Abstract
Compare the number of implants performed in the last 12 years for children and adolescents up to 18 years in different regions of mainland Portugal. Study the trend of total implants over the years as well as the percentage held in early ages. Verify to what extent this practice is in line with the values of fairness and justice that underpin European health systems. A retrospective study of cochlear implantation was conducted using a hospital database containing all the episodes with cochlear implant procedures in public hospitals that occurred in Portugal between 2000 and 2012. An analysis by age, year, and region of the implants were performed. The Northern and Central regions, the nearest big center specializing in cochlear implants in Portugal, are those with the largest number of implants: 2.0 and 2.4 per 10,000 children, respectively. The regions of Alentejo and Algarve, which are more rural and remote regions of the center, record the smallest number of implants, 1.1 and 1.5 per 10,000 children, respectively. Over the years, there seems to be an increase of implants implemented in children under 18, most notably from a significant reduction in 2011 and 2012. However, an increase in children implanted before 24 months has been observed from the same zero children at this age in the early years studied to 0.46 per 10,000 inhabitants in 2012. The right to adequate health care must be in accordance with the full respect of fundamental human rights. Economic, social, and educational conditions must also be guaranteed in this process of auditory rehabilitation. Societies must develop a system of ethical health priorities, so that even in situations of financial crisis, the most disadvantaged sectors are not the most penalized ones by the inevitable economic constraints that are implemented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Childhood deafness represents an important social and public health problem. Indeed, epidemiological studies conducted throughout the western world have proven that there is a child with profound deafness for every 1,000 births [1, 2]. Hearing loss in this age can have various causes, such as prematurity, intrauterine infections, and hereditary or genetic factors. It should be noted that, contrary to what occurs in other areas of medicine, the incidence of neonatal hearing loss has not diminished in the last few decades, as major causal factors are random (genetic causes) or tend to increase with the evolution of medicine (prematurity). Even more, to be effective, a screening program of a deaf child should be made in the first weeks of life. The Joint Committee on Infant Hearing recommended universal newborn hearing screening prior to hospital discharge for all infants [3]. The goal of early hearing detection and intervention is to maximize linguistic competence for deaf or hard of hearing children. Measures of rehabilitation show superiority when intervention is initiated early. Without adequate intervention to learn a language, these children will fall behind their hearing peers in communication, cognition, reading, and social-emotional development.
Some studies find advantages to neonatal deafness universal screening, such as a faster progression to the rehabilitation process [4, 5]. This was the case in a study that used children born in Colorado, in hospitals where universal screening of neonatal deafness was conducted. These hospitals were compared with those that did not perform the screening, and it was found that children with deafness in the screening group were 80 % more likely to have language development within the normal range than children with deafness born in hospitals without screening. Similarly, the vocabulary and the ability to speak were significantly different; that is, children who were subjected to neonatal screening had a wider vocabulary [4].
In 2011, in mainland Portugal there were 6,087 persons with hearing disabilities between 0 and 19 years old [6]; therefore, there were about 30 persons with hearing impairments per 10,000 inhabitants aged between 0 and 19 years old. The incidence of bilateral hearing loss in unborn children is estimated to be one per one thousand births, and 50 percent of these cases are hereditary [7]. From the medical point of view deafness is always a disease and should be treated as such. One of the most developed treatment methods to overcome profound deafness in childhood is the technology of cochlear implantation. The cochlear implant is the most important progress in the treatment of prelingually deaf children, especially if it is performed during their early years [8, 9]. Over the past several decades, implant technology has dramatically developed and has resulted in significant advances in speech and language development in this population. For some children, this surgical technique offers a relatively new and promising way to improve or even acquire a more effective communication. For decades scientists have worked on different models of cochlear implants—an electronic device designed to compensate for missing hair cells or disturbances in the inner ear. Inner ear disturbances targeted by cochlear implants are severe to profound. This is an effective method but implies the existence of technological resources and materials for its application. It should be stated that more moderate levels of inner ear disturbances are usually not rehabilitated with cochlear implantation. Each level brings different challenges and the need for different treatment and technology options.
The Food and Drug Administration (FDA) approved cochlear implantation in adults in 1984 and in children in 1986. The multi-channel cochlear implant was approved by FDA in children with two years of age and commercialized in the United States in 1990. At present guidelines for the cochlear device recommend cochlear implantation in persons aged 2 years and older with severe deafness (70–90 db), and in children 12–23 months of age with profound deafness (90 +db) [10, 11].
Presently, in some countries the implementation is performed even before this age, since early implantation offers greater potential regarding minimizing the effects of auditory deprivation, and since electrical stimulation promoted by the device gives access to information that is necessary to stimulate the auditory system during the critical period for the acquisition of speech and language [12]. Recent studies have shown that the placement of cochlear implant before one year of age, compared to implantation in children after this age, allows them to develop more effectively the perceptible level of hearing in its whole; namely, it appears to provide considerable benefits in terms of receptive and expressive language [13, 14]. A number of investigators have demonstrated significant improvements in speech production following cochlear implantation. For example Tye-Murray et al. assessed whether children acquired intelligible speech following prolonged cochlear implant experience and examined their speech error patterns, examined how age at implantation influences speech acquisition, and assessed how speech production and speech perception skills relate. The authors demonstrated that children who receive a cochlear implant before the age of 5 years appear to show greater benefit in their speech production skills than children who are older, at least after a minimum of 2 years of use [15]. Because it is still a controversial issue more scientific evidence is needed to corroborate the findings that long-term outcomes are better if implantation is performed before 12 months of age.
However, the economic and financial crisis that has developed in the last few years worldwide, with a particular incidence in Europe, profoundly affected Portugal in 2011. The country was forced to implement a harsh program of adjustment of its public finances, which had a profound and lasting impact on the social functions of the State, but also in the business economy and the daily lives of citizens.
The aim of this study is to assess the developmental trend over the last few years of the total of cochlear implants performed in children and adolescents in the different regions of mainland Portugal. A secondary objective is to determine the percentage of cochlear implants performed in early ages and to verify to what extent this practice is in line with the values of fairness and justice that underpin European health systems.
Methods
Study design
A retrospective study of cochlear implantation was conducted using a hospital database containing all the episodes with cochlear implant procedures in public hospitals which occurred in Portugal between 2000 and 2012.
Setting
The data used in this analysis was provided by the Central Administration of the Health System (ACSS) and includes hospital episodes with cochlear implant procedures (codes ICD-9-CM 20.96-98) with hospital discharge between the years 2000 and 2012 in Portuguese public hospitals.
The residence of the patients was grouped into five statistical regions, considering the Portuguese Territorial Units for Statistics, level II (NUTS II), namely “North”, “Center”, “Lisbon”, “Alentejo” and “Algarve” (Mainland Portugal), according to Regulation (CE) No 1059/2003 of the European Parliament and of the Council of 26 May 2003 [16]. In the analysis performed, the episodes relating to patients with addresses outside mainland Portugal were excluded (19 patients aged up to 18 years old). Also, the episodes with patients with 18 or more years of age were excluded from this analysis. The age, in months, was calculated considering the date of admission and date of birth of the patient. Population data was obtained from the National Institute of Statistics website (www.ine.pt), in particular through the indicator “Resident population (Long series, start 1991-No.) by Place of residence (NUTS-2002), Sex and Age; Annual”.
Participants
The sample is composed of all deaf children and adolescents (under 18 years old) who were implanted in Portuguese public hospitals between 2000 and 2012.
Statistical analysis
A descriptive analysis was performed for cochlear implant hospitalizations by age, year, and region of implant. To compare the proportion of children aged less than 24 months, between 24 and 36 months and over 36 months in different years, we used the Fisher’s exact test for a significance level of 0.05.
Ethical considerations
According to Portuguese policy, the study required review by an ethics committee that gave its formal approval. All the procedures followed where in accordance with the Helsinki Declaration of the World Medical Association.
Results
Between 2000 and 2012, 371 deaf children and adolescents were implanted in public hospitals in Portugal. Regardless of the area of residence, the vast majority of implants were performed in the central zone where the major hospital that specializes in this type of implantation is located (Table 1).
The North and Center regions, which are closer to the big specialized center for cochlear implants in Portugal, exhibited the largest number of implants per 10,000 children. The regions of Alentejo and Algarve, which are more rural and distant from the center, exhibited the lowest number of implants per 10,000 children (see Table 2; Fig. 1).
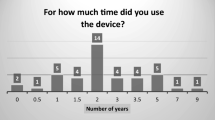
Over the years, the number of implanted children before 24 months has increased, especially from 2007 to 2010. Although in 2011, there has been a decrease of 0.64–0.16 implanted per 10,000 inhabitants (Table 3).
There are significant differences between the year in which the implant was performed and the proportion of children under 24 months, between 24 and 36 months and over 36 months (P < 0.001). There was an increase over the years in the percentage of implanted children before 24 months of age (Fig. 2).
Discussion
Cochlear implants have provided, over recent times, increasingly effective results and have surpassed the expectations of most professionals and those who doubted its effectiveness, namely in prelingual deaf children. Many factors, such as progress and development of hardware (implant design) and software (new strategies for encoding and stimulation modes), refined surgical techniques, greater experience in programming, and rehabilitation and, inevitably, early diagnosis, have contributed to providing better and proven results [17].
There are multiple factors to consider before definitively proceeding with the implantation. Most authors state that the study of the preoperative level of hearing and evaluation of psychosocial conditions, which enables the continued use of this aid, are essential factors for the success of an implantation program [18, 19]. A fundamental component of the candidacy determination is an accurate assessment of baseline status that begins by characterizing residual, functional hearing, and response to amplification. To date, the most consistent finding is that patients with greater degrees of residual hearing preoperatively perform at higher levels with cochlear implants. In children, this situation seems even more complex because of greater difficulty and reduced reliability of audiologic testing in very young children. However, some studies have accumulated support about the superiority of patients’ implantation of increasingly younger ages and in patients with higher degrees of residual hearing [20, 21].”
Thus, patients are selected for the introduction of the cochlear implant based on clinical, audiological, psychological, and social criteria. The factors of success of an auditory rehabilitation program are associated not only to the intrinsic and to their cognitive potential or the number of residual cells at the level of the hearing system, but mainly to the social, educational, and familial underlying conditions. The placement of a cochlear implant is only the first step of the entire hearing rehabilitation program, so its malfunction can be disastrous on a personal and familial level.
As such, the family and the child in the process of informed consent should be informed about the whole global process of rehabilitation, since this global rehabilitation is associated with a large personal, family, and material effort. During the process of informed consent, the complications that may arise from the implantation should be explicit [7]. Not only the technical complications inherent to surgery, but also the complications associated with the global failure of the adaptation and rehabilitation program of the child to the cochlear implant, should be clearly communicated to the legal representatives [22]. Thus, the consent process should be in accordance with the formal principle of respect for personal autonomy, and also in accordance with the substantive principle of non-maleficence.
There are multiple studies and reports at the international level that emphasize the importance of universal neonatal hearing screening. In May 1998, the European Consensus Development Conference on Neonatal Hearing Screening advised the universal neonatal hearing screening in all unborn. This screening should include a diagnosis as well as the respective intervention. It is expected that these screening programs identify approximately 80 % of the cases and can effectively present around 2–3 % false positives in well-conducted programs. That declaration also states that the universal neonatal hearing screening is more efficient, and that the cost is considerably lower when compared with the screening performed at 7 and 9 months of age, by the behavioral assessment [23]. In Portugal, there is not an effective program of universal neonatal hearing screening in all hospitals, which may lead to a late early intervention in respect to other European countries. Prior to the universal neonatal hearing screening in some North American states, the average age of diagnosis of profound bilateral hearing loss was close to 3 years of age [24]. Today, it is widely accepted that simple medical observation and suspicion of the parents are not sufficient for its identification in the first year of life. This has, as consequence, a late diagnosis and intervention for the affected individuals.
Indeed, universal newborn hearing screening has led to increased identification of infants with hearing loss worldwide. This increase in early diagnosis has led to greater opportunities for early intervention. There is now abundant evidence that early implantation in children is advantageous. From a medical perspective, deafness is always the result of an alteration of the auditory system with well-characterized histological and cytological changes. As mentioned previously, congenital deafness occurs in about 1/1,000 births and 50 % of cases are hereditary. There are at least 30 genes responsible for non-syndromic recessive deafness, that is, for deafness that is not associated with other clinical signs or symptoms. In summary, profound deafness in childhood is regarded by medical science as a disease and should be treated accordingly.
In this context, and given the disability and resulting incapacity, there is no doubt that the universal neonatal hearing screening should be considered a priority in health policy in any civilized country. It should be noted that the universal neonatal hearing screening with otoacoustic emissions is already common practice in many countries. This is a simple method that has no risk to the child and that does not need the child’s active collaboration. When performed in the first days after birth (preferably before leaving the maternity hospital), the method is associated with a low rate of false positives and false negatives, being in full compliance with the rules of evidence-based medicine.
International recommendations in this field suggest that a widespread program of universal neonatal hearing screening should be implemented in all countries, given the low cost of otoacoustic emissions and its high sensitivity and specificity [25, 26]. It is important that the early hearing detection and intervention programme is linked to existing health care, social, and educational systems [27]. Moreover, a full equity in access to health means that there are mechanisms to effectively refer these patients to the public health system and to the education system. Remember that the goal of a screening program is to detect, not only but mostly, positive cases and to integrate and rehabilitate the family and a disabled child.
Given the scarcity of available resources, the application of the principle of justice to health care implies that there should be a fair definition of priorities in their provision [28]. We believe that the supported cost by completion of screening and cochlear implantation will certainly be less than the costs of the treatments that will have to be made in the event of late-detected deafness and if the rehabilitation does not happen within the appropriate time. In the United States, the cost of lifetime treatment for a child with congenital deafness has been estimated at around $1 million USD. This cost is due to the need for special education, social services, and support as well as the decrease in productivity of deaf adults [29].
Both the costs of a universal neonatal hearing screening and the costs of cochlear implantation are undeniable and must necessarily be evaluated in economic terms. Therefore, a thorough cost-benefit analysis should be made, implying that the overall costs arising from the investment in the implementation of universal screening and subsequent rehabilitation should be compared against the global social and educational costs of a deaf child throughout his or her life span.
Indeed, the true value of early identification and rehabilitation for the individual and for society will be clearly elucidated in the future as we learn more about the benefits of early identification and rehabilitation and how it relates to educational achievement, with social integration and employment the lifetime of the individual.
The results of this study reveal that Portugal holds few cochlear implants compared to the estimated needs of the population when compared, for example, with Italy (Portugal—0.62 CI/100,000 inhabitants in 2011, Italy—1.2 CI/100,000 inhabitants in 2011). This may be due to several factors: Firstly, the fact that Portugal has not yet defined the universal neonatal hearing screening as a priority in health which leads to a delayed early detection and, therefore, less eligible candidates, for effective implantation. In fact, the number of implants has not increased much before the age of 18. However, it appears that patients who were implanted did it at an increasingly early age, which meets the main existing guidelines on this matter.
Moreover, the data of this investigation confirm the huge geographical inequity that exists in Portugal in terms of auditory rehabilitation. Indeed the factor “proximity of residence to the center of reference” is crucial for access to this technology. In Tables 1 and 2, we can verify the importance of geographical location in accessing cochlear implantation. That is, it is important to understand the particular reasons from within the perspective of integration of health care that cause this situation and to identify the solutions that are needed to overcome this problem, which undermines the principle of equity in access to health care. Indeed, the Portuguese health system is a decentralized system; this is immediately evident because there are specialized centers for cochlear implants in the three major regions of the country (Lisbon, Coimbra, and Oporto) but only one (Coimbra) performs cochlear implantation at a regular basis. Given the specificity and epidemiology of cochlear implantation, it would be worth creating a centralized national system to guarantee all citizens equal access to this technology, regardless of the national region where the patient lives.
In a truly just society anyone, particularly a child, should have the right to an open future. That is, the parents (or legal guardians) must do everything in their power so that the deaf child may fully exercise their autonomy in the future. This new class of fundamental rights requires a high ethical commitment from parents, and when they are not able to provide the child with the conditions for full development of their personality by themselves it is the responsibility of society to do it.
The universal neonatal hearing screening should then be generalized since this is a simple and effective method that is in principle devoid of unwanted side effects and exhibits a sufficiently low unitary cost to be included in perinatal care. In the process of obtaining informed, free, and clear consent, parents should be informed of the scope and scale of this screening program and especially the benefits of early detection of profound deafness. It is in this sense that the principle of equal opportunities holds that to treat all people equally and to provide genuine equal opportunities, society must pay more attention to those who are born with less means and in disadvantaged social positions.
Making people with hearing loss part of the community is only a first step, because being part of the community means collaborating in its structure and playing a social role. Thus, the real challenge to reach is that people with special educational needs in general, and the deaf children in particular, perform social functions that are valid and valued.
It is in this clinical and social context that we should assess the evolution of auditory rehabilitation in Portugal against the economic crisis and financial adjustment program (2011–2014). Indeed, Portugal has a reference center where cochlear implants have been performed since 1985. It is located in the center of Portugal (Coimbra), although cochlear implants are also performed in the North (Oporto) and in the South (Lisbon). In the administrative areas of Algarve and Alentejo, there are no public hospitals where cochlear implants are performed. In Portugal, there are no studies that indicate the number of implants performed.
Most contemporary ethical theories claim for the existence of fundamental human rights, independent of any type of physical constitution, genotype, and consequently any physical characteristic of the human species. Well, if a human is much more than a physical constitution, we cannot enhance the genetic determinism at the expense of educational aspects and environmental acculturation, because this would be a reductive vision of the human person and, more than that, would be in contradiction with the Universal Declaration of Human Rights which emphasizes the principle that all people are born free and equal in dignity and rights [30].
There is no doubt today that the only major difference between deaf people and people who listen lies in the organ of hearing. No difference was found between deaf and hearing people with regard to their cognitive abilities [31]. However, deaf people may not develop processes that will enable a good communication with earing people and this is the main reason why the deaf have developed their own means of communication adapted to their characteristics, which allow them to reduce or even overcome the limitations inherent with the lack of hearing. Sign language, like spoken language, consists of a small set of elements that, in a figurative way, could correspond to the vowels and consonants arranged according to certain rules: hand gestures, its location in proximity to the body, its orientation and their movements. Today, it is recognized as a language equivalent to any other [32]. Whichever method of communication chosen by the parents it is essential to guarantee the child’s right to an open future.
Families who opt for the Deaf cultural model have a long journey ahead as a whole change in family dynamics is needed, namely at the level of communication, since the use of signs by parents and siblings of deaf children, the earliest possible, can facilitate family communication and promote integration of the deaf child. This choice also imposes costs for family and society throughout all the life of the subject. Like all children, the deaf child has a right to education guaranteeing, therefore, a true equality of opportunity to academic achievement. For the fulfillment of this right, it is fundamental to attend to the special needs of each child to provide the best biopsychosocial development possible. Then the school must provide the deaf child the opportunity to access to sign language interpreters, speech therapists, psychologists, among others. Nevertheless, form a strict economic perspective, evidence-based studies are needed that compare the overall costs arising from the choice of the clinical-therapeutical model or by cultural model. Therefore, a thorough cost-benefit analysis should be made, implying that the overall costs arising from the investment in the implementation of universal screening and subsequent rehabilitation should be compared against the global social and educational costs of a deaf child throughout his/her life span.
Indeed, the true value of early identification and rehabilitation for the individual and for society will be clearly elucidated in the future as we learn more about the benefits of early identification and rehabilitation and how it relates to educational achievement; and also with social integration and employment along the lifetime of the individual.
The right to diversity and specifically to cultural diversity should be in accordance with the overall respect for fundamental human rights. Human beings, their dignity and their fundamental rights should be respected as something supreme. Thus, taking into account the different levels of disability, society should provide the necessary resources so that the right to an open future is fulfilled, that is, that the interpersonal differences may be eliminated or at least reduced. In 1980, Joel Feinberg suggested the existence of “rights-in-trust”, rights which are related to the defense of individual interests by legitimate legal representatives when the individual, depending on their level of cognitive development, cannot exercise them in fact. Therefore, these rights must be protected in the present to be exercised later in life. This kind of right can and should be applied to the deaf child [33].
It is in this context that over the last three decades hearing rehabilitation programs have been introduced for profound deaf children in all developed countries, and Portugal was no exception. However, the effect of the economic and financial crisis has been particularly severe toward the access to these programs. In fact, if it is true that cochlear implantation has increased dramatically between 2006 and 2010 as a result of a substantial public investment in this technology, it is also true that the number of implants decreased in 2011 and 2012. It might be interesting to study if in the periods of economic crisis, there is some positive correlation between the decrease in the number of implants and the number of families who choose the cultural model based on sign language.
The years 2011 and 2012, the last for which there are reliable statistics in Portugal, show that there was a significant decrease in the placement of implants in all age groups (before 24 months, before 36 months, and before the age of 18; Table 3).
Indeed, the effect of austerity policies was dramatic in many health care systems, namely in countries with tax-financed systems. This was the case in Portugal and in other European countries. In Spain for instance, the solution to the crisis was health care cuts and an increase in cost sharing for services [34]; in Italy Giulio de Belvisa et al. [35] claim that in a period of public funding constraints health authorities should monitor access to care of the most vulnerable groups and specifically target interventions to those who may be disproportionally hit by the crisis. Also, it has been suggested that the health care sector is not protected during periods of austerity and that much of the burden of budget cuts is concentrated in the health care sector, particularly in countries exposed to International Monetary Fund lending agreements [36].
From a strictly economic perspective what is at stake is a comprehensive cost-benefit analysis. This analysis should take into account the direct and indirect economic costs between whether or not cochlear implantation is performed in children who need it. It should also consider the costs of investing in the realization of a universal neonatal hearing screening as well as subsequent cochlear implantation with its resulting benefits. Finally, it should involve an analysis of the overall burden of society by not carrying out those implants.
In summary, while it is true that society has a duty to promote the conditions for which the child has the right to an open future [30], in a financial crisis certain social benefits such as access to an appropriate hearing rehabilitation program are seriously compromised. The deaf child needs hearing rehabilitation to achieve individual freedom. If the family opts for the placement of a cochlear implant, this should be considered as being in the best interest of the child. The right to adequate health care must be in accordance with the full respect of fundamental human rights. Economic, social, and educational conditions must also be guaranteed in this process of auditory rehabilitation. Also, societies must develop a system of ethical priorities in health care so that even in situations of financial crisis, the most disadvantaged sectors are not the most penalized ones by the inevitable economic constraints that are implemented.
References
Early identification of hearing impairment in infants and young children: NIH Consensus Development Conference 1–3 March 1993 (1993). Int J Pediatr Otorhinolaryngol 27(2): 201–202
Burton S, Blanton S, Culpepper B, White K, Pandya A, Nance W, Arnos K (2006) Education in the genetics of hearing loss: a survey of early hearing detection and intervention programs. Genetics Med 8(8):510–517
AmericanAcademyof Pediatrics Joint Committee on Infant Hearing (1995) Joint committee on infant hearing 1994 position statement. Pediatrics 95(1):152–156
Yoshinaga-Itano C (2003) Early intervention after universal neonatal hearing screening: impact on outcomes. Ment Retard Dev Disabil Res Rev 9:252–266
Yoshinaga-Itano C, Sedey AL, Coulter DK, Mehl AL (1998) Language of early- and later-identified children with hearing loss. Pediatrics 102:1161–1171
Statistics Portugal. Census 2011. Available from: http://www.ine.pt. Cited 19 June 2014
Nunes R (2001) Ethical dimension of paediatric cochlear implantation. Theor Med Bioeth 22:337–349
Peixoto MC, Spratley J, Oliveria G, Martins J, Bastos J, Ribeiro C (2013) Effectiveness of cochlear implants in children: long term results. Int J Pediatr Otorhinolaryngol 77:462–468
May-Mederake B (2012) Early intervention and assessment of speech and language development in young children with cochlear implants. Int J Pediatr Otorhinolaryngol 76:939–946
Bradham TS, Snell G, Haynes D (2009) Current practices in pediatric cochlear implantation. Perpect Hear Hear Disord Child 19:32–42
Clark JG (1981) Uses and abuses of hearing loss classification. Asha 23:493–500
Kileny PR, Zwolan TA, Ashbaugh C (2001) The influence of age at implantation on performance with a cochlear implant in children. Otol Neurotol 22(1):42–46
Leigh J, Dettman S, Dowell R, Briggs R (2013) Communication development in children who receive a cochlear implant by 12 months of age. Otol Neurotol 34(3):443–450
Valencia DM, Rimell FL, Friedman BJ, Oblander MR, Helmbrecht J (2008) Cochlear implantation in infants less than 12 months of age. Int J Pediatr Otorhinolaryngol 72:767–773
Tye-Murray N, Spencer L, Woodworth G (1995) Acquisition of speech by children who have prolonged cochlear implant experience. J Speech Hear Res 38(2):327–337
Official Journal of the European Union (2003). Publishing PhysicsWeb http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2003:154:0001:0041:PT:PDF. Accessed 14 July 2014
Duarte I, Santos C, Rego G, Nunes R (2014) Health-related quality of life in children and adolescents with cochlear implants: self and proxy reports. Acta Oto-Laryngologica. doi:10.3109/00016489.2014.930968
Niparko JK, Lingua C, Carpenter RM (2009) Assessment of candidacy for cohlear implantation. In: Niparko John (ed) Cochlear implants principles & pratices, vol 2nd edn. Lippincott Williams & Wilkins, USA
Schwartz S (1996) Choices in deafness. Woodbine House, United States
Sampaio AL, Araujo MF, Oliveira CA (2011) New criteria of indication and selection of patients of cochlear implant. Int J Otolaryngol 2011(573968):13. doi:10.1155/2011/573968 [Epub 2011 Oct 13]
Zwolan T, Tomas E (2009) Contemporary protocols for evaluating cochlear implant candidacy of children in. Perspect Hearing Hearing Disord Children 19(1):4–13
Hyde M, Power D (2006) Some ethical dimensions of cochlear implantantion for deaf children and their families. J Deaf Stud Deaf Edu 11(1):102–111
Lutman ME, Grandori F (1999) Screening for neonatal hearing defects European. Eur J Pediatr 158:95–96
Kemper A, Downs S (2000) A cost-effectiveness analysis of newborn hearing screening strategies. Arch Pediatr Adolesc Med 154(5):484–488
Yousefi J, Ajalloueyan M, Amirsalari S, Hassanali M (2013) The specificity and sensitivity of transient otoacustic emission in neonatal hearing screening compared with diagnostic test of auditory brain stem response in Tehran hospitals. Iran J Pediatr 23(2):199–204
Kezirian E, White K, Yueh B, Sullivan S (2001) Cost and cost-effectiveness of universal screening for hearing loss in newborns. Otolaryngol Head Neck Surg 124:359–367
World Health Organization (2010). Newborn and infant hearing screening—current issues and guiding principles for action-http://www.who.int/blindness/publications/Newborn_and_Infant_Hearing_Screening_Report.pdf Accessed 10 Sept 2014
Beauchamp T, Childress J (1994) Principles of biomedical ethics, 4th edn. Oxford University Press, New York
Lester EB, Dawson JD, Gantz BJ, Hansen MR (2011) Barriers to the early cochlear implantation of deaf children. Otol Neurotol 32(3):406–412
Nunes R (2006) Deafness, genetics and dysgenics. Med Health Care Philos 1:25–31
Meadow K (1984) Social adjustment of preschool children: deaf and hearing: with or without other handicaps. Topics Early Child Spec Edu 3:27–40
Lane H (1992) The mask of benevolence—disabling the deaf community. Vintage Books, New York
Davis D (1997) Genetic dilemmas and the child’s right to an open future. Hastings Cent Rep 27:7–15
Gené-Badiaa J, Gallob P, Hernández-Quevedoc C, García-Armestod S (2012) Spanish health care cuts: penny wise and pound foolish? Health Policy 106:23–28
Giulio de Belvisa A, Ferrèb F, Specchiaa ML, Valerioa L, Fattoreb G, Ricciardi W (2012) The financial crisis in Italy: implications for the healthcare sector. Health Policy 106:10–16
Reevesa A, McKeeb M, Basub S, Stucklera D (2014) The political economy of austerity and healthcare: cross-national analysis of expenditure changes in 27 European nations 1995–2011. Health Policy 115:1–8
Acknowledgments
The authors thank the Central Administration of the Health System (ACSS) (Portugal) for providing access to the database. The authors also thank Fernando Lopes for support provided by the identification of the ICD-9 codes.
Conflict of interest
The authors state that they have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duarte, I., Santos, C.C., Freitas, A. et al. Ethics, equity, and human dignity in access to health services: the case of cochlear implants in children and adolescents. Eur Arch Otorhinolaryngol 272, 1011–1019 (2015). https://doi.org/10.1007/s00405-014-3340-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3340-8