Abstract
Background
Subclinical hypothyroidism (SCH) in pregnancy is associated with adverse foetomaternal outcomes. The literature is scarce with respect to maternal and perinatal outcomes in women with mild SCH (TSH levels between 2.5–4 mIU/L).
Objectives
The primary objective of the study was to compare the pregnancy outcome between SCH and euthyroid women. The secondary objectives were to find out the proportion of women with SCH having thyroid peroxidase antibodies (TPOAb) and to see the effect of TPOAb positivity on foetomaternal outcomes.
Materials and methods
A total of 178 pregnant women were recruited in the first trimester, and those with TSH between 0.1 and 2.4 mIU/L were considered as euthyroid and 2.5–4mIU/L were labelled as SCH. Women with SCH underwent testing for TPOAb. All women were followed until delivery, and foetomaternal outcomes were assessed.
Results
Amongst SCH group, there was a significantly higher proportion of overweight and obese women (76/91 (83.51%) vs 59/87 (68%), p = 0.031). The neonatal intensive care unit (NICU) admission was higher with adjusted odds ratio of 3.24 (1.41–7.43) in women with SCH as compared to euthyroid women. Otherwise, there was no difference in foetomaternal outcomes between the two groups. The proportion of gestational diabetes mellitus, intrauterine growth retardation and still birth were higher in SCH women with TPOAb as compared to euthyroid. Amongst SCH women, the proportion of induced labour was lower (aOR:0.27 (0.08–0.93) whereas the proportion of stillbirth and low APGAR scores were higher in TPOAb-positive women with a statistically significant difference and adjusted odds ratio (aOR:20.18 (1.84–220.83)) and (aOR:4.77 (1.06–21.3)), respectively, when compared to TPOAb-negative women.
Conclusion
There appears to be no difference in pregnancy outcomes between women with SCH and euthyroid women except higher NICU admission in SCH group. Future multi-centre large prospective studies are required to understand better about the pregnancy outcomes in these women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1. Pregnancy outcome between subclinical hypothyroidism (TSH 2.5-4mIU/L) and euthyroid women is still a matter of debate which requires large multicentric studies in the Indian population to evaluate the difference better. | |
2. If there is no difference in pregnancy outcome between the two groups, then there will be no need for TPOAb testing among SCH (TSH 2.5−4ImU/L ) and the upper limit of normal range of TSH can be safely increased to 4mIU/L for the Indian population. |
Introduction
Subclinical hypothyroidism (SCH) is characterised by high serum thyrotropin (TSH) with normal thyroxine (T4) level. In pregnancy, the prevalence of SCH ranges from 7.48% to 12.04% in India and from 1.50% to 19.60% worldwide [1, 2]. Many factors like ethnicity, presence of environmental goitrogens, nutrition status including iodine intake, genetic susceptibility and diagnostic threshold of TSH can explain such wide variation in the prevalence of SCH in different population [2]. The new 2017 American Thyroid Association (ATA) guideline promotes the use of population-based reference ranges of TSH during pregnancy. However, if these reference ranges are not available, then serum TSH level of 4 mIU/L as the upper limit of normal range should be used for the first trimester, which is higher than the 2.5 mIU/L cutoff based on 2011 ATA guidelines [3, 4]. The levothyroxine (LT4) therapy is recommended for SCH women with a TSH greater than 4 mIU/L in first trimester according to 2017 ATA guideline. In addition, LT4 therapy may be considered for thyroid peroxidase antibody (TPOAb)-positive women with TSH between 2.5 mIU/L and 4 mIU/L, and treatment is not required if they are TPOAb negative. The latter are, however, weak recommendations based on low-to-moderate-quality evidence. The relationship between TSH and free T4 (FT4) was analysed amongst 46,262 pregnant women [5]. FT4 was relatively constant when serum TSH levels were between 0.5 and 4 mIU/L. However, FT4 levels began to decrease significantly when TSH levels were above 4 mIU/L. This finding suggests that the benefits of LT4 supplementation may not be obvious for pregnant women when the diagnostic cutoff of TSH is less than 4.0mIU/L, e.g. 2.5 mIU/L to 4 mIU/L.
Few studies [6,7,8,9] showed that SCH (TSH between 2.5–4 mIU/L) was associated with several obstetric complications, including miscarriage, gestational hypertension(HTN), pre-eclampsia, placental abruption, gestational diabetes mellitus (GDM), intrauterine growth restriction (IUGR), preterm birth and low birth weight (LBW), whereas others [10,11,12,13] did not reveal it in comparison to euthyroid (TSH between 0.1–2.4 mIU/L) mothers. These conflicting results might be due to variability in timing of TSH measurements, assessment of TPOAb status and presence of other confounding factors in different studies [14]. The adjusted odds of adverse pregnancy outcomes were lower in treated women than in untreated women if their pre-treatment TSH concentration was 4.1–10 mIU/L, but not if it was 2.5–4.0 mIU/L [15,16,17,18]. Rather, LT4 therapy increases the risk of poor pregnancy outcomes like preterm delivery, GDM, gestational HTN and preeclampsia in SCH women with TSH between 2.5 and 4.0 mIU/L [19]. However, when a meta-analysis was performed using a TSH diagnostic cutoff of 4.0 mIU/L, pregnant patients with SCH had higher risk of hypertensive disorders of pregnancy both above and below this threshold compared with euthyroid pregnant women [20]. In addition, the presence of TPOAb also affects the foetomaternal outcomes like GDM and decreased foetal growth in SCH mothers as shown in meta-analysis by Derakshan et al. [21] and Kent et al. [22]
Moreover, there is a paucity of data in the Indian population [16]. And there is still insufficient evidence in the current literature whether the 2017 ATA guidelines are applicable to Indian pregnant women. With the goal of validating the current ATA guidelines amongst Indian subjects, this study was performed with the aim of comparing the pregnancy outcomes between SCH with and without TPOAb and euthyroid women.
Materials and methods
This prospective cohort study was carried out in the department of obstetrics and gynaecology of a tertiary care centre in India from January 2020 to September 2021. The study protocol was registered with Clinical Trial Registry of India [Trial REF/2020/09/036436] after getting approval from the ethics committee of the institute [JIP/IEC/2019/441]. The primary objective of the study was to compare the pregnancy outcome between SCH and euthyroid women. The secondary objectives were to find out the proportion of women with SCH having TPOAb, and to see the effect of TPOAb positivity on foetomaternal outcomes. Pregnant women with TSH levels between 2.5 and 4 mIU/L were labelled as SCH, and subjects with TSH levels between 0.1 and 2.4 mIU/L were considered as euthyroid. All of them had normal gestational age-adjusted serum total T4 level [4]. Sample size was calculated using Open Epi software version 3.1 by considering the expected proportion of miscarriage [23] of 2.2% amongst euthyroid and 15.2% amongst women with SCH with 95% CI and power of 80%. The total sample size was estimated to be 178.
Pregnant women attending antenatal outpatient department or admitted in antenatal ward of the institute fulfilling the following inclusion and exclusion criteria were selected. The inclusion criteria were pregnant (< 14 weeks of gestation) women aged > 18 years with serum thyroid stimulating hormone (TSH) levels between 0.1 and 4 mIU/L. Women with history of thyroid disorder, taking medications for hypo/hyperthyroidism, overt diabetes mellitus, chronic hypertension, recurrent pregnancy loss and conception by assisted reproductive technology were excluded from the study. Women diagnosed as SCH based on TSH levels were not treated with antithyroid drugs in the study, and if found to be on treatment with antithyroid drugs during the course of study, they were excluded. Written informed consent was obtained from all the study subjects before recruitment. Detailed history pertaining to demographic factors, obstetric history (present and past pregnancy details including history of infertility and treatment received), menstrual, personal and family history were noted in a predesigned proforma. Gestational age was calculated as per last menstrual period or early dating ultrasonographic scan depending on the reliability. General physical examination including pallor, goitre, pulse rate and blood pressure were noted. Height and weight of the study subjects were also recorded. Body mass index (BMI) was calculated by dividing the pre-pregnancy weight in kilograms by the height in meters squared. BMI between 18.5 and 22.9 kg/m2 was considered as normal, 23 and 24.9 kg/m2 as overweight, and ≥ 25 kg/m2 as obesity according to Asian Indian guidelines [24]. All the subjects were followed up till delivery, and the foetomaternal outcomes were noted.
Hypertensive disorders of pregnancy include preeclampsia and gestational HTN. Gestational HTN is a condition with a blood pressure of more than 140/90 mm Hg in two occasions 4 h apart with or without proteinuria after 20 weeks of gestation in a previously normotensive women. Pre-eclampsia includes gestational HTN with proteinuria or in the absence of proteinuria a new onset thrombocytopenia, renal insufficiency, impaired liver function, pulmonary oedema or headache. GDM is a condition with carbohydrate intolerance with recognition or onset during pregnancy. Miscarriage is defined as expulsion of products of conception before the period of viability. Oligohydramnios is the condition where the amniotic fluid index is less than 5 cm in a term pregnancy. Intrauterine growth restriction(IUGR) is defined as failure of foetus to achieve its genetic growth potential. Premature rupture of membrane (PROM) is a condition where the amniotic membranes rupture before the onset of labour. Labour onset can be spontaneous or induced. Induction of labour is defined as initiation of uterine contractions after the period of viability prior to spontaneous onset of labour. Preterm labour is defined as onset of uterine contractions before 37 completed weeks but may not always end up with the delivery of the baby. Preterm delivery includes those pregnancies with delivery before 37 completed weeks of gestation. Instrumental delivery includes all the deliveries where either forceps or ventouse was used to deliver the foetal head. Caesarean section is delivery of the foetus after the period of viability through abdominal and uterine incisions.
After delivery, the neonatal birth weight, head circumference(HC) and APGAR scores (1 and 5 min) were recorded, and low APGAR score was defined as < 7. Neonatal resuscitation and decision for neonatal intensive care unit (NICU) admission were taken by the neonatologist. We categorized our babies as less than 2.5 kg, 1.5 kg and 1 kg as low birth weight(LBW), very low birth weight (VLBW) and extremely low birth weight (ELBW), respectively. Stillbirth is defined as death foetus beyond 28 weeks of gestation. Respiratory distress syndrome (RDS) is a condition that develops due to pulmonary immaturity and surfactant deficiency. Neonatal sepsis is a clinical syndrome of systemic illness with bacteremia in the first 28 days of life. Congenital anomalies are structural defects that are present at birth. Low HC was defined as HC ≤ 32 cm [25].
The thyroid function test (TFT) that includes serum TSH and total thyroxine (T4) and TPOAb were done in duplication in endocrinology laboratory of the institute. Five ml. of venous blood was drawn from ante-cubital vein of the subjects, and was processed by the chemiluminescent assay system (ADVIA Centaur XP Immunoassay System, Siemens Healthcare Global, USA) in accordance with the manufacturer’s instructions. The total coefficient of variation of TSH and total T4 assay was 3.17% and 5.55%, respectively. The cutoff to indicate positivity for TPOAb was 60 U/mL, which was estimated only in pregnant women with SCH.
Continuous variables were represented as mean ± SD or median with inter-quartile range (IQR), depending on the variable’s distribution. The normality of the data was assessed using appropriate tests. Categorical variables were expressed as a percentage and were analysed using Chi-squared or Fisher’s test. Independent Student’s t test and Mann–Whitney U test were done to compare the continuous variables based on the normality. Both unadjusted and maternal BMI-adjusted odds ratio (aOR) with 95% confidence intervals (95% CIs) for foetomaternal outcomes were calculated. P value < 0.05 was taken as statistically significant. The data were analysed using STATA 14.0.
Results
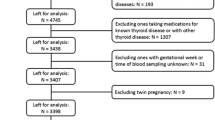
The study included a total of 87 euthyroid and 91 SCH pregnant women as shown in Fig. 1. The mean age of the study participants was 25.91 years, and 60% of the study population were primigravida. SCH women had higher BMI compared to euthyroid subjects (27 ± 5.2 vs. 25 ± 4.5 kg/m2, P = 0.01) as shown in Table 1. Only 14% SCH women had normal BMI in comparison to 30% amongst euthyroid antenatal mothers (P = 0.03). Only 14 (15.38%) pregnant women with SCH had positive TPOAb.
Table 2 shows the comparison of maternal outcomes between pregnant women with SCH and euthyroid mothers. There was no overall difference in maternal outcomes between euthyroid and SCH women. The need for induced labour was twice more common amongst pregnant mothers with TPOAb−ve SCH compared to euthyroid subjects as shown in Table 3. However, TPOAb-positive SCH women have higher risk of both GDM (aOR: 3.92 (1.17–13.08)) and IUGR (aOR: 4.79 (1.48–15.56)) compared to euthyroid mothers as shown in Table 4.
Table 5 shows the comparison of perinatal outcomes between pregnant women with SCH and euthyroid mothers. NICU admission was more in women with SCH as compared to euthyroid mothers with aOR of 3.24 (1.41–7.43). Similar result was also found amongst TPOAb-ve SCH mothers as shown in Table 6. Out of 21 neonates with LBW in euthyroid group, 3 and 4 babies were VLBW and ELBW, respectively. Similarly, out of 24 neonates with LBW in SCH group, 3 and 2 babies were VLBW and ELBW, respectively. No neonate had birth weight > 4 kg in our study. There were two stillbirths in the euthyroid group out of which one foetus had anencephaly and the other foetus was born to a GDM mother. There were four stillbirths in SCH group; the cause being RDS, birth asphyxia, meconium aspiration syndrome and the other one was unknown in whom the mother had GDM. Six and five neonates had congenital anomalies in euthyroid and SCH women, respectively. The congenital anomalies present in euthyroid group were cloacal dystrophy, lateral ventricle dilatation, cleft lip and palate, anencephaly, foetal intraabdominal cystic lesion, and hypospadias. Similarly, the congenital anomalies present in SCH group were autosomal recessive polycystic kidney disease, bilateral hydroureteronephrosis, foetal right lung cystic lesion, choroid plexus cyst and congenital diaphragmatic hernia. The proportion of still birth (aOR:12.01 (1.74–82.64)) was higher in SCH women with TPOAb as compared to euthyroid women as shown in Table 7.
Table 8 compares the maternal outcomes amongst SCH TPOAb-positive with SCH TPOAb-negative women which shows no statistically significant difference except in terms of induced labour where the induction rates were lower in TPOAb-positive women and this difference was statistically significant (aOR:0.27 (0.08–0.93)).Comparing the perinatal outcomes amongst SCH women with TPOAb positive and TPOAb negative, the proportion of stillbirth and low APGAR scores were higher in TPOAb-positive women with a statistically significant difference (aOR:20.18 (1.84–220.83)) and (aOR:4.77 (1.06–21.3)), respectively. There was no statistically significant difference in the other perinatal outcome between the two groups as elicited in Table 9.
Discussion
A total of 178 pregnant women (87 euthyroid and 91 SCH) were recruited in the early pregnancy in this study. SCH women had higher BMI with more proportion of obese women when compared to euthyroid subjects. High BMI during early pregnancy increases the risk of maternal thyroid dysfunction during pregnancy. The possible mechanism is due to the effect of adipokine like leptin on hypothalamus–pituitary–thyroid axis. [16]
The neonatal intensive care unit (NICU) admission was higher (25/88 (28.4%) vs 10/82 (12.2%); P = 0.01) in women with SCH as compared to euthyroid women in this study. This can be explained due to increased proportion of obstetric complications amongst them such as GDM, hypertensive disorders, oligohydramnios, IUGR and induced labour amongst women with SCH when compared to euthyroid women. There were five miscarriages in euthyroid subjects and three in SCH women. The maternal BMI-adjusted OR for NICU admission was 3.24 (1.41–7.43) in the SCH women. Otherwise, there was no difference in foetomaternal outcomes between the two groups. Similar result was found in a cross-sectional study by Sitoris et al. [7] The pregnancy outcomes were compared between 1281 euthyroid (TSH < 2.51 mIU/L without thyroid autoimmunity) and 140 SCH (TSH 2.51–3.7 mIU/L) pregnant women. SCH mothers had higher risk of both NICU admission(aOR 19.36 (CI 1.18–316.97)) and LBW babies (21.38 (CI 1.29–353.39)). In a retrospective study by Arbib et al [6], 3231 euthyroid (TSH levels between 0.1mIU/L and 2.5 mIU/L) and 796 SCH (TSH levels between 2.5 mIU/L and 4 mIU/L) pregnant women were included. There was an increased risk (aOR 1.81, 95% CI 1.0–3.28) of only preterm delivery before 34 gestational weeks in SCH mothers compared to euthyroid subjects.
The need for both induced labour and NICU admission was more common amongst pregnant mothers with TPOAb−ve SCH compared to euthyroid subjects in our study. Amongst SCH women with TPOAb positive, there was decreased need for induced labour when compared to TPOAb-negative women. The possible explanation is the association of thyroid abnormalities with uterine dysfunction. Mothers with TSH 2.5 to 4.08 mIU/L and TPOAb−ve during early pregnancy was associated with higher risk of both miscarriages, i.e. 1.58 (1.17–2.13) and maternal composite outcomes, i.e. 1.27 (1.04–1.54) compared to euthyroid status (0.23 ≤ TSH ≤ 2.5 mIU/L) in a retrospective study by Zhang et al. [8]. The occurrence of one or more of maternal outcomes was defined as the presence of maternal composite outcomes in their study. Except PIH (2.8 vs. 1.5%, OR = 2.99, 95% CI = 1.24–7.23), no correlations were observed on the adverse pregnancy outcomes between the 971 euthyroid (0.27–2.5 mIU/L) and 433 SCH (2.5–4.0 mIU/L) TPOAb−ve pregnant women, after adjustment for potential confounders in a study by Li et al. [12]. Impaired endothelium-related vasodilation due to decreased production of nitric oxide is the possible mechanism of SCH induced PIH [26]. However, no differences in the prevalence of adverse pregnancy outcomes were observed between 172 SCH (2.5 < TSH ⩽4.0 mIU/l) and 2161 euthyroid (0.27 < TSH ⩽2.5 mIU/l) women amongst a TPOAb-negative population in a retrospective study by Zhu et al. [13]. There were also no associations between TPOAb-negative women with TSH concentration between 2.5 and 4.0 mIU/L during their first trimesters and the incidences of adverse pregnancy outcomes in various studies [10,11,12]. However, the results were not controlled for other confounding factors in few of these studies.
The proportion of GDM, IUGR and still birth were higher in SCH women with TPOAb as compared to euthyroid women in our study. Similarly, SCH with positive antithyroid autoantibodies showed markedly increased GDM risk (OR 3.22, 95% confidence interval 1.72–6.03, I2 = 55%) in a meta-analysis by Jia et al. [27]. Women with TSH levels > 4.0 mIU/L have an increased odds of GDM regardless of thyroid autoimmunity status but at TSH levels < 4.0 mIU/L, GDM is dependent on thyroid antibody status in a meta-analysis by Kent et al. [22]. Presence of TPOAb may lead to the progressive increase in TSH during pregnancy, and thyroid hormone affects both insulin production from beta cells in islets and insulin sensitivity at peripheral tissue level [13, 28]. This might be responsible for high prevalence of GDM amongst SCH pregnant women in presence of thyroid autoimmunity. TPOAb has the ability to cross the placenta and affects foetal growth [29, 30]. Each 1 SD increase in maternal TSH concentration was associated with a 6 g lower birthweight (−10 g to −2 g; P = 0·0030), with higher effect estimates in TPOAb-positive women than for women who were Ab negative as shown in a meta-analysis by Derakshan et al. [21]. SCH is associated with IUGR (OR = 1.54; 95% CI, 1.06–2.25); however, TPOAb positivity does not affect the risk of IUGR as found in a meta-analysis by Tong et al. [31]. This may be due to the sensitizing action of thyroid hormone on growth hormone and insulin-like growth factor-1 affecting the foetal growth during intrauterine life irrespective of thyroid Ab status [32]. But, none of the foetomaternal outcomes was different between TPOAb + ve SCH and euthyroid pregnant mothers in a study by Zhang et al. [8]. The implications from our study is that SCH appears to have no influence on adverse pregnancy outcomes except a positive association with the NICU admission amongst them. Amongst SCH with TPOAb positive, there was a positive association with stillbirth and low APGAR scores when compared to TPOAb-negative women after adjusting for BMI. There appears to be a higher proportion of overweight and obese women amongst the SCH women which emphasises the need for counselling about diet and exercise. Advice regarding optimisation of BMI prior to planning pregnancy prevents derangement of thyroid function in pregnancy and good foetomaternal outcomes.
Our study has few strength and limitations. This is the first study in South Indian population to evaluate pregnancy outcomes in women with SCH with and without TPOAb where there is lack of published data. As there was a difference in BMI amongst the study subjects, it was adjusted in both euthyroid and SCH women to study the association in foetomaternal outcomes. In addition, the prospective nature of the study adds to the strengths. Since this study population was recruited from a tertiary hospital, the pregnancy outcomes may not reflect all women with SCH. The extent of derangement in thyroid function amongst women with SCH and association with NICU admission amongst babies born to them requires more prospective studies in the future with a large sample size. Moreover, in our study, there is a small sample size in SCH women with TPOAb and there is a lack of follow-up of neurocognitive development of infants. We also could not estimate TPOAb status amongst euthyroid subjects.
Conclusion
There appears to be no difference in pregnancy outcomes between women with SCH and euthyroid women except higher NICU admission in SCH group. Our study is not powered enough to compare the effect of TPOAb on foetomaternal outcomes. Future prospective studies with larger sample size are required to understand better about the pregnancy outcomes in SCH (TSH levels between 2.5–4mIU/L) with and without TPOAb.
Data availability
Not applicable.
References
Yadav V, Dabar D, Goel AD, Bairwa M, Sood A, Prasad P et al (2021) Prevalence of Hypothyroidism in Pregnant Women in India: A Meta-Analysis of Observational Studies. J Thyroid Res 19(2021):5515831. https://doi.org/10.1155/2021/5515831
Dong AC, Stagnaro-Green A (2019) Differences in Diagnostic Criteria Mask the True Prevalence of Thyroid Disease in Pregnancy: A Systematic Review and Meta-Analysis. Thyroid 29(2):278–289. https://doi.org/10.1089/thy.2018.0475
Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, Nixon A, Pearce EN, Soldin OP, Sullivan S, Wiersinga W (2011) American Thyroid Association Taskforce on Thyroid Disease During Pregnancy and Postpartum. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid 10:1081–1125. https://doi.org/10.1089/thy.2011.0087
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, Grobman WA, Laurberg P, Lazarus JH, Mandel SJ, Peeters RP, Sullivan S (2017) 2017 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid 27(3):315–389. https://doi.org/10.1089/thy.2016.0457
Yang X, Meng Y, Zhang Y, Zhang C, Guo F, Yang S, Ding R, Fan JX (2019) Thyroid function reference ranges during pregnancy in a large Chinese population and comparison with current guidelines. Chin Med J (Engl) 132(5):505–511. https://doi.org/10.1097/CM9.0000000000000051
Arbib N, Hadar E, Sneh-Arbib O, Chen R, Wiznitzer A, Gabbay-Benziv R (2017) First trimester thyroid stimulating hormone as an independent risk factor for adverse pregnancy outcome. J Matern Fetal Neonatal Med 30(18):2174–2178. https://doi.org/10.1080/14767058.2016
Sitoris G, Veltri F, Kleynen P, Cogan A, Belhomme J, Rozenberg S, Pepersack T, Poppe K (2020) The Impact of Thyroid Disorders on Clinical Pregnancy Outcomes in a Real-World Study Setting. Thyroid 30(1):106–115. https://doi.org/10.1089/thy.2019.0199
Zhang Y, Sun W, Zhu S, Huang Y, Huang Y, Gao Y, Zhang J, Yang H, Guo X (2020) The Impact of Thyroid Function and TPOAb in the First Trimester on Pregnancy Outcomes A Retrospective Study in Peking. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgz167
Li MF, Ma L, Feng QM, Zhu Y, Yu TP, Ke JF, Zhang ZH, Liu Y, Li LX (2020) Effects of Maternal Subclinical Hypothyroidism in Early Pregnancy Diagnosed by Different Criteria on Adverse Perinatal Outcomes in Chinese Women With Negative TPOAb. Front Endocrinol (Lausanne) 8(11):580380
Rosario PW, Carvalho M, Calsolari MR (2016) TSH reference values in the first trimester of gestation and correlation between maternal TSH and obstetric and neonatal outcomes: a prospective Brazilian study. Arch Endocrinol Metab 60(4):314–318. https://doi.org/10.1590/2359-3997000000132
Veltri F, Kleynen P, Grabczan L, Salajan A, Rozenberg S, Pepersack T, Poppe K (2018) Pregnancy outcomes are not altered by variation in thyroid function within the normal range in women free of thyroid disease. Eur J Endocrinol 178(2):189–197. https://doi.org/10.1530/EJE-17-0628
Li P, Lin S, Li L, Cui J, Zhou S, Fan J (2018) Effect of mildly elevated thyroid-stimulating hormone during the first trimester on adverse pregnancy outcomes. BMC Endocr Disord 18(1):64. https://doi.org/10.1186/s12902-018-0294-7
Zhu P, Chu R, Pan S, Lai X, Ran J, Li X (2021) Impact of TPOAb-negative maternal subclinical hypothyroidism in early pregnancy on adverse pregnancy outcomes. Ther Adv Endocrinol Metab 28(12):20420188211054690. https://doi.org/10.1177/20420188211054690
Lee SY, Pearce EN (2022) Assessment and treatment of thyroid disorders in pregnancy and the postpartum period. Nat Rev Endocrinol 18(3):158–171. https://doi.org/10.1038/s41574-021-00604-z
Maraka S, Mwangi R, McCoy RG, Yao X, Sangaralingham LR, Singh Ospina NM, O’Keeffe DT, De Ycaza AE, Rodriguez-Gutierrez R, Coddington CC, Stan MN, Brito JP, Montori VM (2017) Thyroid hormone treatment among pregnant women with subclinical hypothyroidism: US national assessment. BMJ 25(356):i6865. https://doi.org/10.1136/bmj.i6865
Ram U, Thirunavukkarasu M, Shyam K, Ghebremichael-Weldeselassie Y, Sukumar N, Saravanan P (2023) Effects of treating subclinical hypothyroidism in pregnancy in India: Are we treating too many for little gain? A retrospective cohort study. Int J Gynaecol Obstet. https://doi.org/10.1002/ijgo.15021
Nazarpour S, Ramezani Tehrani F, Simbar M, Tohidi M, AlaviMajd H, Azizi F (2017) Effects of levothyroxine treatment on pregnancy outcomes in pregnant women with autoimmune thyroid disease. Eur J Endocrinol 176(2):253–265. https://doi.org/10.1530/EJE-16-0548
Nazarpour S, Ramezani Tehrani F, Simbar M, Tohidi M, Minooee S, Rahmati M, Azizi F (2018) Effects of Levothyroxine on Pregnant Women With Subclinical Hypothyroidism, Negative for Thyroid Peroxidase Antibodies. J Clin Endocrinol Metab 103(3):926–935. https://doi.org/10.1210/jc.2017-01850
Gietka-Czernel M, Glinicki P (2021) Subclinical hypothyroidism in pregnancy: controversies on diagnosis and treatment. Pol Arch Intern Med 131(3):266–275. https://doi.org/10.20452/pamw.15626
Han Y, Wang J, Wang X, Ouyang L, Li Y (2022) Relationship Between Subclinical Hypothyroidism in Pregnancy and Hypertensive Disorder of Pregnancy: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne) 8(13):823710. https://doi.org/10.3389/fendo.2022.823710
Derakhshan A, Peeters RP, Taylor PN, Bliddal S, Carty DM, Meems M, Vaidya B, Chen L, Knight BA, Ghafoor F, Popova PV, Mosso L, Oken E, Suvanto E, Hisada A, Yoshinaga J, Brown SJ, Bassols J, Auvinen J, Bramer WM, López-Bermejo A, Dayan CM, French R, Boucai L, Vafeiadi M, Grineva EN, Pop VJM, Vrijkotte TG, Chatzi L, Sunyer J, Jiménez-Zabala A, Riaño I, Rebagliato M, Lu X, Pirzada A, Männistö T, Delles C, Feldt-Rasmussen U, Alexander EK, Nelson SM, Chaker L, Pearce EN, Guxens M, Steegers EAP, Walsh JP, Korevaar TIM (2020) Association of maternal thyroid function with birthweight: a systematic review and individual-participant data meta-analysis. Lancet Diabetes Endocrinol 8(6):501–510. https://doi.org/10.1016/S2213-8587(20)30061-9
Kent NL, Young SL, Akison LK, Cuffe JSM (2021) Is the link between elevated TSH and gestational diabetes mellitus dependant on diagnostic criteria and thyroid antibody status: a systematic review and meta-analysis. Endocrine 74(1):38–49. https://doi.org/10.1007/s12020-021-02733-x
Liu H, Shan Z, Li C, Mao J, Xie X, Wang W, Fan C, Wang H, Zhang H, Han C, Wang X, Liu X, Fan Y, Bao S, Teng W (2014) Maternal subclinical hypothyroidism, thyroid autoimmunity, and the risk of miscarriage: a prospective cohort study. Thyroid 24(11):1642–1649. https://doi.org/10.1089/thy.2014.0029
Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, Joshi SR, Sadikot S, Gupta R, Gulati S, Munjal YP (2009) Concensus Group. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 57:163–170 (PMID: 19582986)
Cunningham FG, Leveno JK, Bloom SL, Spong YC, Jodi S. Dashe, Hoffman LB, et al. The thyroid disorders. In: Cunningham FG, Leveno JK, Bloom SL, Spong YC, Jodi S. Dashe, Hoffman LB, Brian editors. Williams Obstetrics. 25 th Edition. New York: McGraw-Hill; 2014:637–53.
Taddei S, Caraccio N, Virdis A, Dardano A, Versari D, Ghiadoni L, Salvetti A, Ferrannini E, Monzani F (2003) Impaired endothelium-dependent vasodilatation in subclinical hypothyroidism: beneficial effect of levothyroxine therapy. J Clin Endocrinol Metab 88(8):3731–3737. https://doi.org/10.1210/jc.2003-030039
Jia M, Wu Y, Lin B, Shi Y, Zhang Q, Lin Y, Wang S, Zhang Y (2019) Meta-analysis of the association between maternal subclinical hypothyroidism and gestational diabetes mellitus. Int J Gynaecol Obstet 144(3):239–247. https://doi.org/10.1002/ijgo.12751
Mir F, Chiti H, Mazloomzadeh S (2022) Short-Term Adverse Pregnancy Outcomes in Women with Subclinical Hypothyroidism: A Comparative Approach of Iranian and American Guidelines. J Thyroid Res 5(2022):9315250. https://doi.org/10.1155/2022/9315250
Balucan FS, Morshed SA, Davies TF (2013) Thyroid autoantibodies in pregnancy: their role, regulation and clinical relevance. J Thyroid Res 2013:182472. https://doi.org/10.1155/2013/182472
Seror J, Amand G, Guibourdenche J, Ceccaldi PF, Luton D (2014) Anti-TPO antibodies diffusion through the placental barrier during pregnancy. PLoS ONE 9(1):e84647. https://doi.org/10.1371/journal.pone.0084647
Tong Z, Xiaowen Z, Baomin C, Aihua L, Yingying Z, Weiping T, Zhongyan S (2016) The Effect of Subclinical Maternal Thyroid Dysfunction and Autoimmunity on Intrauterine Growth Restriction: A Systematic Review and Meta-Analysis. Medicine (Baltimore) 95(19):e3677. https://doi.org/10.1097/MD.0000000000003677
Blazer S, Moreh-Waterman Y, Miller-Lotan R, Tamir A, Hochberg Z (2003) Maternal hypothyroidism may affect fetal growth and neonatal thyroid function. Obstet Gynecol 102(2):232–241. https://doi.org/10.1016/s0029-7844(03)00513-1
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. Priyanka R. The first draft of the manuscript was written by Dr. Priyanka and Dr. Sahoo, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the institution.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
No images of participants were used in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Priyanka, R., Sagili, H., Sahoo, J. et al. Pregnancy outcome in subclinical hypothyroidism with and without thyroid peroxidase antibodies—a prospective cohort study. Arch Gynecol Obstet 310, 1935–1944 (2024). https://doi.org/10.1007/s00404-024-07659-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-024-07659-z