Abstract
Objective
Cesarean scar pregnancy (CSP) is a potentially life-threatening disease that has been steadily increasing in prevalence. Pregnancy termination is usually recommended given the risk of life-threatening complications. In some cases, patients refuse to terminate viable CSPs, even after counseling. Recent studies report that, even with a high burden of possible complications and maternal morbidity, many CSPs progress to live, close to term births. The aim of this study is to further demonstrate the natural history of viable cesarean scar pregnancies.
Methods
We conducted a systematic review of original studies reporting cases of expectant management of CSPs with positive fetal heartbeats.
Results
After selection, 28 studies were included in the review, with a total of 398 cases of CSP, 136 managed expectantly and 117 with positive fetal heartbeat managed expectantly. This study confirmed that the majority of patients experience live births, as 78% of patients selected for expectant management experienced live births at or close to term, with 79% developing morbidly adherent placenta, 55% requiring hysterectomy, and 40% having severe bleeding.
Discussion
The optimal management protocol for CSP is still to be defined and more studies are needed to further elucidate this rare but rising disease. Our study provides information on the natural history of untreated CSPs and suggests that termination may not be the only option offered to the patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
This review helps broaden the knowledge of cesarean scar pregnancies' natural history and contributes to the decision making of the clinician on whether to recommend termination in all cases. |
Introduction
Cesarean scar pregnancy (CSP) is a potentially life-threatening disease that has been steadily increasing in prevalence, following the worldwide rise of cesarean delivery [1, 2]. Defined as the development of the gestational sac in the hysterotomy scar, it is now considered an early form of morbidly adherent placenta (MAP) [3]. The risks of CSP include severe hemorrhage, uterine rupture, prematurity, MAP, hysterectomy, development of arteriovenous malformation and maternal death [4, 5].
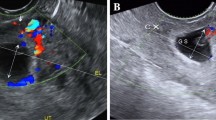
The clinical presentation of CSP can vary greatly, as it may be asymptomatic in early pregnancy [1]. CSP can be diagnosed by abdominal or transvaginal ultrasound by the identification of an empty endometrial cavity, a placenta or gestational sac implanted in the anterior segment, in some cases filling the niche of the scar or bulging from it, and a thin or absent myometrial layer between gestational sac and bladder [1]. However, some cases can remain undiagnosed and present themselves as severe vaginal bleeding and abdominal pain [2].
Considering the severity of the possible outcomes, screening for early signs of CSP and MAP is now recommended, with a detailed evaluation of the uterus in the midsagittal plane to document the gestational sac location by transvaginal ultrasound [5].
Following diagnosis, the patient should thoroughly be counseled on the possible outcomes and risks involved in this disease [6]. Many treatment options have been proposed, but there is no universally agreed upon management protocol [6, 7]. In the past, pregnancy termination was usually recommended given the risk of life-threatening complications, although recent evidence suggests that expectant management frequently results in live births complicated by placenta accreta spectrum disorder [7, 8].
It is of utmost importance to determine the pregnancy viability. If there is no yolk sac and/or embryo and/or fetal heartbeat, and this remains to be the case in regular new ultrasound examinations, the management could be restricted to sonographic and biochemical follow up [6]. Many studies have shown safety in conservative management of non-viable CSPs, with uncommon adverse outcomes [6, 9].
In some cases, however, patients refuse to terminate viable CSPs, even after counseling, based on their personal beliefs or their reluctance to terminate a pregnancy conceived after a long wait or by medical infertility treatments. Recent studies report that, even with a high burden of possible complications and maternal morbidity, many CSPs progress to live, close to term births [6]. This knowledge changes the options given during patient counseling—she must be informed that a placenta accreta and cesarean-hysterectomy may probably occur, but expectant management is a possibility [2, 6].
The aim of this systematic review is to update knowledge of the natural history of expectant management of cesarean scar pregnancies.
Methods
Before data extraction, the review was registered with the PROSPERO International Prospective Register of Systematic Reviews (Registration No: CRD42022343548) following the PRISMA guidelines for protocols (PRISMA-P).
We conducted a systematic review of original studies reporting cases of expectant management of viable CSPs. An electronic search was performed using the MEDLINE, Embase, Web of Science and BVS databases on April 2022, utilizing combinations of MeSH terms and keywords variants for ‘Cesarean scar pregnancy’ (‘cesarean scar ectopic pregnancy’ or ‘c-section pregnancy’) and ‘expectant management’. Reference lists of relevant articles were also hand-searched. Reports were excluded if there were insufficient details of the outcomes. We considered all study designs including case reports, case series, comparative studies and controlled trials. We did not consider for inclusion other systematic or narrative reviews, editorials and opinion articles.
Study eligibility was assessed independently by 3 reviewers screening abstracts, and full text publications when required. Only full text articles in English were considered eligible for inclusion. Only studies including women diagnosed with single CSP by ultrasound, with positive fetal heartbeat and undergoing expectant management were included. Studies reporting only cases of CSP undergoing treatment were excluded, as were studies reporting only non-viable CSPs undergoing expectant management and reports of women diagnosed with heterotopic pregnancies. We included case series written by the same authors but had the care to remove the specific repeated cases when the authors made them clearly distinguishable.
The selected outcomes were uncomplicated miscarriage, complicated miscarriage (defined as the need of intervention or surgical treatment), severe bleeding (defined as the need for blood transfusions), uterine rupture, hysterectomy, live birth, MAP (diagnosed during surgery or histopathological examination), maternal death or other complications.
Results
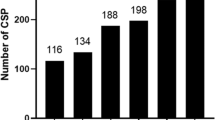
A total of 3106 articles were identified from the search, of which 104 were assessed for eligibility in full text (Fig. 1). After selection, 28 studies were included in the review, with a total of 398 cases of CSP, 136 managed expectantly and 117 with positive fetal heartbeat managed expectantly (Table 1).
The main weaknesses of the studies were the retrospective design, small sample size, lack of stratification according to position of the gestational sac and corresponding classification of the CSP, lack of detailed information on the volume of blood loss and interventions required, and incomplete information on the patients included in some studies. Also, we included case reports that could lead to publication bias.
The mean number of previous cesarean sections (CS) was rounded up whenever needed. Of all cases where the number of previous CSs were informed, the average was 1.6. Only 3 cases of CSP were reported as being a product of assisted reproduction.
Outcomes of viable CSPs managed expectantly are summarized in Table 2. Of the 117 cases of CSP with positive heartbeat managed expectantly, 6 cases experienced an uncomplicated miscarriage (5%), while 13 cases (11%) experienced complicated miscarriages that required treatment and surgical intervention. Uterine rupture occurred in 11 cases (9%), all required hysterectomies. Severe bleeding was reported in 47 cases (40%), either previous to or during surgeries. Of all cases, in 65 women hysterectomies were performed (55%).
Ninety-two live births were the result of the 117 cases of viable CSPs (78%). Morbidly adherent placenta was reported in 81 cases, diagnoses either during surgery or by histopathological evaluation (69%). No maternal deaths were reported.
Other complications were reported in 11 cases, being prematurity the most frequent complication. One study reported 2 cases of infection leading to sepsis. One case reported a live fetus with prenatal diagnosis of neural tube defect sequence-type myelomeningocele-anencephaly-iniencephaly, but the patient refused termination due to religious beliefs, gave birth to a stillborn baby and a hysterectomy was performed. One study reported a case of preeclampsia, leading to an emergency cesarean section and hysterectomy at 29 weeks due to MAP. One study reported a case of placenta percreta, in which the placenta was implanted into the bladder.
Discussion
This study confirmed that the majority of patients experience live births, at or close to term, during expectant management of CSP (78%), which are frequently complicated by MAP (69%) and need for hysterectomy (55%). This information needs to be part of the patient counseling, to provide all the possibilities and help make an informed decision. In case the patient decides not to terminate the pregnancy, even knowing all possible outcomes, providers need to understand the natural history of CSP and how to manage it.
We found that 69% of cases progressed to MAP. Considering that other studies have demonstrated that CSP and MAP are part of the same spectrum of diseases, we believe this number may have been underestimated by publication bias or incomplete information of some reports [3, 5, 14].
There is still a high maternal morbidity related to expectant management of viable CSPs, with 40% of cases developing severe bleeding and 55% requiring hysterectomies. The risk of hysterectomy is reported to be 66% in cases of MAP [36].
Our finding of 11% cases of miscarriages in CSP patients that required surgical intervention was not higher than the need of unplanned surgical treatment in miscarriages in the general population, that can be as high as 28% [37]. However, we understand that said surgical interventions may be more severe than the usual curettage or aspiration required in the general population, as demonstrated by the 9 nine cases of uterine rupture (11%) in CSPs patients after miscarriages. This rate of uterine rupture in the first trimester was similar to that found by Cali et al (9.9% of CSP cases with positive fetal heartbeat) [2].
The strength of this study is its methodology for identifying all possible studies and the large number of cases reported of a rare disease, that even more scarcely is allowed to progress to the third trimester.
Our limitations include primarily the high risk of publication bias associated with including case reports. It is possible that only the most drastic outcomes were published or that the authors chose not to publish cases of maternal death. Also, their retrospective design and different follow up periods limit the quality of evidence.
We believe that the most relevant limitation involves the lack of stratification of the cases according to the position of the gestation sac. Some authors have already proposed classifications of CSP and their correlation likely prognosis, such as the COS criteria [34, 35]. The natural history of a pregnancy in which the gestational sac is implanted within the myometrial wall will probably progress differently than a case in which the gestational sac is implanted above the endometrial line, but most studies included have not stratified the cases as such. The position of the gestational sac in relation to the scar and the endometrial line is determinant to the pregnancy’s prognosis and natural history, therefore each classification of CSP should be treated differently [34]. Also, it is important that future studies and case reports use tools such as the COS criteria to stratify CSP cases [34].
The optimal management protocol for CSP is still to be defined and more studies are needed to further elucidate this rare but rising disease. Our study provides information on the natural history of untreated CSPs and suggests that expectant management should be offered along with termination, in the context of full informed consent about the risks and benefits of each.
Data availability
The data that support this systematic review and meta-analysis are available from the corresponding author, upon reasonable request.
References
Timor-Tritsch IE, Monteagudo A, Santos R, Tsymbal T, Pineda G, Arslan AA (2012) The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol 207(1):44.e1-44.e13. https://doi.org/10.1016/j.ajog.2012.04.018
Calì G et al (2018) Outcome of cesarean scar pregnancy managed expectantly: systematic review and meta-analysis. Ultrasound Obst Gynecol 51(2):169–175. https://doi.org/10.1002/uog.17568
Timor-Tritsch IE et al (2014) Cesarean scar pregnancy is a precursor of morbidly adherent placenta. Ultrasound Obstet Gynecol 44(3):346–353. https://doi.org/10.1002/uog.13426
Michaels AY, Washburn EE, Pocius KD, Benson CB, Doubilet PM, Carusi DA (2015) Outcome of cesarean scar pregnancies diagnosed sonographically in the first trimester. J Ultrasound Med 34(4):595–599. https://doi.org/10.7863/ultra.34.4.595
Shainker SA et al (2021) Special report of the society for maternal-fetal medicine placenta accreta spectrum ultrasound marker task force: consensus on definition of markers and approach to the ultrasound examination in pregnancies at risk for placenta accreta spectrum. Am J Obstet Gynecol 224(1):B2–B14. https://doi.org/10.1016/j.ajog.2020.09.001
Timor-Tritsch IE, Monteagudo A, Calì G, D’Antonio F, Agten AK (2019) Cesarean scar pregnancy: patient counseling and management. Obstet Gynecol Clin North Am 46(4):813–828. https://doi.org/10.1016/j.ogc.2019.07.010
Grechukhina O et al (2018) Cesarean scar pregnancy, incidence, and recurrence: 5-year experience at a single tertiary care referral center. Obstet Gynecol 132(5):1285–1295. https://doi.org/10.1097/AOG.0000000000002940
Marion LL, Meeks GR (2012) Ectopic pregnancy: history, incidence, epidemiology, and risk factors. Clin Obstet Gynecol 55(2):376–386. https://doi.org/10.1097/GRF.0b013e3182516d7b
Drever N, Bertolone J, Shawki M, Janssens S (2020) Caesarean scar ectopic pregnancy: experience from an Australian tertiary centre. Aust N Z J Obstet Gynaecol 60(3):330–335. https://doi.org/10.1111/ajo.13119
Maymon R et al (2004) Ectopic pregnancies Caesarean section scars: the 8 year experience of one medical centre. Hum Reprod 19(2):278–284. https://doi.org/10.1093/humrep/deh060
Ben Nagi J et al (2005) First-trimester cesarean scar pregnancy evolving into placenta previa/accreta at term. J Ultrasound Med 24(11):1569–1573. https://doi.org/10.7863/jum.2005.24.11.1569
El-Matary A, Akinlade R, Jolaoso A (2007) Caesarean scar pregnancy with expectant management to full term. J Obstet Gynaecol 27(6):624–625. https://doi.org/10.1080/01443610701546334
Abraham RJ, Weston MJ (2012) Expectant management of a caesarean scar pregnancy. J Obstet Gynaecol 32(7):695–696. https://doi.org/10.3109/01443615.2012.703263
Sinha P, Mishra M (2012) Caesarean scar pregnancy: a precursor of placenta percreta/accreta. J Obstet Gynaecol 32(7):621–623. https://doi.org/10.3109/01443615.2012.698665
Ahmadi F, Moinian D, Pooransari P, Rashidi Z, Haghighi H (2013) Ectopic pregnancy within a cesarean scar resulting in live birth: a case report. Arch Iran Med 16(11):679–682
Nishida R, Yamada T, Yamada T, Morikawa M, Kawaguchi S, Minakami H (2013) Viable delivery after conservative management of a cesarean scar pregnancy. J Ultrasound Med 32(9):1682–1684. https://doi.org/10.7863/ultra.32.9.1682
Riaz RM, Williams TR, Craig BM, Myers DT (2015) Cesarean scar ectopic pregnancy: imaging features, current treatment options, and clinical outcomes. Abdom Imaging 40(7):2589–2599. https://doi.org/10.1007/s00261-015-0472-2
Timor-Tritsch IE, Khatib N, Monteagudo A, Ramos J, Berg R, Kovács S (2015) Cesarean scar pregnancies: experience of 60 cases. J Ultrasound Med 34(4):601–610. https://doi.org/10.7863/ultra.34.4.601
Zosmer N, Fuller J, Shaikh H, Johns J, Ross JA (2015) Natural history of early first-trimester pregnancies implanted in cesarean scars. Ultrasound Obstet Gynecol 46(3):367–375. https://doi.org/10.1002/uog.14775
Agten AK, Monteagudo A, Timor-tritsch IE, Thilaganathan B (2020) Cesarean scar pregnancy registry: an international research platform. Ultrasound Obstet Gynecol 55(4):438–440. https://doi.org/10.1002/uog.21952
Bennett TA, Morgan J, Timor-Tritsch IE, Dolin C, Dziadosz M, Tsai M (2017) Fifth recurrent cesarean scar pregnancy: observations of a case and historical perspective. Ultrasound Obstet Gynecol 50(5):658–660. https://doi.org/10.1002/uog.17461
Hsu CC, Huang KG (2017) Evolving cesarean scar pregnancy into morbidity adherent placenta—evidence from serial ultrasound examination. J Med Ultrasound 25(1):47–51. https://doi.org/10.1016/j.jmu.2016.11.002
Tamada S et al (2017) Successful pregnancy located in a uterine cesarean scar: a case report. Case Rep Womens Health 14:8–10. https://doi.org/10.1016/j.crwh.2017.03.003
Harb HM et al (2018) Caesarean scar pregnancy in the UK: a national cohort study. BJOG 125(13):1663–1670. https://doi.org/10.1111/1471-0528.15255
Ramkrishna J, Kan G, Reidy K, Ang W, Palma-Dias R (2018) Comparison of management regimens following ultrasound diagnosis of nontubal ectopic pregnancies: a retrospective cohort study. BJOG 125(5):567–575. https://doi.org/10.1111/1471-0528.14752
Lòpez M, Nieto A, Arango J, Quintero J, Zambrano M, Lòpez J (2019) Cesarean scar pregnancy with progression to abnormally invasive placenta; expectant management according to will of patient: report of a case and literary review. Placenta 83:e102. https://doi.org/10.1016/j.placenta.2019.06.323
Orhan A, Kasapoğlu I, Çetinkaya Demir B, Özerkan K, Duzok N, Uncu G (2019) Different treatment modalities and outcomes in cesarean scar pregnancy: a retrospective analysis of 31 cases in a university hospital. Ginekol Polska 90(6):291–307. https://doi.org/10.5603/GP.2019.0053
Kutlesic R, Kutlesic M, Vukomanovic P, Stefanovic M, Mostic-Stanisic D (2020) Cesarean scar pregnancy successfully managed to term: when the patient is determined to keep the pregnancy. Med (Lithuan) 56(10):1–10. https://doi.org/10.3390/medicina56100496
López-Girón MC, Nieto-Calvache AJ, Quintero JC, Benavides-Calvache JP, Victoria-Borrero A, López-Tenorio J (2022) Cesarean scar pregnancy, the importance of immediate treatment. J Matern Fetal Neonat Med 35(6):1199–1202. https://doi.org/10.1080/14767058.2020.1742691
Nieto-Calvache AJ, et al. (2020) Cesarean scar pregnancy with iniencephaly and progression to placenta accreta due to early management rejection. Matern Fetal Med 2(1): 56–58. https://doi.org/10.1097/FM9.0000000000000025 (Wolters Kluwer Health)
Suzuki N et al (2020) Late-diagnosed cesarean scar pregnancy resulting in unexpected placenta accreta spectrum necessitating hysterectomy. Fukushima J Med Sci 66(3):156–159. https://doi.org/10.5387/fms.2020-14
Yang X, Zheng W, Zhang H, Wei X, Yan J, Yang H (2021) Expectant management of cesarean scar pregnancy in 13 patients. J Mater Fetal Neonat Med. https://doi.org/10.1080/14767058.2021.1940942
Fu L, Luo Y, Huang J (2022) Cesarean scar pregnancy with expectant management. J Obstet Gynaecol Res 48(7):1683–1690. https://doi.org/10.1111/jog.15258
Cali G, Forlani F, Timor-Tritsch IE, Palacios-Jaraquemada J, Minneci G, D’Antonio F (2017) Natural history of cesarean scar pregnancy on prenatal ultrasound: the crossover sign. Ultrasound Obstet Gynecol 50(1):100–104. https://doi.org/10.1002/uog.16216
Kaelin Agten A, Cali G, Monteagudo A, Oviedo J, Ramos J, Timor-Tritsch I (2017) The clinical outcome of cesarean scar pregnancies implanted on the scar versus in the niche. Am J Obstet Gynecol 216(5): 510.e1–510.e6. https://doi.org/10.1016/j.ajog.2017.01.019.
Doumouchtsis SK, Arulkumaran S (2010) The morbidly adherent placenta: an overview of management options. Acta Obstet Gynecol Scand 89(9):1126–1133. https://doi.org/10.3109/00016349.2010.503869
Nanda K, Opez LM, Grimes DA, Peloggia A, Nanda G (2012) Expectant care versus surgical treatment for miscarriage. Cochrane Database Syst Rev 3:3518. https://doi.org/10.1002/14651858.CD003518.pub3
Funding
No funds, grants, or other support was received. The authors have no financial or proprietary interests in any material discussed in this article.
Author information
Authors and Affiliations
Contributions
PVM: project development, data collection, data analysis, manuscript writing. RFB: project development, manuscript editing. CFK: data collection, manuscript editing. LRH: data collection, manuscript editing. All authors contributed to this study. RFB envisioned this review, material preparation, data collection and analysis were performed by PVM, assisted by LRH and CFK. The first manuscript was written by PVM and all authors commented, edited and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vieira de Mello, P., Bruns, R.F., Fontoura Klas, C. et al. Expectant management of viable cesarean scar pregnancies: a systematic review. Arch Gynecol Obstet 308, 701–707 (2023). https://doi.org/10.1007/s00404-022-06835-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06835-3