Abstract
Purpose
There is little information on the use of extracorporeal membrane oxygenation (ECMO) in pregnant women. Our objectives are to estimate the use of ECMO in pregnant patients, identify clinical conditions associated with ECMO use, and assess survival rates by the associated condition.
Methods
Using the Healthcare Cost and Utilization Project–Nationwide Inpatient Sample, we carried out a retrospective cohort study of all delivery admissions in the United States from January 1, 1999, to October 1, 2015. Within the cohort, women who received ECMO therapy were identified using ICD-9 codes and then survival rates among these women were calculated.
Results
There were 83 women who underwent ECMO therapy in our cohort of 15,335,205 births, for an overall ECMO use rate of 0.54/100,000 pregnancies. The incidence of ECMO use increased from 0.23/100,000 in 1999 to 2.57/100,000 in 2015. Patients on ECMO were more likely to be older, have a lower income, and have pre-existing medical conditions when compared with the patients not on ECMO. The overall survival rate for the ECMO group was 62.7%. The most common reason for ECMO use was acute respiratory failure. Etiologies associated with the highest survival in those on ECMO were pneumonia and venous thromboembolism, which were found to have survival rates of 75.0% and 81.0%, respectively.
Conclusion
The incidence of ECMO use in the obstetric population increased over the last decade and a half. Although it carries a limited survival rate within this population, it has proven life-saving for many suffering from complications of pregnancy and delivery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extracorporeal membrane oxygenation (ECMO) is an invasive technique of providing cardiac and/or pulmonary support extracorporeally for patients whose heart and/or lungs cannot adequately provide oxygenation or perfusion to sustain life. ECMO systems are most commonly found in hospital intensive care units (ICU), as typical patients requiring ECMO suffer from respiratory or cardiac failure [1]. Although ECMO use has risen in the general population over the past few decades [2], the extent of its use and benefit in pregnant patients is still unknown. Many of the rare complications of pregnancy and delivery can lead to cardiac or pulmonary failure in the patient [3]. The Centers for Disease Control and Prevention (CDC) recently stated 700 women in the United States die every year from pregnancy-related causes [4], and the Maternal Mortality Review Information Application (MMRIA) reported that 14% of maternal deaths are due to cardiovascular and coronary conditions, alone [5]. The current literature of ECMO use in the pregnant or peripartum patient consists mainly of case reports and a few case series. A limited review of this literature showed favorable survival rates of pregnant women placed on ECMO, such as 80% for the mother, and 70% for the fetus [6]. Only one cohort study was found, which focused on peripartum patients and ECMO at a single tertiary institution and stated a maternal survival rate of 33% [7]. The paucity of observational analytical studies examining the use of ECMO in obstetrical patients, in conjunction with the observed greater use of ECMO in the parturient, indicates an urgent need for a large population-based cohort study. The objectives of this study are to estimate the rate of ECMO usage in pregnant patients and assess associated survival rates in such patients, as well as investigate clinical conditions in which ECMO was indicated.
Materials and methods
Data source
We used the Healthcare Cost and Utilization Project (HCUP) database to address our study objectives. HCUP is a family of healthcare databases, encompassing the largest amount of inpatient hospital admission data in the United States. The volume of data available allows for the identification and analysis of trends across the nation [8]. The information from HCUP follows proper confidentiality protocols per the Health Insurance Portability and Accountability Act (HIPAA) privacy rule. The National Inpatient Sample (NIS) is a subset database composed of virtually 20% of all hospital admissions in US community hospitals, regardless of payer, excluding rehabilitation and long-term care institutions [9]. New data is publicly released annually for up-to-date research. Their Clinical Classification Software (CCS) is based on the uniform and standardized International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) coding system.
Study population
Using the HCUP database, a cohort was created comprised of pregnant or peripartum patients from 1999 to October 1st, 2015, exclusively. The data of 230,487,673 patient discharges were collected by the NIS between 1999 and December 31, 2015. This dataset was then truncated as of October 1, 2015 as the NIS switched their coding system from ICD-9-CM to ICD-10-CM on this date, resulting in the exclusion of 1,744,617 patients. Of the remaining 228,713,056 discharges, 53,577,365 male patients were excluded and then the ICD-9 codes for pregnancy and delivery (diagnosis codes V22.xx, V23.xx, V27.xx, 634.xx-679.xx, and procedure codes 72xx-75.xx) and maternal deaths (761.6, NIS Died During Hospitalization) were used to create a cohort of 15,335,288 pregnant patients. The ICD-9 code for ECMO (39.65) was subsequently used, creating two distinct groups: 83 pregnant patients who were treated with ECMO, and 15,335,205 pregnant patients who were not treated with ECMO. This code is in concordance with similar studies that focused on the use of ECMO in different patient populations, such as a study on ECMO use in the pediatric population by Bokman et al. [10], or the study by Wallace et al. regarding geographical access to life-supporting machines within the United States [11].
Statistical analysis
First, the annual incidence of ECMO use was calculated within the number of annual births, and trends were inspected over the study period. Next, the baseline characteristics of women requiring ECMO use or not were identified and the frequency of these characteristics was summarized. These variables included maternal age, race, insurance type, hospital type, household median income quartile, history of previous cesarean section, smoking status, and pre-existing medical conditions. Then, the indications for ECMO use were identified using ICD-9-CM codes as follows: heart failure (code 428x), cardiac arrest (427.5), cardiogenic shock (785.51), peripartum cardiomyopathy (674.5x), pneumonia (480x–487x), acute respiratory failure (518.81, 518.82, 799.1), disseminated intravascular coagulation (DIC) (286.6), venous thromboembolism (VTE) (415.1, 453.4, 671.3, 671.4, 673.2, V12.51), sepsis (995.91, 991.92), septic shock (785.52), other infectious conditions (030x–041x), and acute renal failure (584.9, 639.3, 669.3). Survival rates and corresponding 95% confidence intervals were calculated to determine the influence of ECMO use on survival overall by associated diagnosis. Per the 2010 Tri-Council Policy statement, the institutional review board was not necessary, as this study used only de-identified publicly available data. All analyses were carried out using the statistical software package SAS Enterprise Guide 6.1 (Cary, NC, USA).
Results
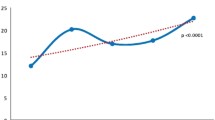
The overall incidence of ECMO use in pregnant patients during the study period was 0.54 per 100,000 deliveries. The incidence of ECMO use in pregnant patients per year between 1999 and 2015 is shown in Fig. 1. Since the dataset used was truncated as of October 1, 2015, we extrapolated the data until December 31 to represent a relevant trend. The incidence increased from 0.23 patients per 100,000 in 1999, to 2.57 patients per 100,000 in 2015, p < 0.0001.
Table 1 lists the baseline demographic characteristics of the patients by ECMO status. The patients in the ECMO group were more likely to be older, with 27.7% being 35 years or older, as compared with 14.5% in the non-ECMO group. Some minor racial disparities were seen, with Black women being more likely to require ECMO. The ECMO patients tended to have a lower income, to be on Medicare, and over 95% of them were treated in urban teaching hospitals. Another notable distinction is that patients on ECMO were more likely to have pre-existing conditions, such as lung disease, rheumatic disease, immunologic conditions, and hematologic conditions.
Diagnoses leading to the necessity of ECMO use in pregnant patients are listed in Table 2. Notably, acute respiratory failure (62.7%), pneumonia (43.4%), sepsis (53.0%), and other infectious conditions (55.4%), excluding septic shock, were the most common conditions leading to the ECMO use in our patient population. The survival rates for each associated diagnosis and their respective 95% confidence intervals are graphically displayed in Fig. 2. The survival rates for the disorders listed above were 61.5% (95% Confidence Interval [95% CI] 48.3–74.3%), 75.0% (95% CI 60.9–89.1%), 65.9% (95% CI 51.9–79.9%), and 67.4% (95% CI 53.9–81.0%), respectively. The diagnoses with the lowest survival rates were cardiac arrest (56.3%, 95% CI 32.0–80.6%), peripartum cardiomyopathy (54.2%, 95% CI 34.2–74.1%), disseminated intravascular coagulation (47.1%, 95% CI 23.4–70.8%), and acute renal failure (57.1%, 95% CI 40.7–73.5%).
Discussion
The purpose of this study was to evaluate the use of ECMO in the pregnant population. Specifically, our objectives were to investigate the temporal changes in ECMO use in obstetrical patients, to enumerate the diagnoses resulting in the placement of pregnant patients on ECMO, and to analyze the survival rates of patients on ECMO by diagnostic condition. A cohort of deliveries was created using the HCUP-NIS database, which was then subdivided into two groups: those treated with ECMO and those not treated with ECMO. Eighty-three patients were treated with ECMO during pregnancy or in the peripartum period, with acute respiratory failure being the most common reason for placement on ECMO. The overall survival rate among pregnant women requiring ECMO was 62.7%.
In our study, the overall incidence of ECMO use was 0.54 per 100,000 deliveries over the study period. Although the use of ECMO appeared to be uncommon until about 2006, in the ensuing years we observed a pronounced increase in the use of ECMO within the obstetric population. Its use rose more than 11-fold between 1999 and 2015. A similar temporal trend in ECMO use was noted by the Extracorporeal Life Support Organization (ELSO) in their annual International Summary [2]. In this summary, they plotted the frequency of ECMO use over time in the general population. This resulted in a similar curve, showing a steady rise in the use of ECMO over a larger timespan, from 1990 to 2017. The overall number of cases however, only increased by about 4.5 times, from 1644 cases in 1990 to 9330 cases in 2017 [2]. A 2015 study by Sauer et al. declared a 433% increase in ECMO utilization in the US adult population from 2006 to 2011, with a trend toward improved survival rates and unchanged hospital costs [12].
When compared to the pregnant patients who did not receive ECMO therapy, those requiring ECMO tended to be older, had a lower income, were treated in urban teaching hospitals, and had higher rates of pre-existing medical conditions, such as lung disease, rheumatic disease, immunologic conditions, or hematologic disorders. As in similar studies, such as Elbadawi et al. and the previously mentioned study by Wallace et al., urban teaching hospitals have the equipment and expertise to place a patient on ECMO [11, 13]. This is in concordance with our study, which showed 95.2% of ECMO patients being treated in urban teaching hospitals.
Survival within our cohort was generally favorable with an overall survival rate of 62.7%, representing 52 out of 83 patients. There is a wide range of survival rates within the literature that has examined ECMO use among obstetrical patients, which has essentially consisted solely of case reports and case series. For instance, the largest case series to date on this procedure within the pregnant and postpartum population was conducted by Agerstrand et al. This study analyzed a single hospital’s ICU admissions from 2009 to 2015. In all, 18 patients were identified and compared. The overall survival rate in this study was 88.9%, significantly higher than our study’s survival rate [14]. We hypothesize that the discrepancy between survival rates is caused by a significant difference in sample size between studies. A cohort study from Aubron et al. focused on ECMO use at one of the largest ICUs in Australia. Their patient population, consisting of 151 patients, represented all adult men and non-pregnant women over the age of 16 who underwent ECMO therapy. Based on the overall mortality rate presented in the study, we calculated a survival rate of 62.7%, equal to the survival rate in our study [15]. In the aforementioned study, ELSO’s International Summary includes cumulative survival rates from 1990 to 2017, inclusively [2]. Within the adult population, the overall survival rate was 47.8%, which is much lower than the rate found in our cohort. We surmise that the 15% difference in survival rates may be due to a larger proportion of older patients within ELSO’s adult cohort. Although patients placed on ECMO are evidently very sick, in general, geriatric patients would likely have more comorbid illnesses than the younger population and thus, the survival rate would be lower in a sample from the general population. In contrast, women of reproductive age, like in our study, tend to be healthier with less co-morbidity, placing them at a greater likelihood of survival.
Within our patient population, the most common indications for ECMO use were acute respiratory failure, sepsis, pneumonia, and other infectious conditions, with over half of the patients diagnosed with one or more of these conditions. Survival rates in these patients were somewhat favorable and ranged from 61.5 to 75.0%. Pneumonia and venous thromboembolism were associated with the most favorable outcomes, with survival rates of 75.0% and 81.0%, respectively. It is likely that the often-reversible nature of infectious conditions, given proper antibiotics and supportive therapy, is what leads to favorable results in patients with pneumonia, sepsis, septic shock or other infectious conditions. Overall survival in all the associated diagnoses was over 50% throughout, with the exception of disseminated intravascular coagulation, which showed a slightly lower survival rate of 47.1%.
Pregnancy causes changes in hemodynamics, such as volume overload and cardiovascular changes [16], which may lead to detrimental maternal and fetal outcomes. Due to the youthful and typically healthier baseline status of the obstetric population when compared to the general population, ECMO may be useful to provide temporary cardiac and respiratory support while reversible conditions, such as peripartum cardiomyopathy, are managed. With well-trained and experienced staff, the risk of adverse events can be controlled, thus allowing for predominantly favorable outcomes.
Based on the favorable outcomes of our study, we recommend the development of a comprehensive registry. This registry could facilitate future research and be a consulting resource for physicians when deciding if their patients could benefit from ECMO.
Our study had several limitations. First, our study was retrospective based on an existing dataset; hence, some variables of interest were not available. For example, we did not have information on the gestational age at which patients were put on ECMO therapy, whether they were treated before or after delivery, or the long-term maternal outcomes. Similarly, the duration of therapy, neonatal survival and outcomes were not available. On the other hand, this study had several strengths. It is the first major population-based cohort study on ECMO use in the pregnant and peripartum population. To our knowledge, it is also the largest study on this rare obstetrical intervention with the longest timeline to date, spanning 16 years of data, allowing for the analysis of temporal trends. Further, the findings of our study are generalizable to the larger North American obstetrical population. As previously mentioned, our study used the ICD-9 code 39.65 to identify the subset of patients who received ECMO therapy. This is in agreement with similar studies conducted on different patient populations, such as aforementioned Bokman et al. [10] and Wallace et al. [11]
Conclusion
ECMO use in the obstetric population is on the rise in the United States and we anticipate the use of this therapy to continue to increase within this population over the coming years. The favorable findings were seen in our study open the doors to a new intervention for fatal complications of pregnancy. Due to the youthful and, in general, healthier baseline status of the obstetric population, ECMO is a valid option for the recovery of severe maternal complications.
References
ELSO Guidelines for Cardiopulmonary Extracorporeal Life Support (2013) Extracorporeal Life Support Organization. Ann Arbor, MI, USA. www.elsonet.org. Accessed 20 Nov 2019
ECLS Registry Report: International Summary (2018) Extracorporeal Life Support Organization. Ann Arbor, MI, USA. https://www.elso.org/Registry/Statistics/InternationalSummary.aspx. Accessed 20 Nov 2019
Clardy PF, Reardon CC (2018) Critical illness during pregnancy and the peripartum period. Available from: https://www.uptodate.com/contents/critical-illness-during-pregnancy-and-the-peripartum-period. Accessed 20 Nov 2019
Pregnancy-Related Deaths (2018) Centers for disease control and prevention. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-relatedmortality.htm. Accessed 25 Jan 2019
Building U.S. Capacity to Review and Prevent Maternal Deaths (2018). Report from nine maternal mortality review committees. https://reviewtoaction.org/Report_from_Nine_MMRCs. Accessed 25 Jan 2019.
Sharma NS, Wille KM, Bellot SC, Diaz-Guzman E (2015) Modern use of extracorporeal life support in pregnancy and postpartum. ASAIO J 61:110–114 (American Society for Artificial Internal Organs : 1992)
Webster CM, Manuck T (2019) 836: Extracorporeal membrane oxygenation in pregnant and postpartum women: a ten-year cohort. Am J Obstet Gynecol 220:S545–S546
HCUP Databases Rockland, MD.: Agency for healthcare research and quality; 2006–2009. Available from: https://www.hcup-us.ahrq.gov/databases.jsp. Accessed 20 Nov 2019
HCUP National Inpatient Sample (NIS) (2012) Healthcare Cost and Utilization Project (HCUP). www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 20 Nov 2019
Bokman CL, Tashiro J, Perez EA, Lasko DS, Sola JE (2015) Determinants of survival and resource utilization for pediatric extracorporeal membrane oxygenation in the United States 1997–2009. J Pediatric Surg 50:809–814
Wallace DJ, Angus DC, Seymour CW, Yealy DM, Carr BG, Kurland K et al (2014) Geographic access to high capability severe acute respiratory failure centers in the United States. PLoS ONE 9:e94057
Sauer CM, Yuh DD, Bonde P (2015) Extracorporeal membrane oxygenation use has increased by 433% in adults in the United States from 2006 to 2011. ASAIO J 61:31–36 (American Society for Artificial Internal Organs : 1992)
Elbadawi A, Mentias A, Elgendy IY, Mohamed AH, Syed MH, Ogunbayo GO et al (2019) National trends and outcomes for extra-corporeal membrane oxygenation use in high-risk pulmonary embolism. Vascr Med (London, England) 24:230–233
Agerstrand C, Abrams D, Biscotti M, Moroz L, Rosenzweig EB, D'Alton M et al (2016) Extracorporeal membrane oxygenation for cardiopulmonary failure during pregnancy and postpartum. Ann Thoracic Surg 102:774–779
Aubron C, Cheng AC, Pilcher D, Leong T, Magrin G, Cooper DJ et al (2013) Factors associated with outcomes of patients on extracorporeal membrane oxygenation support: a 5-year cohort study. Crit Care (London, England) 17:R73
Maternal adaptations to pregnancy (2017) Cardiovascular and hemodynamic changes. Available from: https://www.uptodate.com/contents/maternal-adaptations-to-pregnancy-cardiovascular-and-hemodynamic-changes. Accessed 20 Nov 2019
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
NS: contributed to study design; interpretation of data; drafting of the manuscript; read and approved the final version of the manuscript. NC-S: data management; formal data analysis; revision of the manuscript; read and approved the final version of the manuscript. AS: contributed to study design; interpretation of data; revising of original manuscript; read and approved the final version of the manuscript. HA: conception and design; acquisition of data; supervision of analyses; interpretation of data; critical revision of the manuscript for important intellectual content; read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest. We had full control of all primary data and we agree to allow the Journal to review this data if requested.
Research involving human participants
This study exclusively used data from an existing administrative database. This data was publicly available; hence, according to the Tri-Council Policy statement (2010), institutional review board approval was not required.
Informed consent
This study used publicly available data; hence, we did not personally obtain informed consent from study subjects. This would be the responsibility of the Agency for Healthcare Research and Quality (AHRQ), who sponsors the National Inpatient Sample.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sebastian, N., Czuzoj-Shulman, N., Spence, A.R. et al. Use of extracorporeal membrane oxygenation in obstetric patients: a retrospective cohort study. Arch Gynecol Obstet 301, 1377–1382 (2020). https://doi.org/10.1007/s00404-020-05530-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05530-5