Abstract
Purpose
To investigate the association between different treatments of tubal ectopic pregnancy (EP) —expectant management, methotrexate (MTX), selected or recommended laparoscopic surgery—and the subsequent reproductive outcomes.
Methods
We conducted a retrospective cohort study including 228 EPs. The patients were divided into four treatment groups: 28 (12.3%) with expectant management successfully, 60 (26.3%) with MTX successfully, 140 patients with laparoscopic salpingectomy, of which 47 (20.6%) were assigned to selected surgery group because they opted for surgical treatment versus MTX, 93 (40.8%) were assigned to recommended surgery group as recommended by the attending physician.
Results
The recommended surgery group had the lowest rate of intrauterine pregnancy (IUP) (77.42%) and live birth (LB) (72.04%), while the incidence of recurrent EP (REP) (20.43%) was the highest, but the statistical differences were not significant. We did not observe significant differences of the EP-IUP time interval, rates of LB and miscarriage (MIS) between the four groups. Compared to the MTX group, recommended surgery was negatively associated with IUP (adjusted OR, 95%CI: 0.34, 0.11–1.03) and LB (0.35, 0.14–0.92), while it had higher risk for REP (3.48, 1.03–11.74) in the subsequent pregnancy. Further, compared to selective surgery group, recommended surgery was negatively associated with IUP (0.15, 0.03–0.68) and LB (0.23, 0.07–0.74), while it had higher risk for REP (6.83, 1.43–32.67) in the subsequent pregnancy. Expectant treatment was negatively associated with assisted reproductive technology (ART) (0.08, 0.02–0.40) compared with MTX. Of the185 patients who had LBs, all adverse outcomes were not statistically different between the four groups.
Conclusion
Patients with recommended laparoscopic salpingectomy had worse reproductive outcomes than the other treatment groups. The disease status of EP may play an important role in the association rather than the surgery alone.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Eligible Patients with tubal pregnancy can choose MTX treatment or laparoscopic salpingectomy for there is no significant difference between the two ways on future fertility outcome; however, for those who have undergone recommended surgery, which had lower probability of IUP/LB and higher risk of REP, we should follow up frequently and provide better reproductive capacity assessment, and use ART to conceive if necessary. |
Introduction
Ectopic pregnancy (EP) defined as a pregnancy that occurs outside of the uterus, is a major cause of maternal morbidity and mortality [1, 2]. Tubal pregnancy is the most common type of EP, accounting for 98% of cases, in which an embryo implants in the fallopian tube [3]. With the improved technology of early diagnosis of EP by serial hCG testing combined with transvaginal ultrasound scan (TVUS), the rate of emergency surgery and mortality of EP has decreased significantly [4], and now people are more concerned about the impact of EP and different treatments on future fertility.
The treatment methods of tubal EP mainly include expectant treatment, methotrexate (MTX) and laparoscopic surgery. For EPs with stable hemodynamics and unruptured mass, expectant management and MTX can be attempted. A meta-analysis showed that expectant treatment was not inferior to MTX in hemodynamically stable patients with EP that had declining or low hCG levels, for the differences in either the hCG decline or the rate of switching to surgery were both statistically insignificant [5]. If the hCG value is less than 2000 mIU/mL, the success rate of the expectant treatment can reach 88% [6]. However, for those with a high initial hCG level (especially > 5000 mIU/mL), a rapidly increasing hCG concentration (greater than 50% in 48 h), a large ectopic gestational mass (greater than 35 mm in diameter) and an EP mass with cardiac activity, laparoscopic surgery (salpingectomy, salpingostomy or ‘tubal milking’) is recommended [7, 8]. When a patient experienced signs of an ongoing ruptured ectopic mass, such as hemodynamic instability, hemoperitoneum or severe abdominal pain, emergency surgery is required [9]. In addition, some simpler and more effective detection methods are also being explored. Al Zubaidi A et al. found that the serum level of the placental growth factor (PLGF) may be a biomarker for diagnosing EP because the range of PLGF was significantly lower than that in ectopic pregnancy, but PLGF is not widely available in all clinical settings [10].
Previous studies on the effects of different treatments for tubal EP on fertility-related outcomes were inconsistent. Most studies found that there was no difference in the rate of subsequent pregnancy, the risk of recurrent EP or the average time to next conception between expectant treatment, MTX and salpingectomy [11, 12]. However, a cohort study found that the incidence of intrauterine pregnancy and live birth was higher and the time interval between treatment and first intrauterine pregnancy was shorter in the expectant management compared to surgery (p < 0.05) [13]. In these studies, the choice of different treatment modalities was often determined by serum hCG value, EP mass size and pelvic effusion. It is difficult to determine whether the observed differences are due to the treatment or the EP itself. Therefore, we conducted a retrospective cohort study and aimed to compare the effects of expectant treatment, MTX and surgery (laparoscopic salpingectomy) on fertility and adverse reproductive outcomes for women with a tubal EP.
Patients and methods
We conducted a retrospective cohort study including 903 EPs from August 2014 to July 2016 at Shanghai First Maternity and Infant Hospital in Shanghai, China. EP was diagnosed according to the following criteria: 1. the serum hCG value is positive, but showing little reduction, staying at a plateau or suboptimal rising after 48 h; 2. an ultrasound visualization of an inhomogeneous mass or a gestational sac with a yolk sac adjacent to the ovary. All enrolled patients in the study had a first tubal pregnancy. The following patients were excluded from the study: 1. those with a previous EP; 2. patients with a history of tubal surgery; 3. EPs were accompanied by IUP; 4. non-tubal EPs.
Patients with a suspected tubal EP underwent serial serum hCG testing within 24–48 h and TVUS. Asymptomatic EPs with an initial serum hCG level ≤ 2000 IU/L, showing decreasing trends, and the maximum diameter of EP mass ≤ 35 mm were managed expectantly. Laparoscopic surgery (recommended surgery) was recommended for those who met at least one of the following conditions: initial serum hCG level > 5000 IU/L, the maximum diameter of EP mass > 35 mm, tubal mass showing yolk sac, tubal mass with fetal cardiac activity, pelvic effusion depth > 30 mm, significant abdominal pain or obvious positive signs. For other hemodynamically stable women, they could choose laparoscopic surgery (selected surgery) or intramuscular MTX administration (single-dose regimen) after being fully informed of the benefits and risks of each approach. If the hCG level decreased less than 15% from days 4 to 7 after MTX administration, a second dose was given on day 7. When a patient experienced signs and symptoms of an ongoing ruptured ectopic mass (such as hemodynamic instability, hemoperitoneum or severe abdominal pain), the hCG did not decrease after two doses of MTX, or if they developed severe adverse effects, those indicated failure of MTX treatment and surgery was recommended. Such patients who failed MTX treatment and were converted to surgery were not included in the study. Laparoscopic surgery included salpingectomy, salpingostomy and tubal milking. Salpingectomy is the most common modality in our hospital, while a small number of patients choose salpingostomy or tubal milking for preserving the fallopian tube. In this study, only laparoscopic unilateral salpingectomy was included, and other procedures (salpingotomy, tubal milking, bilateral salpingectomy) were excluded. In addition, other combinations of treatments were also excluded, such as MTX or surgery combined with traditional Chinese medicine or mifepristone. All patients required close follow-up of serum hCG levels until negative. The patients’ characteristics (maternal age, precedent pelvic surgery, miscarriage, parity, infertility) and the information of EP (including clinical symptom, serum hCG level and ultrasound image) were obtained through the electronic health records (EHR) of the hospital.
Effective contraception for at least 3 months was recommended for all patients after the serum hCG level normalized. We followed all the patients by phone for their first subsequent pregnancy within 5 years after the treatment. Specifically, this includes the reproductive outcomes (IUP, LB, preterm, MIS, EP), whether or not to conceive with ART and the pregnancy interval time. Those who were unmarried, who used contraception without desire for reproduction, who could not be reached by phone, or who refuse to enroll were excluded from the study. For those with an IUP, several adverse birth outcomes were examined, including gestational diabetes mellitus (GDM), preeclampsia, premature rupture of membrane (PROM), hypothyroidism, multiple birth, abnormal fetal position (such as breech presentation), fetal growth restriction (FGR), placenta previa, oligohydramnios, isolated proteinuria and cesarean delivery.
Statistical analysis
Continuous variables were reported as the mean ± standard deviation (SD) when they met normal distribution, otherwise, the median and range were reported. The Kolmogorov–Smirnov test was applied to determine the normal distribution. One-way analysis of variance (ANOVA) and post hoc analysis were applied to compare the difference between the four groups for normally distributed variables. Categorical variables were reported as the absolute number and percentage (%). The Kruskal–Wallis test by rank was used to compare nonparametric continuous and ordinal variables, with post hoc analysis if required. Chi-squared tests were used to compare qualitative data, and Fisher’s exact test was applied when the expected frequency was less than five and p < 0.05 was considered significant, which was adapted using the Bonferroni method in case of multiple comparisons.
Multivariable logistic regression models were applied to explore the association of treatments and IUP, LB, REP and ART respectively. For the factors, including maternal age, precedent pelvic surgery, parity, miscarriage, infertility, and ART have been previously reported have clinical significance for reproductive outcomes [14, 15], they were all adjusted in the multivariable regression models (expect the ART model), regardless of statistical significance. The estimated adjusted odds ratios (ORs) with 95% CIs were presented on forest plot. Data management and analysis were performed using SAS statistical analysis software, version 9.4 (SAS Institute, Inc), and forest plot figure were constructed using R statistical software, version 4.1.2 (R Project for Statistical Computing).
Results
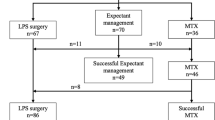
As shown in Fig. 1, there were totally 903 EPs. 675 were excluded from the study and the final number of eligible participants was 228. Overall, 28 out of 228 (12.3%) were successfully treated with expectant management, 60 (26.3%) was successfully administered with MTX. A total of 140 (61.4%) women underwent laparoscopic salpingectomy, of whom 47 were in the selected surgery group and 93 in the recommended surgery group.
As shown in Table 1, there were no statistically significant differences between the four groups in terms of maternal age, precedent pelvic surgery, miscarriage, parity and infertility. Vaginal bleeding was the most common clinical symptom, accounting for the highest proportion of 96.43% in the expectant treatment group. Nineteen (20.43%) patients with severe abdominal pain and sixteen (17.2%) patients with obvious positive signs underwent surgery in the recommended surgery group. The average hCG level in the recommended surgery group was 8953.17 ± 13,219.04 mIU/ml, significantly higher than the other three groups. The average hCG level in the selected surgery group was 2192.04 ± 1452.26 mIU/ml, which was higher than 579.62 ± 855.43 mIU/ml in the expectant group and 588.06 ± 557.12 mIU/ml in the MTX group, but the differences were not statistically significant. The max diameter of EP mass in the recommended surgery was 33.67 ± 12.50 mm, significantly bigger than 21.29 ± 7.02 mm in the expectant group, 22.45 ± 6.94 mm in the MTX treatment and 22.09 ± 8.59 mm in the selected surgery. The depth of pelvic effusion in the recommended surgery (25.70 ± 12.01 mm) was the highest in the four groups, 16.19 ± 8.67 mm in the selected surgery was also higher than that in the expectant management (10.21 ± 10.01 mm) and the MTX treatment (11.27 ± 8.52 mm) with significant statistically difference.
We followed up the first reproductive outcomes in the four treatment groups during the following 5 years (Table 2). There was no significant statistically difference in the EP-IUP time interval in the four groups. In the expectant group, only 2 women (7.14%) underwent ART, which was significantly lower than that in the MTX treatment (38.98%), the selected surgery (34.78%) and the recommended surgery (40.22%) (p = 0.011). In the four groups, the recommended surgery had the lowest rate of IUP (77.42%) and LB (72.04%), while the incidence of REP (20.43%) was the highest, but the differences were not statistically significant. There were no statistical differences in the rates of preterm birth and MIS between the four groups.
The associations between EP administrations and reproductive outcomes (IUP, LB, REP, ART) were estimated by multivariable logistic regression models, adjusting for maternal age, precedent pelvic surgery, miscarriage, parity, infertility and ART (expect in the ART models). As shown in Fig. 2, compared to the MTX group, recommended surgery was negatively associated with IUP (adjusted OR, 95%CI: 0.34, 0.11–1.03, p = 0.057) and live birth (0.35, 0.14–0.92, p = 0.033), while it was positively correlated with REP (3.48, 1.03–11.74, p = 0.045) in the subsequent pregnancy, although the association between recommended surgery and IUP was borderline significant (p = 0.057). Further, compared to selected surgery group, recommended surgery was negatively associated with IUP (0.15, 0.03–0.68, p = 0.014) and live birth (0.23, 0.07–0.74, p = 0.013), while it was positively correlated with REP (6.83, 1.43–32.67, p = 0.016) in the subsequent pregnancy, and all the correlations was statistically significant. Expectant was negatively associated with ART (0.08, 0.02–0.40, p = 0.002) compared with MTX group. We didn’t observe statistically significant correlations between other treatment groups and ART.
The associations between tubal EP administrations and reproductive outcomes. The covariates including maternal age, precedent pelvic surgery, miscarriage, parity, infertility and ART were adjusted in the logistic regression models for IUP, LB, REP. The covariates including maternal age, precedent pelvic surgery, miscarriage, parity and infertility were adjusted in the logistic regression models for ART. (OR odds ratio; CI confidence interval)
The overall adverse reproductive outcomes of subsequent LB in patients with tubal EP were ranked in proportion from highest to lowest in Table 3. Of the185 patients who had LB, 94 (50.81%) underwent cesarean delivery. The next top 5 adverse outcomes were GDM (18.38%), PROM (17.84%), twin pregnancy (9.73%), preeclampsia (9.19%) and hypothyroidism (5.95%). However, all adverse reproductive outcomes were not statistically different between the four treatment groups.
Discussion
In this retrospective cohort study of 228 first tubal EPs who had fertility desire, we found that the recommended surgery group had the lowest rate of IUP and LB, while the incidence of REP was the highest, compared to expectant treatment, MTX and selective surgery group. There were no significant differences in the EP-IUP time interval, rates of LB and MIS (Table 2), and adverse reproductive outcomes of subsequent LBs between the four treatment groups (Table 3).
Interpretation in light of previous literature
Most previous research on the fertility outcomes of women with a tubal EP had focused on the IUP and REP rates with different treatment modalities. A considerable number of studies suggest that the IUP rates of women with tubal EPs were similar after expectant treatment (30.8–83.7%), MTX (63.6– 79%), and surgery (51.4–65.2%) [12, 16,17,18]. However, Baggio S et al. found that expectant management had higher rate of IUP and LB, and shorter time interval of EP-IUP compared to surgery (p < 0.05), the rate of REP was comparable between expectant treatment, MTX and surgery. To exclude the influence of hCG and EP mass diameter on the results, they further repeated the analysis by restricting EP mass less than 25 mm and got consistent results, but when restricted hCG less than 1745 mUI/mL, there were no differences in IUP, LB and REP [13]. However, their study could not completely exclude the effect of hCG and EP mass on reproductive outcomes, as the high value of hCG and EP mass was not studied. In our study, patients with EP were grouped according to different treatments. The surgery group was divided into selected surgery and recommended surgery groups according to the patients' symptom and sign, serum hCG level and ultrasound image. There were no significant differences in patients’ basic characteristics, hCG value and the maximum size of EP in the expectant group, MTX and selected surgery group (Table 1). We found that the EP-IUP time interval in the four groups was comparable, and ART was widely used in the MTX and surgery group. The rates of IUP (p = 0.031), LB (p = 0.034) and REP (p = 0.017) were statistically different between the four groups. The recommended surgery had the lowest rate of IUP (77.42%) and LB (72.04%) and the highest rate of REP (20.43%) (Table 2). We further conducted a multivariable logistic regression analysis by controlling the possible confounders of maternal age, precedent pelvic surgery, miscarriage, parity, infertility and ART, and the results showed that compared to the MTX or selected surgery treatments, recommended surgery increased the risk of REP and reduced the probability of IUP and LB (Fig. 2). The obvious advantages of MTX and selected surgery compared to recommended surgery remind us that the active and effective management in the early stage of EP who are hemodynamically stable is essential to optimize the subsequent reproductive outcomes.
There were few studies on the relationship between EP and the adverse reproductive outcomes of subsequent LB. Chouinard et al. found that women with surgically treated first EPs had an increased risk of adverse reproductive outcomes at future first IUP than those without EP, including 1.45 times the risk of placenta previa, 1.27 times the risk of preterm birth, 1.25 times the risk of gestational diabetes, 1.20 times the risk of low birth weight, 1.17 times the risk of cesarean delivery, and 1.11 times the risk of oligohydramnios [14]. Roitman MS et al. found that a history of EP was significantly associated with adverse outcomes in future IUP, such as placental abruption, preterm delivery, and cesarean delivery. Additionally, the incidence of hypertensive disorders and diabetes mellitus was higher than women with no history of EP. They also found that both surgically and medically treated ectopic pregnancies were noted as independent risk factors for preterm delivery in the subsequent pregnancies [19]. These studies were all about the adverse outcomes of future LB in patients with a history of EP versus those without EP, but lack studies between different treatments for EP. We studied the fertility differences in women with EP treated with expectant management, MTX, and laparoscopic salpingectomy. We found that there were no statistical differences in the rate of preterm birth as well as other adverse reproductive outcomes between the four groups (Table 3).
Strength and limitation of the study
The biggest strength of our research was the high accuracy of the data. Shanghai First Maternity and Infant Hospital is one of the largest obstetrics and gynecology hospitals in Shanghai, which serves approximately 20% pregnant women and has an annual delivery volume of about 25,000–30,000. A considerable number of patients with EP will choose to have obstetric examination and delivery in our hospital after re-pregnancy. In the study, data of patients, including the reproductive outcomes and adverse outcomes were mainly obtained through EHR of the hospital (87%), and a small number were obtained through telephone follow-up (13%).
However, insufficient sample size was the main limitation in our study. First, about one in five of the 903 EPs recorded in the EHR in our hospital from August 2014 to July 2016 lost contacts. This may be related to the high mobility of Shanghai's population. Second, we did not find the relative advantage of the expectant treatment in our study, which may be due to the small sample size of the expectant group for a substantial number of patients who were hemodynamically stable and who had low hCG level were followed up in outpatient clinics. Finally, the limitation of small sample size was particularly evident in the part of adverse reproductive outcomes of re-LB. In future, prospective cohort study with large sample size should be conducted to obtain better experimental results.
Conclusion
Despite the same surgery (laparoscopic salpingectomy) performed, compared with the MTX group, only the recommended surgery group had lower probability of IUP and LB during the follow-up, and higher risk of REP. Besides, the rates of IUP, LB and REP differed significantly between the selected surgery and the recommended surgery. These results suggested that the disease status may play an important role in the reproductive outcomes of EP, rather than the surgery alone. Therefore, for the patients of EP who have undergone recommended surgery and need to reproduce again, we should follow up frequently and provide better reproductive capacity assessment, and use ART to conceive if necessary.
References
Creanga AA, Syverson C, Seed KCallaghan WM. (2017) Pregnancy-related mortality in the United States 2011–2013. Obstet Gynecol 130:366–373
Wang E, Glazer KB, Howell EAJanevic TM. (2020) Social determinants of pregnancy-related mortality and morbidity in the united states: a systematic review. Obstet Gynecol 135:896–915
Bouyer J, Coste J, Fernandez H, Pouly JLJob-Spira N. (2002) Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod 17:3224–3230
Abusheikha N, Salha OBrinsden P, (2000) Extra-uterine pregnancy following assisted conception treatment. Hum Reprod Update 6:80–92
Naveed AK, Anjum MU, Hassan AMahmood SN. (2021) Methotrexate versus expectant management in ectopic pregnancy: a meta-analysis. Arch Gynecol Obstet 305(3):547–543
Korhonen J, Stenman UHYlostalo P. (1994) Serum human chorionic gonadotropin dynamics during spontaneous resolution of ectopic pregnancy. Fertil Steril 61:632–636
Menon S, Colins JBarnhart KT. (2007) Establishing a human chorionic gonadotropin cutoff to guide methotrexate treatment of ectopic pregnancy: a systematic review. Fertil Steril 87:481–484
Cohen A, Zakar L, Gil Y, Amer-Alshiek J, Bibi G et al (2014) Methotrexate success rates in progressing ectopic pregnancies: a reappraisal. Am J Obstet Gynecol 211(128):e1-5
Committee on Practice B-G (2018) ACOG practice bulletin no 191: tubal ectopic pregnancy. Obstet Gynecol 131:e65–e77
Zubaidi Al, AEid MM. (2021) The diagnostic utility of placental growth factor in ectopic pregnancy. Arch Gynecol Obstet 304:833–838
Park EHG, Mohammadi-Zaniani G, Pronin S, Elderfield CHJDuncan WC. (2017) Subsequent pregnancy outcome of tubal ectopic pregnancies treated by methotrexate and salpingectomy. Eur J Obstet Gynecol Reprod Biol 212:192–193
Helmy S, Sawyer E, Ofili-Yebovi D, Yazbek J, Ben Nagi J et al (2007) Fertility outcomes following expectant management of tubal ectopic pregnancy. Ultrasound Obstet Gynecol 30:988–993
Baggio S, Garzon S, Russo A, Ianniciello CQ, Santi L et al (2021) Fertility and reproductive outcome after tubal ectopic pregnancy: comparison among methotrexate, surgery and expectant management. Arch Gynecol Obstet 303:259–268
Chouinard M, Mayrand MH, Ayoub A, Healy-Profitos JAuger N. (2019) Ectopic pregnancy and outcomes of future intrauterine pregnancy. Fertil Steril 112:112–119
Bhattacharya S, Townend J, Shetty A, Campbell DBhattacharya S. (2008) Does miscarriage in an initial pregnancy lead to adverse obstetric and perinatal outcomes in the next continuing pregnancy? BJOG 115:1623–1629
Olofsson JI, Poromaa IS, Ottander U, Kjellberg LDamber MG. (2001) Clinical and pregnancy outcome following ectopic pregnancy; a prospective study comparing expectancy, surgery and systemic methotrexate treatment. Acta Obstet Gynecol Scand 80:744–749
Li J, Jiang KZhao F. (2015) Fertility outcome analysis after surgical management of tubal ectopic pregnancy: a retrospective cohort study. BMJ Open 5:e007339
Turan V (2011) Fertility outcomes subsequent to treatment of tubal ectopic pregnancy in younger Turkish women. J Pediatr Adolesc Gynecol 24:251–255
Roitman MS, Wainstock T, Sheiner E, Leibson TPariente G. (2021) Ectopic pregnancy: perinatal outcomes of future gestations and long-term neurological morbidity of the offspring. Arch Gynecol Obstet 304:633–640
Funding
This work was supported by [The National Natural Science Foundation of China] (Grant numbers [81971338] and [81971338], Wen Lu).
Author information
Authors and Affiliations
Contributions
YS Data collection, Data analysis, Manuscript writing and editing, Forming Table 1/2/3 and Fig. 1, Manuscript revision. YY Data analysis, Statistical analysis, Forming Fig. 2, Manuscript revision. PZ Data collection. LH Data collection. RC Data collection. ZL Statistical analysis, Manuscript revision. WL Project development, Manuscript revision.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the Ethics Committee, Shanghai First Maternity and Infant Hospital, No. KS21336.
Consent to publications
All authors consent to the publication of this manuscript.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, Yt., Yang, Yy., Zhang, Pg. et al. Tubal ectopic pregnancy: a retrospective cohort study on clinical characteristics, treatment options and reproductive outcomes within 5 years. Arch Gynecol Obstet 306, 2055–2062 (2022). https://doi.org/10.1007/s00404-022-06690-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06690-2