-4
Hald J, Andreassen UK (1994) Submandibular gland excision: short- and long-term complications. ORL 56:87–91
Dabirmoghaddam P, Hosseinzadehnik R (2013) Interventional sialendoscopy with endoscopic sialolith removal without fragmentation. Indian J Otolaryngol Head Neck Surg 65:111–115. doi:10.1007/s12070-012-0573-y
Nahlieli O (2009) Endoscopic surgery of the salivary glands. Alpha Omegan 102:55–60
Gillespie MB, O’Connell BP, Rawl JW, et al (2014) Clinical and quality-of-life outcomes following gland-preserving surgery for chronic sialadenitis. Laryngoscope. doi:10.1002/lary.25062 (Epub ahead of print)
Danquart J, Wagner N, Arndal H, Homøe P (2011) Sialoendoscopy for diagnosis and treatment of non-neoplastic obstruction in the salivary glands. Dan Med Bul 58:A4232
Gundlach P, Hopf J, Linnarz M (1994) Introduction of a new diagnostic procedure: salivary duct endoscopy (sialendoscopy) clinical evaluation of sialendoscopy, sialography, and X-ray imaging. Endosc Surg Allied Technol 2:294–296
Rasmussen ER, Arndal H, Rasmussen SH, Wagner N (2012) Steady progress seen in endoscopic surgery on major salivary glands. Dan Med J 59:A4525
Koch M, Iro H, Künzel J et al (2012) Diagnosis and gland-preserving minimally invasive therapy for Wharton’s duct stenoses. Laryngoscope 122:552–558. doi:10.1002/lary.22452
Pedersen EG, Hallas J, Hansen K et al (2011) Identifying patients with myasthenia for epidemiological research by linkage of automated registers. Neuroepidemiology 37:120–128. doi:10.1159/000331481
Datatilsynet (2015) http://www.datatilsynet.dk/, http://www.datatilsynet.dk/
The World Medical Association (2013) http://www.wma.net, http://www.wma.net/en/30publications/10policies/b3/
Roberg O (1904) IV. Sialolithiasis. Ann Surg 39:669–682
Kauffman RM, Netterville JL, Burkey BB (2009) Transoral excision of the submandibular gland: techniques and results of nine cases. Laryngoscope 119:502–507. doi:10.1002/lary.20029
Tilley H (1918) A surgical contretemps, illustrating the value of endoscopy. Proc R Soc Med 11:73–74
Marchal F, Dulguerov P, Lehmann W (1999) Interventional sialendoscopy. N Engl J Med 341:1242–1243. doi:10.1056/NEJM199910143411620
Phillips J, Withrow K (2014) Outcomes of holmium laser-assisted lithotripsy with sialendoscopy in treatment of sialolithiasis. Otolaryngol Head Neck Surg 150:962–967. doi:10.1177/0194599814524716
Strychowsky JE, Sommer DD, Gupta MK et al (2012) Sialendoscopy for the management of obstructive salivary gland disease: a systematic review and meta-analysis. Arch Otolaryngol Head Neck Surg 138:541–547. doi:10.1001/archoto.2012.856
Matsunobu T, Kurioka T, Miyagawa Y et al (2014) Minimally invasive surgery of sialolithiasis using sialendoscopy. Auris Nasus Larynx 41:528–531. doi:10.1016/j.anl.2014.05.009
Ianovski I, Morton RP, Ahmad Z (2014) Patient-perceived outcome after sialendoscopy using the glasgow benefit inventory. Laryngoscope 124:869–874. doi:10.1002/lary.24343
Konstantinidis I, Chatziavramidis A, Iakovou I, Constantinidis J (2014) Long-term results of combined approach in parotid sialolithiasis. Eur Arch Otorhinolaryngol. doi:10.1007/s00405-014-3391-x (E-pub ahead of print)
Durbec M, Dinkel E, Vigier S et al (2012) Thulium-YAG laser sialendoscopy for parotid and submandibular sialolithiasis. Lasers Surg Med 44:783–786. doi:10.1002/lsm.22094
Iro H, Zenk J, Escudier MP et al (2009) Outcome of minimally invasive management of salivary calculi in 4691 patients. Laryngoscope 119:263–268. doi:10.1002/lary.20008
Juul ML, Wagner N (2014) Objective and subjective outcome in 42 patients after treatment of sialolithiasis by transoral incision of Warthon’s duct: a retrospective middle-term follow-up study. Eur Arch Otorhinolaryngol 271:3059–3066. doi:10.1007/s00405-014-2905-x
Klein H, Ardekian L (2014) The treatment of large sialoliths by sialendoscopic combined approach. J Oral Maxillofac Surg 72:737–743. doi:10.1016/j.joms.2013.09.003
Modest MC, Galinat L, Rabinowitz MR et al (2014) Learning progression in the use of sialendoscopy for sialolithiasis: effect on gland preservation. Otolaryngol Head Neck Surg 151:240–245. doi:10.1177/0194599814533658
Koch M, Künzel J, Iro H et al (2014) Long-term results and subjective outcome after gland-preserving treatment in parotid duct stenosis. Laryngoscope 124:1813–1818. doi:10.1002/lary.24534
Acknowledgments
The authors would like to thank Dr. Troels G. Nielsen and the Department of Otolaryngology, Head and Neck Surgery at Hilleroed Hospital to have supported this study financially.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare to have no conflicts of interests.
Rights and permissions
About this article
Cite this article
Rasmussen, E.R., Lykke, E., Wagner, N. et al. The introduction of sialendoscopy has significantly contributed to a decreased number of excised salivary glands in Denmark. Eur Arch Otorhinolaryngol 273, 2223–2230 (2016). https://doi.org/10.1007/s00405-015-3755-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3755-x