Abstract
Purpose
To explore the value of high-frequency two-dimensional (2D) ultrasound on demonstrating the morphology of puborectalis muscle and detect muscle avulsion.
Methods
High-frequency 2D ultrasound and tomographic ultrasound image (TUI) were peformed to demonstrate puborectalis muscle and detect muscle avulsion respectively among 158 women with or without significant pelvic organ prolapse (POP) (POP quantification grade 2 or higher). Mean values were compared using student’s t test between women with or without avulsion defects. We performed Cohen’s Kappa analysis to examine the test agreement between high-frequency 2D ultrasound and TUI mode. Pearson correlation analysis was performed to explore the relationship between the thickness of puborectalis muscle and the measurements of levator–urethra gap (LUG).
Results
The result of high-frequency 2D ultrasound in detecting muscle avulsion agreed well with TUI mode (Kappa 0.88, P < 0.05). Women with muscle avulsion had thinner muscles and larger LUG measurements than those with normal muscle insertion (P < 0.05). Pearson correlation analysis revealed the negative relationship between the thickness of puborectalis muscle and LUG measurements (r = − 0.73).
Conclusion
The study confirmed that it was feasible to observe the morphology of puborectalis muscle and detect muscle avulsion by high-frequency 2D ultrasound.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pelvic floor dysfunction (PFD) is a common condition among women, especially in aged women over 50 years or young postpartum women with prolonged second stage of labor in vaginal delivery. The mechanism is not fully understood; parity, delivery mode, growing age and inherent weakness are all high-risk factors [1]. The pelvic floor is a complex structure composed of organs, bones, muscles, fascia, ligaments and other supportive tissues. The levator ani muscles, especially puborectalis muscle, play an important role in maintenance of the integrity of pelvic floor and the normal morphology of levator hiatus. Once the muscles are defected, the pelvic organs will drop in position or even prolapse and the area of levator hiatus will increase abnormally [2, 3]. Muscle avulsion may also be an important indicator of pelvic organ prolapse recurrence [4], so detecting muscle avulsion timely and effectively may be of great value for prolapse management.
Three-dimensional (3D) ultrasound, magnetic resonance imaging (MRI) and clinical palpation have been broadly applied in the diagnosis of muscle avulsion [5,6,7]. MRI can provide a multiplanar view of levator ani muscles with its high-resolution and thin-layer scanning technology and has been taken as the standard in the diagnosis of muscle avulsion. Tomographic ultrasound image (TUI), a special mode of 3D ultrasound, is becoming more and more popular in recent years for its ease of use, multiplanar imaging capacity, and excellent temporal resolution. TUI mode is used to measure the levator-urethra gap (LUG) for detecting muscle defects in common, both for Caucasians and Chinese [8,9,10]. Numerous researches have proved the value of TUI and MRI in the overview of levator ani muscles and diagnosis of muscle avulsion [6, 11,12,13,14]. Conventional 2D ultrasound with abdominal transducer was also used to detect levator defects [15]. High-frequency two-dimensional (2D) ultrasound was used to evaluate the biological function of levator ani muscles by elastography [16, 17]. Levator ani muscle was in a superficial position under perineum, so we raised the hypothesis that high-frequency 2D ultrasound could show a more clear image of levator ani muscle. After repeated clinical practice, we found high-frequency 2D ultrasound could demonstrate more details such as muscle fibers when compared with conventional 2D mode. However, to our knowledge, there has been no research concerning about the role of high-frequency 2D ultrasound in evaluating the thickness of puborectalis muscle and detecting muscle avulsion.
In this study, we, therefore, tried to evaluate the thickness of puborectalis muscle and detect muscle avulsion with high-frequency 2D ultrasound. TUI mode was also used to detect muscle avulsion to estimate the validity of the new method.
Patients and methods
This prospective, observational study was conducted by Department of Ultrasound in Medicine of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital from March 2018 to January 2019. The study design was approved by the Human Ethics Committee of the hospital. A total of 164 women who went to the urological and gynecological clinic of the hospital for consultation of pelvic floor discomfort, such as pelvic organ prolapse, urine incontinence, vaginitis, pelvic inflammatory disease, dysuria and sexual pain were included. Women with prior surgery for incontinence or prolapse and those who were unable to perform a maximum muscle contraction after repeating several times were excluded. All enrolled women were required to have a standardized clinical questionnaire, physical examination for prolapse according to POP quantification system and transperineal ultrasound examination. POP quantification grade 2 or higher refers to prolapse situated ≤ 1 cm above the hymen.
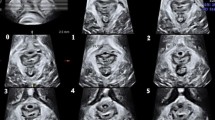
A 11L-D 2D linear transducer (GE Medical System, Zipf, Australia) was placed at an inclination of 10–20° from mid-sagittal plane to detect muscle insertion on the inferior pubic ram [15]. The image of a normal intact of the muscle on the inferior pubic ramus on high-frequency 2D ultrasound represented as hyperechogenic muscle fibers clearly visible from muscle insertion to anorectal junction. Puborectalis muscle defect or avulsion was diagnosed if there was a detachment or avulsion of its muscle insertion from the pelvic sidewall, representing as the normal insertion being replaced by an abnormal hypoechogenic zone on high-frequency 2D ultrasound. The muscle thickness should be measured vertical to muscle fibers, starting from the muscle insertion on maximum muscle contraction, and the measurements were taken at intervals of 0.5 cm (Fig. 1a, b). A total of three measurements were taken and the three measured values were averaged.
a High-frequency 2D ultrasound view of normal puborectalis muscle insertion on the inferior pubic ram, muscle thickness was measured vertical to muscle fibers from the muscle insertion at intervals of 0.5 cm. b High-frequency 2D ultrasound view of puborectalis muscle avulsion of its muscle insertion from the pelvic sidewall, with the normal insertion being replaced by an abnormal hypoechogenic zone, as marked by arrow, muscle thickness was measured. c Tomographic image of normal puborectalis muscle insertion on the inferior pubic ram, LUG was performed from the center of the hypoechogenic structure indicating the urethral mucosa and smooth muscle to most medial aspect of the muscle insertion. d Tomographic image of puborectalis muscle avulsion, with obvious defects in the central three slices, as marked by arrow, LUG was performed. PR pubic rami, PRM puborectalis muscle
Tomographic ultrasound was performed on every woman after bladder emptying with the RAB4-8-D 3D volume transducer (GE Medical System, Zipf, Australia) placed on the perineum in the mid-sagittal plane at maximum muscle contraction. A series of eight tomographic images were obtained in the axial plane at pelvic muscle contraction at intervals of 2.5 mm from 5.0 mm below to 12.5 mm above the plane of minimal levator hiatus. The normal muscle intact on TUI mode represented as puborectalis muscle originating from the pubic rami and forming a symmetrical V-shaped sling towards from the pelvic sidewall to the anorectal junction. The abnormal muscle intact on TUI mode was diagnosed when there was abnormal hypoecho inserted between the muscle and pelvic sidewall. The measurement of LUG was performed from the center of the hypoechogenic structure indicating the urethral mucosa and smooth muscle to most medial aspect of the muscle insertion (Fig. 1c, d). LUG parameters were measured on both sides in the three central slices. A cut-off value of LUG > 25 mm was determined to diagnose puborectalis avulsion [8]. In our study, muscle avulsion was diagnosed once unilateral or bilateral LUG > 25 mm in any one of the three central slices. The images were analyzed separately by two operators professional in diagnosing muscle avulsion, and they were blinded to each other.
Statistical analysis was undertaken using SPSS 22.0 software for Windows (SPSS Chicago, IL, USA). The measurements were expressed as mean ± standard deviation. Mean values were compared using student’s t test. Cohen’s Kappa analysis was used to examine the test agreement between high-frequency 2D ultrasound and TUI mode. Pearson correlation analysis was performed to explore the relationship between the thickness of puborectalis muscle and LUG measurements. A value of P < 0.05 was considered of statistical significance.
Results
Of the all 164 datasets, 6 were excluded from analysis for poor image quality, leaving valid data for 158 patients. The average age of study women was 49 years (range 20–71) and the mean body mass index (BMI) was 22.26 kg/m2 (range 17–29). A total of 143 (90%) women were parous and the median parity was 2 (range 1–7). A total of 107 (67%) women had spontaneous vaginal deliveries, and 36 (23%) women had one or more deliveries assisted by forceps. Presenting complaints were urinary dysfunctions (37%) such as stress incontinence, urge incontinence and dysuria, symptoms of prolapse (23%) such as bladder prolapse, vaginal bulging and heavy sensation, and diarrhea or chronic constipation (23%). After clinical examination (POP-Q system), a total of 108 (68%) women were shown to have severe prolapses (POP-Q grade ≥ 2 or higher).
The agreement between high-frequency 2D ultrasound and TUI mode in diagnosis of muscle avulsion
In the 158 enrolled women, avulsion defects were detected in 57 women (36%), with a proportion of 26 (16%) left defects, 13 (8%) right defects and 18 (12%) bilateral defects on high-frequency 2D ultrasound. On TUI mode, puborectalis avulsion was diagnosed in 60 women (38%), with a proportion of 23 (15%) left defects, 13 (8%) right defects and 24 (15%) bilateral defects. Cohen’s Kappa analysis verified the excellent agreement between high-frequency two-dimensional ultrasound and TUI mode in the diagnosis of avulsion defects (Kappa 0.88, P < 0.05) (Table 1).
Muscle thickness and LUG measurements between women with avulsion defects or normal insertion
The thickness of puborectalis muscle on high-frequency 2D ultrasound and the measurements of LUG on TUI mode are shown in Table 2. The thickness of muscle with avulsion defects was much thinner than the one of normal muscle insertion and LUG measurements of avulsion defects were much larger than those of normal muscle insertion (P < 0.05).
Correlation between the thickness of puborectalis muscle and LUG measurements
Pearson correlation analysis revealed an excellent correlation between the thickness of puborectalis muscle and LUG measurements (r = − 0 .73) (Table 3).
Discussion
Levator ani muscles play a key role in the normal structure and function of the pelvic floor. The levator ani muscles were consisted of the puborectalis, pubococcygeus and iliococcygeus. The puborectalis, the most important part, originates from the pubic rami and forms a V-shaped sling towards from the pelvic sidewall to the anorectal junction. The morphological abnormalities of the puborectalis muscle were closely associated with the alterations in pelvic floor structure and function [18,19,20], acting as a major etiological factor in the pathogenesis of POP and even a high-risk factor of prolapse recurrence [2, 4]. A simple and widely available method of assessing muscle integrity must be of great clinical value.
Different techniques have been peformed in the evaluation of the levator ani muscle [7, 14, 21, 22]. MRI is good at identifying soft tissues and can show the deep structure of the pelvic floor and its spatial adjacent relationship [23]. MRI has not been widely promoted in clinical due to the expensive cost, long examination time and some contraindications such as claustrophobia, metal implants and so on. Intracavitary 3D ultrasound has been used to observe the normal morphology and defects of levator ani muscle in the former studies [24, 25]. However, this examination mode has a high demand on the technique of operation. TUI mode has been widely recognized to be of great value in the diagnosis of muscle avulsion [26]. In this study, the LUG measurements on TUI mode of the avulsion side was 27.55 ± 2.96 mm, which was basically consistent with the result raised by Dietz [27]. High-frequency 2D ultrasound can show more details such as muscle fibers when compared with conventional 2D mode with abdominal transducer. Our study confirmed that high-frequency 2D ultrasound equipped with a linear array transducer in 4–10 MHz range could be performed to demonstrate puborectalis muscle and detect muscle avulsion. Obvious differences were found in the morphology and the thickness of puborectalis muscle between women with and without muscle avulsion. The normal puborectalis muscle without defect illustrates a normal insertion of the muscle on the inferior pubic ramus, with hyperechogenic muscle fibers clearly visible from muscle insertion to anorectal junction. Muscle avulsion was detected with a detachment or avulsion of its muscle insertion from inferior pubic ramus, presenting as an irregular hypoechogenic zone. The phenomenon of more left avulsion and high forceps deliveries rate in our study were similar to other researches existed [10, 20, 28], population characteristics and clinical symptoms of pelvic floor discomfort might be associated with the results. The efficiency of high-frequency 2D ultrasound in detecting muscle avulsion agreed well with TUI mode (Kappa 0.88, P < 0.05). This result suggested that the two methods were of almost equal value in detecting muscle avulsion. Furthermore, the thickness of puborectalis muscle with normal morphology in our study was 9.07 ± 1.73 mm on right and 8.98 ± 1.44 mm on left, the result was mainly consistent with the previous study [29], and the measurements in muscle avulsion group decreased significantly. LUG measurements were much higher in muscle avulsion group than normal insertion group. Pearson correlation analysis revealed the negative relationship that the thinner puborectalis muscle was, the larger LUG would be (r = − 0.73). In clinical practice, we found that different states did not affect the sonographic performance of muscle avulsion, so we considered that it was sufficient to detect muscle avulsion at rest. To perform numerical analysis in the same state, muscle thickness in this study was measured on contraction. The purpose of this study was to examine the feasibility and value of 2D high-frequency ultrasound in detecting muscle avulsion, which was a qualitative research. Therefore, we did not conduct a specific quantitative discussion on the degree of avulsion on both 2D high-frequency ultrasound and TUI mode. However, we observed the difference in amount of residual muscles fibers, which might be associated with the degree of avulsion, the hypothesis would be further analyzed.
As the equipment and system have been widely available, even in some less developed regions, high-frequency 2D ultrasound can be a valuable method in demonstrating puborectalis muscle and detecting muscle avulsion. But there were several limitations that could not be ignored. First, detecting puborectalis muscle on high-frequency 2D ultrasound requires adequate anatomical knowledge and experience in ultrasound examination due to the complex anatomy of levator ani muscles. Second, the accuracy and efficiency of high-frequency 2D ultrasound in detecting muscle avulsion requires to be further verified by other existed methods for detecting muscle avulsion such as MRI and intracavitary 3D ultrasound with a larger sample size.
In conclusion, high-frequency 2D ultrasound, an universally available and convenient examination, is valuable in visualizing the normal morphology and abnormal avulsion of puborectalis muscle. High-frequency 2D ultrasound may be valuable in practice, especially in some areas with backward economic development and medical resources.
References
Walker GJA, Gunasekera P (2011) Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J 22(2):127–135. https://doi.org/10.1007/s00192-010-1215-0
Dietz HP, Simpson JM (2008) Levator trauma is associated with pelvic organ prolapse. BJOG 115(8):979–984. https://doi.org/10.1111/j.1471-0528.2008.01751.x
Cheung RYK, Shek KL, Chan SSC, Chung TKH, Dietz HP (2015) Pelvic floor muscle biometry and pelvic organ mobility in East Asian and Caucasian nulliparae. Ultrasound Obstet Gynecol 45(5):599–604. https://doi.org/10.1002/uog.14656
Model AN, Shek KL, Dietz HP (2010) Levator defects are associated with prolapse after pelvic floor surgery. Eur J Obstet Gynecol Reprod Biol 153(2):220–223. https://doi.org/10.1016/j.ejogrb.2010.07.046
Notten KJ, Weemhoff M, Kluivers KB, Schweitzer KJ, Mulder F, Stoker J, Beets-Tan RG, Futterer JJ, Vliegen RF, Evers JL, Link G, Bergmans MG, Kampschöer PH, Gondrie ET, van Gestel I, van Dooren I, Dirksen C, Smits LJ, Bossuyt PM, Roovers JPWJBWSH (2011) Protocol for Translabial 3D-Ultrasonography for diagnosing levator defects (TRUDIL): a multicentre cohort study for estimating the diagnostic accuracy of translabial 3D-ultrasonography of the pelvic floor as compared to MR imaging. BMC Womens Health 11(1):23. https://doi.org/10.1186/1472-6874-11-23
DeLancey JO, Sørensen HC, Lewicky-Gaupp C, Smith TM (2012) Comparison of the puborectal muscle on MRI in women with POP and levator ani defects with those with normal support and no defect. Int Urogynecol J 23(1):73–77. https://doi.org/10.1007/s00192-011-1527-8
Kearney R, Miller JM, Delancey JO (2006) Interrater reliability and physical examination of the pubovisceral portion of the levator ani muscle, validity comparisons using MR imaging. Neurourol Urodyn 25(1):50–54. https://doi.org/10.1002/nau.20181
Dietz HP, Abbu A, Shek KL (2008) The levator–urethra gap measurement: a more objective means of determining levator avulsion? Ultrasound Obstet Gynecol 32(7):941–945. https://doi.org/10.1002/uog.6268
Yan Y, Dou C, Wang X, Xi Y, Hu B, Ma L, Ying T (2017) Combination of tomographic ultrasound imaging and three-dimensional magnetic resonance imaging-based model to diagnose postpartum levator avulsion. Sci Rep 7(1):11235. https://doi.org/10.1038/s41598-017-08201-9
Dietz HP, Garnham AP, Rojas RG (2016) Is the levator–urethra gap helpful for diagnosing avulsion? Int Urogynecol J 27(6):909–913. https://doi.org/10.1007/s00192-015-2909-0
Rodrigo N, Wong V, Shek KL, Martin A, Dietz HP (2014) The use of 3-dimensional ultrasound of the pelvic floor to predict recurrence risk after pelvic reconstructive surgery. Aust N Z J Obstet Gynaecol 54(3):206–211. https://doi.org/10.1111/ajo.12171
Majida M, Brækken IH, Bø K, Engh MEM (2012) Levator hiatus dimensions and pelvic floor function in women with and without major defects of the pubovisceral muscle. Int Urogynecol J 23(6):707–714. https://doi.org/10.1007/s00192-011-1652-4
Dietz HP (2007) Quantification of major morphological abnormalities of the levator ani. Ultrasound Obstet Gynecol 29(3):329–334. https://doi.org/10.1002/uog.3951
Lammers K, Fütterer JJ, Inthout J, Prokop M, Vierhout ME, Kluivers KB (2013) Correlating signs and symptoms with pubovisceral muscle avulsions on magnetic resonance imaging. Am J Obstet Gynecol 208(2):148.e141–148.e147. https://doi.org/10.1016/j.ajog.2012.12.006
Dietz HP, Shek KL (2009) Levator defects can be detected by 2D translabial ultrasound. Int Urogynecol J Pelvic Floor Dysfunct 20(7):807–811. https://doi.org/10.1007/s00192-009-0839-4
Xie M, Zhang X, Liu J, Ding J, Ren Y, Hua K (2015) Evaluation of levator ani with no defect on elastography in women with POP. Int J Clin Exp Med 8(6):10204–10212
Gachon B, Nordez A, Pierre F, Fradet L, Fritel X, Desseauve D (2019) In vivo assessment of the levator ani muscles using shear wave elastography: a feasibility study in women. Int Urogynecol J 30(7):1179–1186. https://doi.org/10.1007/s00192-018-3693-4
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, Hussain H, Umek W, Hsu Y, Ashton-Miller JA (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109(2):295–302
Otcenasek M, Krofta L, Baca V, Grill R, Kucera E, Herman H, Vasicka I, Drahonovsky J, Feyereisl J (2007) Bilateral avulsion of the puborectal muscle: magnetic resonance imaging-based three-dimensional reconstruction and comparison with a model of a healthy nulliparous woman. Ultrasound Obstet Gynecol 29(6):692–696. https://doi.org/10.1002/uog.4030
Dietz HP, Shek C (2008) Levator avulsion and grading of pelvic floor muscle strength. Int Urogynecol J Pelvic Floor Dysfunct 19(5):633–636. https://doi.org/10.1007/s00192-007-0491-9
Betschart C, Kim J, Miller JM, Ashton-Miller JA, DeLancey JO (2014) Comparison of muscle fiber directions between different levator ani muscle subdivisions: in vivo MRI measurements in women. Int Urogynecol J 25(9):1263–1268. https://doi.org/10.1007/s00192-014-2395-9
Abdool Z, Shek KL, Dietz HP (2009) The effect of levator avulsion on hiatal dimension and function. Am J Obstet Gynecol 201(1):89.e81–89.e85. https://doi.org/10.1016/j.ajog.2009.02.005
Shi M, Shang S, Xie B, Wang J, Hu B, Sun X, Wu J, Hong N (2016) MRI changes of pelvic floor and pubic bone observed in primiparous women after childbirth by normal vaginal delivery. Arch Gynecol Obstet 294(2):285–289. https://doi.org/10.1007/s00404-016-4023-z
van Delft K, Shobeiri SA, Thakar R, Schwertner-Tiepelmann N, Sultan AH (2014) Intra- and interobserver reliability of levator ani muscle biometry and avulsion using three-dimensional endovaginal ultrasonography. Ultrasound Obstet Gynecol 43(2):202–209. https://doi.org/10.1002/uog.13193
Shobeiri SA, Leclaire E, Nihira MA, Quiroz LH, O'Donoghue D (2009) Appearance of the levator ani muscle subdivisions in endovaginal three-dimensional ultrasonography. Obstect Gynecol 114(1):66–72
Turel F, Shek KL, Dietz HP (2019) How valid is tomographic ultrasound imaging in diagnosing levator and anal sphincter trauma? J Ultrasound Med 38(4):889–894. https://doi.org/10.1002/jum.14767
Dietz HP, Bernardo MJ, Kirby A, Shek KL (2011) Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J 22(6):699–704. https://doi.org/10.1007/s00192-010-1329-4
Calderwood CS, Thurmond A, Holland A, Osmundsen B, Gregory WT (2018) Comparing 3-dimensional ultrasound to 3-dimensional magnetic resonance imaging in the detection of levator ani defects. Female Pelvic Med Reconstr Surg 24(4):295–300. https://doi.org/10.1097/spv.0000000000000485
Dierick F, Galtsova E, Lauer C, Buisseret F, Bouché A-F, Martin L (2018) Clinical and MRI changes of puborectalis and iliococcygeus after a short period of intensive pelvic floor muscles training with or without instrumentation. Eur J Appl Physiol 118(8):1661–1671. https://doi.org/10.1007/s00421-018-3899-7
Acknowledgements
National Science Foundation of China (No. 81571699), Shanghai Key Discipline of Medical Imaging Fund (No. 2017 ZZ 02005) and Shanghai Key Clinical Disciplines Fund (No.shslczdzk03203) are acknowledged for providing financial support to this work.
Author information
Authors and Affiliations
Contributions
MZ: project development, manuscript writing, data collection. HD: data analysis. TY: conceptualization, funding acquisition. WS: data collection, project development. CD: data collection.
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. All procedures carried out in this study involving human participants were in accordance with Helsinki Declaration of 1964 and its subsequent amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, M., Du, H., Ying, T. et al. Value of high-frequency two-dimensional ultrasound on evaluating puborectalis muscle. Arch Gynecol Obstet 301, 1347–1352 (2020). https://doi.org/10.1007/s00404-020-05523-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05523-4