Abstract
Typically, the medial orbital wall contains an anterior ethmoidal foramen (EF) and a posterior EF, but may also have multiple EFs transmitting the arteries and nerves between the orbit and the anterior cranial fossa. The aim of this study is to determine a patient-friendly landmark of the medial orbital wall and to specify a precise location of the ethmoidal foramens (EF) in order to standardize certain anatomical marks as safe ethmoidal arteries. Orientation points on the anterior ethmoidal foramen (AEF), posterior ethmoidal foramen (PEF) and middle ethmoidal foramen (MEF) were investigated in 262 orbits. Using a software program, distances between each foramen and the midpoint of the anterior lacrimal crest (ALC), the optic canal (OC), and some important angles were measured. The EFs were identified as single in 0.8 %, double in 73.7 %, triple 24,4 % and quadruple in 1.1 % specimens. The mean distances between ALC and AEF, ALC and PEF and ALC and MEF were 27.7, 10.6, and 12.95 mm, respectively. The distances from ALC–AEF, AEF–PEF, and PEF-OC were 27.7 ± 2.8, 10.6 ± 3.3, 5.4 ± 1 mm. The angles from the plane of the EF to the medial border of the OC were calculated as 13.2° and 153°, respectively. The angle from the AEF to the medial border of the OC was based on the plane between the ALC and AEF was 132°. The occurrence of multiple EF with an incidence of 25 % narrows the borders of the safe region in the medial orbital wall. Safe distance of the ALC–EF was measured as 22.1 mm on medial wall. The line of the location of the EF was calculated 16.2 mm. In this study, it was possible to investigate the variability of the orbital orifice of the EF and the feasibility of the EA, to observe various angles of the orbital wall bones and to calculate the lengths of some parameters with the help of certain software.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ethmoidal foramens (EF) are small openings usually in the medial wall of the orbit, and lateral to the medial end of the optic canal (OC) [2, 3, 7, 17, 24, 28, 34]. Typically, the medial orbital wall contains an anterior ethmoidal foramen (AEF) and a posterior ethmoidal foramen (PEF), but may also have multiple EFs transmitting the arteries and nerves between the orbit and the anterior cranial fossa [9, 15, 28, 30–32].
The weakest point of the medial wall of the orbit is where the EF leaves the ethmoid surface of the orbit. It is this very point that the extremely thin bone provides the least resistance to surgical instruments [3, 13, 15, 26]. It is crucial to know the courses of the EA pre-operatively because when the EA, which normally has a bony coverage, freely transverses within the ethmoidal cells, it can be injured during procedures at the medial wall of the orbit [5, 22, 27–29].
In cases of surgeries, orbital decompression and endoscopic approaches, post-traumatic orbital reconstruction and anterior skull base reconstruction, anterior ethmoidal artery (AEA) or posterior ethmoidal artery (PEA) can be damaged [10, 21, 22, 28, 29, 34]. Injury to the EF may result in massive hemorrhage, orbital hematoma, blindness and optic neuropathy after the operation, unless the surgeon has mastered in terms of foraminal features [11, 19, 33, 34]. The reason of unexpected bleedings during orbital medial wall surgery is the cut, rupture or damage caused in the EA through EF [6, 10, 13, 15]. In some cases, knowing the location of the artery is life-saving [4, 5, 33].
Since the horizontal orientation of the EFs directly affects the surgical procedure, previous morphometric researches which were limited by the anatomical landmarks might have contained some misleading information. The aim of this study is to explain where bleeding occurs at certain anatomical points along the medial wall.
Materials and methods
In this study, the reference points of the AEF, PEF and MEF on the medial orbital wall were investigated in 262 orbits. None of the orbits was affected by the orbital abnormally or disrupted anatomically due to a previous orbital surgery or trauma.
Using the macro mode of a Nikon D 300 megapixel camera, photographs were taken in the aperture priority mode, with f7.1 diaphragm clarity. The skulls were fixed horizontally and the images were taken by fixing the camera 26 cm away from the orbital rim with help of a tripod set at an angle of 78° from the horizontal surface. The pictures were then uploaded onto a personal computer and software (last edition of National Institute of Health’s public software Image J 1.48v) was used to calculate the distance of the medial wall of the orbit (Fig. 1). With the software, the EF was chosen and its sizes, distances, angles, and relations with other anatomical structures were evaluated on right and left sides separately (Fig. 2a, b).
Measurements in the medial wall using Image J 1.47 version. ALC midpoint of the anterior lacrimal crest, AEF anterior ethmoidal foramen, PEF posterior ethmoidal foramen, MEF middle ethmoidal foramen, OC optic canal, circle shows result of measured angle, lines those are lines of software angle tool which is dark gray on tool bar due to selection, black arrows ethmoidal foramens
Measurements from the midpoint of the anterior lacrimal crest (ALC), AEF, PEF, MEF and the medial border of the OC were taken. The distances measured between two different points were as follows (Figs. 1, 2):
-
1.
The distance between the ALC and the AEF,
-
2.
The distance between the ALC and the PEF,
-
3.
The distance between the AEF and the PEF,
-
4.
The distance between the AEF and the MEF,
-
5.
The distance between the PEF and the OC,
-
6.
The distance between the MEF and the OC,
-
7.
The distance between the ALC and the OC,
-
8.
The angle between PEF–OC and OC–AEF,
-
9.
The angle between AEF–OC and OC–ALC,
-
10.
The angle between OC–PEF and PEF–AEF,
-
11.
The angle between PEF–AEF and AEF–OC,
-
12.
The angle between OC–AEF and AEF–ALC,
-
13.
The angle between AEF–ALC and ALC–OC.
Descriptive statistics (mean, minimum, maximum and standard deviation) were evaluated for all the parameters collected from dry skull measurements. Differences between the data of skull measurements were analyzed by Student’s t test. For all the analyses p < 0.05 was accepted as statistically significant, while p < 0.01 was accepted as highly significant.
The study was approved by a suitably constituted Ethical Committee at Ege University Hospital Researches Department, within which the work was undertaken, and the study conforms to the Declaration of Helsinki (14.04.2011).
Results
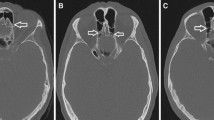
The observation of 262 orbits of dry adult human skulls showed that the EFs were as identified the medial wall of the orbit (Fig. 3a–d). The AEF, PEF and MEF were found to be located at various numbers (Fig. 3a–d).
Differences in the size of the ethmoidal foramen on the orbit. ALC midpoint of the anterior lacrimal crest, AEF anterior ethmoidal foramen, PEF posterior ethmoidal foramen, MEF middle ethmoidal foramen, OC optic canal, black arrows ethmoidal foramens. a Single, b double, c triple, d quadruple EF localized on the orbital wall
Out of 262 specimens, the EF followed a double-foramen pattern in 193 specimens (73.7 %); an AEF and a PEF were defined as a double-foramen pattern (Fig. 3b). Sixty-nine specimens (26.3 %) were demonstrated to have an anatomical variation pattern which consisted of a triple and a quadruple EF. Anatomical appearance of the EF occurred as a single EF in 2 cases (0.8 %) (Fig. 3a), 3 EFs in 64 cases (24.4 %) (Fig. 3c), and 4 EFs in 3 cases (1.1 %) (Fig. 3d).
The average distances between ACL and AEF, and PEF and OC were 27.7 ± 2.8, 36.6 ± 4, 41.4 ± 3.8 mm, respectively. The mean distances between AEF and MEF, MEF and PEF, and AEF and PEF were 10.6 ± 3.3, 2 ± 1, and 12.95 ± 2.80 mm, respectively. The anatomical landmarks from ALC–AEF, AEF–PEF, and PEF–OC were 27.7 ± 2.8, 10.6 ± 3.3 and 5.41 ± 1 mm, respectively.
The angles from the plane of the EF to the medial border of the OC were calculated as 13.2° and 153°, respectively. The angle from the AEF to the medial border of the OC was based on the plane between the ALC and AEF was 132° (Table 1).
For the anatomical waypoints of the EF, points of the orbit that form the transverse lines are generated on the ALC, AEF, PEF and OC. It may be mentioned that the distances between those points are orientation points for safety of EA (Fig. 4).
The navigational area of ethmoidal foramens and the recommended safety operating lateral view of the right orbit. ALC midpoint of the anterior lacrimal crest, AEF anterior ethmoidal foramen, PEF posterior ethmoidal foramen, OC optic canal. Dashed circular area localization area of ethmoidal foramens, lines passing through the landmarks
Discussion
The orbit can be affected by a large number of congenital, traumatic, neo-plastic, vascular and endocrine disorders [4, 5, 11, 18, 20, 21, 26, 27, 33, 34]. Different clinical problems such as orbital decompression, frontoethmoidal sinonasal pathology, severe epistaxis, and orbital pathology may require a surgical approach to the medial wall of the orbit [10, 18, 21, 22]. The AEF and PEF, through which the AEA and the PEA pass, are present in the medial wall (Fig. 5). Sometimes, to prevent accidental traumatization or when the artery requires to be connected, location of the EA need to be identified for intervention. For this, definition of the location of arteries’ orbital opening holes is used navigationally. Damage to these vessels can cause severe hemorrhage and may result in urgent eye surgery, in cases where orbital hematoma forms rapidly owing to the retraction of the lacerated artery into the orbit [10, 19, 27]. Etiology of the orbital hematomas can be traumatic since orbital fractures or pathological lesions such as Graves ophthalmology increase the volume of the orbital contents which results in a rise in the intraorbital pressure [28, 34].
The relationship between ethmoidal foramens and ethmoidal arteries in the medial orbital wall. The superior orbital rim, the superior orbital wall, the lateral orbital rim, and the lateral orbital wall were exposed and the medial wall becomes visible (a, c single, b, d double ethmoidal arteries; a, b supero-lateral view of medial wall, c, d supero-anterior view medial wall). a The single EF and EA pattern is presented on lateral view of medial wall. b The orbit with double EF pattern is shown on the lateral view medial wall. c The orbit sample with single EF is localized in the anterior direction of the orbit. d The orbit with double EF pattern is presented anterior direction of the orbit. ALC midpoint of the anterior lacrimal crest, AEF anterior ethmoidal foramen, PEF posterior ethmoidal foramen, EF ethmoidal foramen, OC optic canal, ON optic nerve, OA ophthalmic artery, SOV superior ophthalmic vein, SR superior rectus muscle, LPS levator palpebra superior muscle, SO superior oblique muscle, arrows ethmoidal foramens
An increase in intraorbital pressure influences vision and leads to traumatic optic neuropathy [19, 27]. Surgery of decompression of the OC through ethmoid cells is an effective way to improve and restore vision [21, 27, 28, 33]. Lateral operation of the OC should be judged by the distance between the anatomical landmarks and the orbital medial wall in a different level.
Extra-cranial ligation of the EF is performed successfully for control of the EA prior to the resection of hypervascular giant anterior skull base meningiomas, ethmoidal vessel ligation for epistaxis, explorations of the medial wall fractures and orbital decompression surgery [22]. Injuries to the EA coming through the EF during operations on the orbit make surgical interventions longer and augment the operating risk, especially for the structures of the orbit [8, 11, 14].
It is an indisputable fact that success in surgical strategy and planning mainly rely on surgeon’s knowledge of the navigational landmarks of the EF; gaining the right horizontal orientations of the medial wall, providing a shorter surgery time, and avoiding complications [4, 27, 32, 33]. The present study has quantitatively analyzed the anatomical landmarks of the EF, which have not been reported previously.
Number
Classically, there is an AEF which transmits the AEA, vein and the nerve, and a PEF, which transmits the PEA and the nerve (Fig. 5b, d) [2, 6, 15, 25]. The multiple EFs transmit EAs, similar to the AEF and the PEF [9]. The higher incidence of multiple EF is clinically important as all ethmoidal vessels need to be identified to ensure an effective control of epistaxis. The MEFs play a significant role during medial orbital wall surgery and inadvertent injuries to these arteries can result in massive orbital bleeding [9].
A variation in EF number ranging from 1 to 6 has been reported by previous researchers [1, 2, 6, 9, 25]. Abed et al. [2] and Piagkou and co-authors [25] reported the cases of quintuple EF. Similarly, in this study, quintuple EF was identified in 1.1 % specimens (Fig. 3c). Multiple EF is previously reported as unilateral with a range of 25–62 % [16, 17, 20, 25, 31]. In our study, this incidence was 25.5 %. The accessory hole can be observed in approximately one of four orbits. The existence of quadruple EF proves the presence of holes which are located on the medial wall with frequent intervals. This is a misfortune in terms of surgical intervention. It becomes risky to make an intervention on the medial wall as the safe intervention region has become narrow and there are quite a number of arteries to be connected (Figs. 3c, d, 4).
Distance
The distances between the anatomical points on the medial wall provide essential orientation information for surgeons to prevent injury of the important neurovascular bundles. The location of the AEF is important since it is a reliable anatomical landmark for identifying the AEA (Figs. 4, 5) [17, 23, 25, 27, 32, 34]. The ALC was used as a constant landmark on the medial wall in the present study and previous studies since it can be easily located by palpation (Figs. 4, 5) [17]. The anterior lacrimal crest is an important landmark during orbital and oculoplastic surgery, external dacryocystorhinostomy, as the anterior limb of the medial canthal tendon attaches to the anterior lacrimal crest superiorly [11, 27, 34]. Incision is made along the anterior lacrimal crest to enter the orbit. Remembering the mean distance of ALC–AEF during skin, subcutaneous, medial canthal ligament and lacrimal gland apparatus dissections, allows the surgeon to have a safe entry to the anterior ethmoidal neurovascular bundle (Figs. 4, 5).
Another important waypoint is the distance from the PEF to the OC. In literature the mean OC–PEF distance ranges 4.3–9.15 mm [5, 17, 24].
Safe distance of the ALC–EF was measured as 22.1 mm on medial wall with spatial software technology in this study (Fig. 4). The line of the location of the EF was calculated 16.2 mm in present study. To damage accidental traumatization of the EA may result in orbital surgery on this line the medial wall (Fig. 4). The mean OC–EF distance measured in this study was 2.4 mm, which will be of help to surgeons to avoid optic nerve injury (Fig. 4).
Orientational waypoints are valuable value for surgeons on the delicate medial orbital wall. Traditionally, surgeons have used the 24–12–6 mm rule for ALC–AEF, AEF–PEF, and PEF–OC to navigate the medial wall structures [1, 14]. The waypoints have been reported with ratios of 26–14–12 [2], 25–11–6 [9], 24–10–7 [17] and 23–10–4 [24]. The anatomical landmarks from ALC–AEF, AEF–PEF, and PEF–OC was 27.7 ± 2.8, 10.6 ± 3.3, 5.4 ± 1 mm in this study.
Angle
Angles on the orbital medial wall are equally important as the distances between the points. It was stated in the study by Abed et al. [1, 2] that the angles from the plane of the EF to the OC are calculated to be 32° and 112°, respectively. The angle from the AEF to the OC based on the plane between the ALC and AEF is 107°. In this study, the angles from the plane of the EF to the medial border of the OC were calculated to be 13.21° and 153°, respectively [2]. The angle from the AEF to the medial border of the OC based on the plane between the ALC and AEF was 132° in this study. Potential location of EFs and passing EAs through the canal were demonstrated in Fig. 5. Variation positions EF must remembered and utmost care must be paid while approaching the area of the artery. Even though there is a double arterial pattern in the orbit (Fig. 3b), it must be remembered that there may be more number EF patterns in the orbital wall (Fig. 3c, d). These arteries which carry a potential risk of bleeding are important as they may contain hidden traps for surgeons (Fig. 3b).
When compared with the studies of previous researchers, it is thought that there may be a difference resulting from ethnic origin or measurement method. The measurements are considered valuable since the method used was a more standard one.
In this study, digital photometric methods were used to collect linear, area and perimeter data of medial orbital wall. The process of measuring photographs (photogrammetry) has been routinely in odontological studies for several decades, and is being employed in bioarchaeological and forensic investigations concerning other anatomical structures as well. Photogrammetry has several advantages over conventional measurements methods [8, 12, 24]. Another advantage of it is the opportunity to preserve the material, which allows to repeat the measurements anytime, and to add new parameters in subsequent measurements [8, 12, 24]. After getting the digital images, they can be edited in image processing programs like Photoshop to obtain any standard parameter desired. The measurements may be performed by using digital image processing and analysis softwares like Image J, which is one of the most preferred processing and analysis, provided by National Institute of Health, available at http://rsb.info.nih.gov.ij. The most important point in measurements is to set a proper and visible scale for each size, the scale can be set using this bar. Success of photogrammetry depends on uniform lighting conditions, placement of feature positions close to their actual positions in images, and providing accurate scales on the images [12].
Increased pressure in the optic nerve due to an external (depressed bone fracture, orbital tumors, or hematoma) or internal (optic nerve edema in traumatic optic neuropathy, inflammatory diseases or increased intracranial pressure) mechanism causes optic nerve dysfunction and results in ischemia with irreversible vision loss if left untreated.
In our study, the measurements of these distances and a description of the projection point may serve as crucial clinical applications for localizing the EA, defining the severity of arterial injury and detecting possible complications in preoperative planning and postoperative evaluation. The development of spatial processing technology provided a basis for obtaining valuable measuring points in navigational approach (Fig. 4).
With the development of spatial software technology, anatomical waypoints can be measured effectively. Application of the three-dimensional technique overcomes the limitations of two-dimensional scans, making it possible to observe the orbital wall bones from various angles and calculate the lengths of some parameters with certain software [8, 24].
Conclusions
An analysis of the variability of the AEF and PEF morphology and the distances between its orbital opening and selected topographical points which can be of significance for clinical applications were investigated in this study.
References
Abed SF, Shams P, Shen S, Adds PJ, Uddin JM (2011) A cadaveric study of the morphometric and geometric relationships of the orbital apex. Orbit 30(2):72–76
Abed SF, Shams P, Shen S, Adds PJ, Uddin JM (2012) A cadaveric study of ethmoidal foramina variation and its surgical significance in Caucasians. Br J Ophthalmol 96(1):118–121
Abuzayed B, Tanriover N, Gazioglu N, Eraslan BS, Akar Z (2009) Endoscopic endonasal approach to the orbital apex and medial orbital wall: anatomic study and clinical applications. J Craniofac Surg 20(5):1594–1600
Asanau A, Timoshenko AP, Vercherin P, Martin C, Prades JM (2009) Sphenopalatine and anterior ethmoidal artery ligation for severe epistaxis. Ann Otol Rhinol Laryngol 118(9):639–644
Avcı E, Aktüre E, Seçkin H, Uluç K, Bauer AM, Izci Y, Morcos JJ, Baskaya MK (2011) Level I to III craniofacial approaches based on Barrow classification for treatment of skull base meningiomas: surgical technique, microsurgical anatomy, and case illustrations. Neurosurg Focus 30(5):E5
Caliot P, Plessis JL, Midy D, Poirier M, Ha JC (1995) The intraorbital arrangement of the anterior and posterior ethmoidal foramina. Surg Radiol Anat 17(1):29–33
Cankal F, Apaydin N, Acar HI, Elhan A, Tekdemir I, Yurdakul M, Kaya M, Esmer AF (2004) Evaluation of the anterior and posterior ethmoidal canal by computed tomography. Clin Radiol 59(11):1034–1040
Celik S, Kazak Z, Ozer MA, Govsa F (2014) Navigational area of the cranio-orbital foramen and its significance in orbital surgery. Surg Radiol Anat. doi:10.1007/s00276-014-1293-7
Cheng AC, Lucas PW, Yuen HK, Lam DS, So KF (2008) Surgical anatomy of the Chinese orbit. Ophthal Plast Reconstr Surg 24(2):136–141
Dallan I, Tschabitscher M, Castelnuovo P, Bignami M, Muscatello L, Lenzi R, Battaglia P, Sellari-Franceschini S (2009) Management of severely bleeding ethmoidal arteries. J Craniofac Surg 20(2):450–454
Deda H, Ugur HS, Yorulmaz I, Babur K (2001) Anteromedial approach to the orbit. Skull Base 11:233–239
Douglas TS (2004) Image processing for craniofacial landmark identification and measurement: a review of photogrammetry and cephalometry. Comput Med Imaging Graph 28:401–409
Floreani SR, Nair SB, Switajewski MC, Wormald PJ (2006) Endoscopic anterior ethmoidal artery ligation: a cadaver study. Laryngoscope 116(7):1263–1267
Graham SM, Brown CL, Carter KD, Song A, Nerad JA (2003) Medial and lateral orbital wall surgery for balanced decompression in thyroid eye disease. Laryngoscope 113(7):1206–1209
Han JK, Becker SS, Bomeli SR, Gross CW (2008) Endoscopic localization of the anterior and posterior ethmoid arteries. Ann Otol Rhinol Laryngol 117(12):931–935
Huanmanop T, Agthong S, Chentanez V (2007) Surgical anatomy of fissures and foramina in the orbits of Thai adults. J Med Assoc Thai 90(11):2383–2391
Karakas P, Bozkir MG, Oguz O (2003) Morphometric measurements from various reference points in the orbit of male Caucasians. Surg Radiol Anat 24(6):358–362
Kelly CP, Cohen AJ, Yavuzer R, Jackson IT (2005) Cranial bone grafting for orbital reconstruction: is it still the best? J Craniofac Surg 16(1):181–185
Kountakis SE, Maillard AA, El-Harazi SM et al (2000) Endoscopic optic nerve decompression for traumatic blindness. Otolaryngol Head Neck Surg 123:34–37
Lannoy-Penisson L, Schultz P, Riehm S, Atallah I, Veillon F, Debry C (2007) The anterior ethmoidal artery: radio-anatomical comparison and its application in endonasal surgery. Acta Otolaryngol 127(6):618–622
Liao SL, Chang TC, Lin LL (2006) Transcaruncular orbital decompression: an alternative procedure for Graves ophthalmopathy with compressive optic neuropathy. Am J Ophthalmol 141:810–818
Manjila S, Cox EM, Smith GA, Corriveau M, Chhabra N, Johnson F, Geertman RT (2013) Extracranial ligation of ethmoidal arteries before resection of giant olfactory groove or planum sphenoidale meningiomas: 3 illustrative cases with a review of the literature on surgical techniques. Neurosurg Focus 35(6):E13
McDonald SE, Robinson PJ, Nunez DA (2008) Radiological anatomy of the anterior ethmoidal artery for functional endoscopic sinus surgery. J Laryngol Otol 122(3):264–267
Ozer MA, Celik S, Govsa F (2009) A morphometric study of the inferior orbital fissure using three-dimensional anatomical landmarks: application to orbital surgery. Clin Anat 22(6):649–654
Piagkou M, Skotsimara G, Dalaka A, Kanioura E, Korentzelou V, Skotsimara A, Piagkos G, Johnson EO (2014) Bony landmarks of the medial orbital wall: an anatomical study of ethmoidal foramina. Clin Anat 27:570–577
Simmen D, Raghavan U, Briner HR, Manestar M, Schuknecht B, Groscurth P, Jones NS (2006) The surgeon’s view of the anterior ethmoid artery. Clin Otolaryngol 31(3):187–191
Song Y, Song J, Liu Q, Li Y, Yao D (2014) Study on measurements for margin of safety in lateral operation of a transnasoethmoid-sphenoid approach to decompress the optic canal. J Craniofac Surg 25(1):243–246
Takahashi Y, Miyazaki H, Ichinose A, Nakano T, Asamoto K, Kakizaki H (2013) Anatomy of deep lateral and medial orbital walls: implications in orbital decompression surgery. Orbit 32(6):409–412
Unal M, Leri F, Konuk O, Hasanreisoglu B (2003) Balanced orbital decompression combined with fat removal in Graves ophthalmopathy: do we really need to remove the third wall? Ophthal Plast Reconstr Surg 19(2):112–118
Takahashi Y, Kakizaki H, Nakano T (2011) Accessory ethmoidal foramina: an anatomical study. Ophthal Plast Reconstr Surg 27(2):125–127
Wang L, Youseef A, AlQahtani AA, Gun R, Prevedello DM, Otto BA, Ditzel L, Carrau L (2014) Endoscopic anatomy of the middle ethmoidal artery. Int Forum Allergy Rhinol 4(2):164–168
Yang YX, Lu QK, Liao JC, Dang RS (2009) Morphological characteristics of the anterior ethmoidal artery in ethmoid roof and endoscopic localization. Skull Base 19(5):311–317
Yeh S, Yen MT, Foroozan R (2004) Orbital apex syndrome after ethmoidal artery ligation for recurrent epistaxis. Ophthal Plast Reconstr Surg 20(5):392–394
White DV, Sincoff EH, Abdulrauf SI (2005) Anterior ethmoidal artery: microsurgical anatomy and technical considerations. Neurosurgery 56(2):406–410 (discussion 406–410)
Conflict of interest
The authors declare that they have no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Celik, S., Ozer, M.A., Kazak, Z. et al. Computer-assisted analysis of anatomical relationships of the ethmoidal foramina and optic canal along the medial orbital wall. Eur Arch Otorhinolaryngol 272, 3483–3490 (2015). https://doi.org/10.1007/s00405-014-3378-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3378-7