Abstract
Snoring is usually caused by the vibration of walls of the soft palate at the pharyngeal level. Its worldwide prevalence is estimated to range between 2 and 85 % depending on age, gender or population group. The aim of this study is to determine the degree of improvement that can be subjectively evident in patients treated by snoring with radiofrequency-assisted uvulopalatoplasty based on a one-session protocol. This is a prospective, longitudinal, non-randomized study. Patients of both sexes, aged 18 years, who attended to the ENT consultation in a tertiary hospital with snoring during the period of July 2012–July 2013 were included. Age, body mass index, Epworth sleepiness scale were calculated. The volume of snoring of each subject was assessed using a visual analog scale. A total of 27 patients were included in the study; the average age of the sample was 49 years (±8.7; min 36/max 74); of these 22 (81.5 %) were male and 5 (18.5 %) females. The average BMI was 27.07 ± 2.5 (min 23.15/max 29.39) before the test and after 1 year was 26.75 ± 2.32 (min 23.11/max 29.56) with no statistically significant differences in BMI before and after surgery (p = 0.407). Preoperative snoring intensity was 8.10 ± 0.93 according to VAS. We found a statistically significant difference in the post-operative intensity at 3 months of 3.93 ± 0.88 (p ≤ 0.05) at 6 months of 4.41 ± 1.08 (p ≤ 0.05), and after 1 year 4.90 ± 0.77 (p ≤ 0.05). The average rate of ESS was significantly higher preoperatively than post-operative, being 8.76 ± 3.1 preoperative and 6.93 ± 1.68 post-operative (p ≤ 0.05). We conclude that the use of radiofrequency in simple snorers with an apnea/hypopnea index <15 events per hour and a BMI < 30 kg/m2 in whom clinically proven that the source of snoring is the soft palate, can be treated by one-session protocol, being possible to obtain an improvement of snoring up to 70 % of cases by a short follow-up period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Snoring is usually caused by the vibration of walls of the soft palate at the pharyngeal level [1]. Its worldwide prevalence is estimated to range between 2 and 85 % depending on age, gender or population group [2].
Since Fujita et al. [3] introduced the uvulopalatoplasty in 1981, multiple techniques have been added to the armamentarium for the management of snoring. In 1990, Kamami [4] introduced CO2 laser-assisted uvulopalatoplasty. Later in 1998, Powell et al. [5] described the volumetric reduction of the soft palate with radiofrequency, and in 2002 Wedman and Miljeteig [6] introduced the radiofrequency-assisted uvulopalatoplasty (RAUP).
The utility of RAUP and its positive effects on snoring have recently been demonstrated [7]. In turn, the ease with which it is possible to do, low cost involved, low rate of complications and less post-operative pain compared with other techniques, has greatly increased its popularity today. However, most studies concerned need an average of 1.8–5 sessions to obtain a significant results on snoring [7, 8], and evidence exists that these effects may decrease over time [9].
For these reasons, the aim of this study is to determine the degree of improvement that can be subjectively evident in patients treated by snoring with RAUP based on a one-session protocol.
Materials and methods
Design
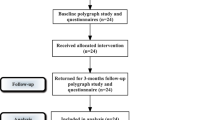
This is a prospective, longitudinal, non-randomized study. Patients of both sexes, aged 18 years, who attended to the ENT consultation in a tertiary hospital with snoring during the period of July 2012 to July 2013 were included. This study was approved by the ethics committee of our hospital and was conducted according to the principles of the Declaration of Helsinki.
Participants
Prior to surgery, the medical history, Epworth sleepiness scale (ESS) preoperative and post-operative at 6 months, body mass index (BMI) and a complete ENT evaluation were conducted. Those patients who underwent a polysomnography and had an apnea/hypopnea index <15 events per hour, with a BMI < 30 kg/m2 (simple snoring), in which by physical and flexible nasopharyngoscope examination, evaluating two levels of the pharynx (retrovelar and retroglossal), the soft palate was considered as a possible source of snoring, and confirmed posteriorly by the Müller maneuver, were included. Patients with obesity (BMI > 30 kg/m2), macroglossia (Friedman tongue position >4), nasal obstruction, mandibular insufficiency, tonsillar hypertrophy (Friedman tonsil size >3), severe gastroesophageal reflux, retrognathia, craniofacial abnormalities, hematologic disorders, allergy to topical anesthesia or cardiovascular disease were excluded.
Subjective assessment of snoring
The volume of snoring of each subject was assessed using a visual analog scale (VAS) from 0 to 10, applied to the couple or bed partner of the patient, where 0 is no snoring and 10 is the maximum volume snoring. Also applied to the couple was a subjective test in which the response is based on four variables, overall, satisfied, partially satisfied or not satisfied improvement.
Anesthesia
All procedures were performed under local anesthesia. A lidocaine spray 10 % (Xylocaine®) was applied, 2–4 sprays on two occasions and once the gag reflex was abolished, a mixture of lidocaine (2 %) + epinephrine (1/100,000) was infiltrated with a 24G dental syringe in the soft palate, uvula and palatoglossal pillars.
Surgical procedure
The procedure was performed on an outpatient basis, the room was prepared for possible contingencies, and was performed by two senior consultants. Vital signs (HR, BP, SatO2) were monitored. The patient was seated in a comfortable position, facing the surgeon. Later, 20 min after infiltration, six punctures were performed with a power of 14 W, one in the central portion of the soft palate approximately 1 cm below the junction with the hard palate, two towards both palatoglossal pillars, two in the lateral side to the midline and one on the uvula insertion through the azygous muscle of the uvula and towards the tip. The equipment used was a CelonLab® device (Olympus Corporation, Tokyo, Japan). Bipolar energy application was conducted by an average of 6–10 s, according to the manufacturers’ specifications, with the completion time of this application characterized by an acoustic alarm.
Analgesia and other complications
After surgery, patients were discharged with a protocol of analgesia with NSAIDs (Ibuprofen 600 mg × 3 times daily) ± opioid analgesic only if the pain did not improve after taking the NSAIDs. At 7 days after surgery, patients were consulted by telephone about post-operative pain. Pain was rated using visual analog scale (VAS) with 0 being the least pain and 10 the worst possible pain experienced. In turn, the need for other types of analgesics or sedatives was consulted. Other complications such as pharyngeal foreign body sensation, nasal reflux, nasal voice, taste changes, ulceration or perforation of the soft palate and bleeding were assessed in subsequent revisions.
Statistical analysis
Statistical analysis was performed using SPSS 20.0 for Windows (SPSS Inc., IL, USA). Quantitative and qualitative variables in the study are expressed as mean ± standard deviation. A comparison of the snoring volume, ESS and BMI before and after surgery was performed using the “t Student test” for paired data.
Results
A total of 27 patients were included in the study; the average age of the sample was 49 years (±8.7; min 36/max 74); of these 22 (81.5 %) were male and 5 (18.5 %) females. There were no statistical differences in epidemiological parameters in this study. The follow-up period was 12.6 ± 1.8 months (range 12–15 months). The average BMI was 27.07 ± 2.5 (min 23.15/max 29.39) before the test and after 1 year was 26.75 ± 2.32 (min 23.11/max 29.56) with no statistically significant differences in BMI before and after surgery (p = 0.407) (Table 1).
Preoperative snoring intensity was 8.10 ± 0.93 according to VAS. In assessing the post-operative intensity, we found a statistically significant difference in the post-operative intensity at 3 months of 3.93 ± 0.88 (p ≤ 0.05) at 6 months of 4.41 ± 1.08 (p ≤ 0.05), and after 1 year 4.90 ± 0.77 (p ≤ 0.05) (Table 2).
As for the subjective scale of satisfaction applied to the roommates, 17 (62.9 %) reported an overall improvement of snoring; other 5 (18.51 %) patients reported they were satisfied with the results; and other 2 (7.40 %) reported partially satisfied. However, another 3 (11.1 %) male patients did not have any sign of improvement after surgery. Subsequently, two patients on the satisfied group and three patients of the partially satisfied group experienced recurrence of snoring similar to pre-surgical levels. In these 5 (18.51 %) patients (two patients on the satisfied group and three patients of the partially satisfied group) was considered relapse treatment, and in the three patients that did not have any sign of improvement and it was necessary to repeat the treatment.
The average rate of ESS was significantly higher preoperatively than post-operative, being 8.76 ± 3.1 preoperative and 6.93 ± 1.68 post-operative (p ≤ 0.05).
Evaluating the average of pain experienced during the first week after treatment, this was 3.75 ± 0.93. 24 (88.8 %) of the patients reported good pain control by taking Ibuprofen 600 mg every 8 h, another 3 (11.1 %) needed to associate taking an opioid to achieve pain palliation. During the successive revisions made after the procedure, patients were questioned about the presence of complications; 3 (11.1 %) patients reported episodes of muscular contraction of the wound. No other complication was reported (Table 3).
Discussion
Snoring is due to a combination of a narrowed pharyngeal airway and redundant vibratory tissues. The soft palate, including the uvula, has been reported to be the primary vibratory tissue in 70 % of cases [10]. And it depends highly on outer variables such as alcohol intake, sleep position, and tiredness.
Simple snoring refers to continuous or intermittent sound of varying intensity, generated by the vibration of the pharyngeal walls during sleep, without being accompanied by episodes of apnea. It is usually a condition associated with significant medical problems such as hypertension, angina or stroke compared with non-snorers [11, 12]. Besides, the simple snoring increases the risk of OSAS, and an early intervention over this is associated with a decrease in this risk [13]. Snoring is also a frequent cause of problems at home because of how uncomfortable it can mean for roommates snoring intensity.
Since Fujita [3] describes the uvulopalatopharyngoplasty, multiple efforts have been aimed to describe new methods that would be able to improve outcomes and reduce comorbidities and technical difficulties that this represents. From these efforts and work, Wedman and Miljeteig [6] describe the RAUP technique, and since then this has been gaining popularity due to their advantages in terms of less pain, less risk of post-operative complications and bleeding among others. Recently, Virk et al. [14] in a study of the local effects of radiofrequency conducted in tonsils, described the effect of this lesion as an oval character of 6.7 mm wide by 7–8 mm length.
In our study, we have managed to achieve a margin of reduced snoring with clinical and statistical significance in up to 70.3 % of patients, of which 17 (62.9 %) reported complete disappearance of snoring. But several definitions for success or for efficacy of the treatments about snoring exist. Efficacy can be defined as a significant decrease of snoring volume, in some studies under an arbitrary level, and in others by a cessation. And success can be related to the bed partner’s satisfaction with no regard to the snoring volume’s intensity [15]. In patients treated by laser-assisted uvulopalatoplasty, Mauw and Marsan used a VAS from 0 to 10, with 10 being the preoperative snoring volume. They measured a reduction of snoring volume; results were considered excellent when the final score was between 0 and 2 and satisfactory if it was between 3 and 5 [16]. Astor et al. used VAS from 0 to 7. Success was defined as the patient’s initial score dropping 3 points or more and the final snoring score being 3 or less. Cessation of snoring was defined as a final score of 2 or less and the level of snoring was agreeable to the family. Failure was defined as “a snoring score of more than 3 or the patient verbalized dissatisfaction” [17]. And Blumen et al. [15] considered as a success a significant decrease in the snoring volume in the range of normal breathing or loud respiration associated with the bed partner’s satisfaction.
The ESS is a simple and economical questionnaire which is answered by the patient and subjectively estimate the level of daytime sleepiness a person may experience. Although their results may be influenced by several variables, they can be used as an evaluation parameter in the treatment of simple snoring [13, 18]. In this study, the rate of daytime sleepiness Epworth statistically significantly decreased after treatment parameter, which could be associated at least subjectively with decreased risk of OSA in the future; however, this conclusion should be confirmed by more rigorous and lengthy studies in time.
Some studies report that one of the factors affecting short-term results of RAUP’s is the BMI [19, 20]. Apart from this, the weight gain is also considered a risk factor for recurrence of snoring [21]. In our study, each patient was advised to reduce weight to improve the post-surgical outcomes. Though not all of the patients complete the recommendations, a slight decrease in weight in the whole sample was evident, without statistical significance.
The short-term efficacy of RAUP has been demonstrated in several studies, including a meta-analysis [18], but one problem that usually occurs frequently in patients treated by RAUP is the risk of recurrence, which can range from 11 to 41 % depending on the follow-up period of each study [7, 9, 18, 22, 23]. Recently, De Kermadec et al. [24] published a retrospective study that evaluated during 6-year follow-up of 77 patients treated by RAUP, in which they showed up to 92.7 % of recurrence of snoring. In our study, 18.51 % of patient had recurrence of snoring during the follow-up period, consistent with the data presented in the literature for similar follow-up periods, and lower than those reported by De Kermadec et al., probably due to the short follow-up period of our study.
Regarding complications, the post-operative bleeding, infection, fistula of the soft palate, velo-palatal insufficiency, altered taste sensation and muscle tightness across the scar are described in the literature [7, 9]. In our study, only 3 (11.1 %) patients had some type of complication, and in all 3 cases corresponded to muscle contracture of the surgical wound. The post-operative period was well tolerated by 88.8 % of patients, pain and just only 3 (11.1 %) patients had to take an analgesic opioid type not showing improvement of pain with NSAIDs.
But our study has a number of limitations, primarily the lack of control group and the small sample size limit the validity of our results; second would be the short follow-up period (12.6 months), as the trend demonstrated in longer studies would for recurrence; and thirdly, the subjective nature of the assessment of improvement in the snoring. Probably new and more objective methods (sound pressure, duration of snoring, frequency bands, among others) could help in future studies to determine more precisely the improvement of this condition with the different therapeutic tools that exist today.
Conclusion
We conclude that the use of RAUP in simple snorers with an apnea/hypopnea index <15 events per hour and a BMI < 30 kg/m2 in whom clinically proven that the source of snoring is the soft palate and in the absence of nasal obstruction or base of tongue hypertrophy, can be treated by one-session protocol, being possible to obtain an improvement of snoring up to 70 % of cases by a short follow-up period. However, we must note that we can not always predict which cases will go better; for this reason, further studies with a longer period of follow-up and more patients are needed to determine whether these results are maintained over time.
References
De Vito A, Frassineti S, Panatta ML, Montevecchi F, Canzi P, Vicini C (2012) Multilevel radiofrequency ablation for snoring and OSAHS patients therapy: long-term outcomes. Eur Arch Otorhinolaryngol 269(1):321–330
Bouscoulet LT, Vázquez-García JC, Muiño A, Márquez M, López MV, de Oca MM et al (2008) Prevalence of sleep related symptoms in four Latin American cities. J Clin Sleep Med 4(6):579–585
Fujita S, Conway W, Zorick F, Roth T (1981) Surgical correction of anatomic abnormalities in obstructive sleep apnea syndrome: uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 89(6):923–934
Kamami YV (1990) Laser CO2 for snoring. Preliminary results. Acta Otorhinolaryngol Belg 44(4):451–456
Powell NB, Riley RW, Troell RJ, Li K, Blumen MB, Guilleminault C (1998) Radiofrequency volumetric tissue reduction of the palate in subjects with sleep-disordered breathing. Chest 113(5):1163–1174
Wedman J, Miljeteig H (2002) Treatment of simple snoring using radio waves for ablation of uvula and soft palate: a day-case surgery procedure. Laryngoscope 112(7 Pt 1):1256–1259
Bäck LJ, Hytönen ML, Roine RP, Malmivaara AO (2009) Radiofrequency ablation treatment of soft palate for patients with snoring: a systematic review of effectiveness and adverse effects. Laryngoscope 119(6):1241–1250
Johnson JT, Pollack GL, Wagner RL (2002) Transoral radiofrequency treatment of snoring. Otolaryngol Head Neck Surg 127(3):235–237
Stuck BA (2009) Radiofrequency-assisted uvulopalatoplasty for snoring: long-term follow-up. Laryngoscope 119(8):1617–1620
Quinn SJ, Daly S, Ellis PMD (1995) Observation of the mechanism of snoring using sleep nasoendoscopy. Clin Otolaryngol 20:360–364
Koskenvuo M, Kaprio J, Partinen M, Langinvainio H, Sarna S, Heikkilä K (1985) Snoring as a risk factor for hypertension and angina pectoris. Lancet 1(8434):893–896
Koskenvuo M, Kaprio J, Telakivi T, Partinen M, Heikkilä K, Sarna S (1987) Snoring as a risk factor for ischaemic heart disease and stroke in men. Br Med J (Clin Res Ed) 294(6563):16–19
Lim DJ, Kang SH, Kim BH, Kim HG (2007) Treatment of primary snoring using radiofrequency-assisted uvulopalatoplasty. Eur Arch Otorhinolaryngol 264(7):761–767
Virk JS, Kumar G, Al-Okati D, Kotecha B (2014) Radiofrequency ablation in snoring surgery: local tissue effects and safety measures. Eur Arch Otorhinolaryngol. doi:10.1007/s00405-014-3152-x
Blumen MB, Dahan S, Wagner I, De Dieuleveult T, Chabolle F (2002) Radiofrequency versus LAUP for the treatment of snoring. Otolaryngol Head Neck Surg 126(1):67–73
Mauw J, Marsan J (1997) Uvulopalatopharyngoplasty versus laser assisted uvulopalatopharyngoplasty in the treatment of snoring. J Otolaryngol 26:232–235
Astor FC, Hanft KL, Benson C et al (1998) Analysis of short-term outcome after office-based laser-assisted uvulopalatoplasty. Otolaryngol Head Neck Surg 118:478
Stuck BA, Verse T, Hein G, Hormann K, Maurer JT (2004) Radiofrequency surgery of the soft palate in the treatment of snoring—a review of the literature. Sleep 27:551–555
Pessey JJ, Rose X, Michenet F, Calmels MN, Lagleyre S (2005) Treatment of simple snoring by radiofrequency velar coblation. Ann Otolaryngol Chir Cervicofac 122(1):21–26
Trotter MI, D’Souza AR, Morgan DW (2002) Medium-term outcome of palatal surgery for snoring using the Somnus unit. J Laryngol Otol 116(2):116–118
Neruntarat C (2001) Laser-assisted uvulopalatoplasty: short-term and long-term results. Otolaryngol Head Neck Surg 124(1):90–93
Li KK, Powell NB, Riley RW, Troell RJ, Guilleminault C (2000) Radiofrequency volumetric reduction of the palate: an extended follow-up study. Otolaryngol Head Neck Surg 122(3):410–414
Said B, Strome M (2003) Long-term results of radiofrequency volumetric tissue reduction of the palate for snoring. Ann Otol Rhinol Laryngol 112(3):276–279
De Kermadec H, Blumen MB, Engalenc D, Vezina JP, Chabolle F (2014) Radiofrequency of the soft palate for sleep-disordered breathing: a 6-year follow-up study. Eur Ann Otorhinolaryngol Head Neck Dis 131(1):27–31
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiesa Estomba, C.M., Rivera Schmitz, T., Ossa Echeverri, C.C. et al. The treatment of snoring by radiofrequency-assisted uvulopalatoplasty and results after one-session protocol: a prospective, longitudinal, non-randomized study. Eur Arch Otorhinolaryngol 272, 3059–3063 (2015). https://doi.org/10.1007/s00405-015-3617-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-015-3617-6