Abstract
Purpose
This study aimed to assess the rates of retained products of conception (RPOC) after routine postpartum evaluation of patients who underwent post-delivery manual uterine revision due to retained placenta.
Methods
This is a retrospective cohort study of 599 consecutive women who underwent manual removal of placenta during 2010–2018. Group A comprised 465 women who underwent postpartum symptom-based evaluation (2010–2016). Group B comprised 134 women who were routinely evaluated by ultrasound and subsequently by hysteroscopic examination 6 weeks after delivery (2016–2018).
Results
The rates of abnormal postpartum bleeding were similar between groups A and B (12% and 13%, respectively, p = 0.72%). A significantly smaller proportion of women underwent hysteroscopy in group A than group B (12% vs. 37%, p < 0.05). The rate of persistent RPOC confirmed by hysteroscopy was significantly lower in group A than group B (9.7% vs. 23%, p < 0.05).
Conclusion
Among patients who underwent post-delivery manual removal of placenta, a threefold higher rate of RPOC was discovered by routine elective evaluation than by evaluating only symptomatic patients. Future studies may show whether this approach translates to an effect on fertility.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retained placenta after vaginal delivery is generally defined as failure of spontaneous expulsion of the placenta within 30 min after delivery of the fetus [1]. The reported incidence of retained placenta is in the range of 0.5–3.3% of vaginal deliveries [2, 3]. Possible pathophysiological mechanisms of retained placenta include adherent placenta and failed retroplacental myometrial contraction [2, 4, 5].
Retained placenta can lead to severe early postpartum hemorrhage (PPH). Management of retained placenta is essential to prevent this life-threatening complication. Manual removal of placenta (MROP) after vaginal delivery is widely performed in cases of retained placenta. Instrumental procedures such as curettage may also be used to stop bleeding [6, 7].
Retained products of conception (RPOC) may be observed after removal of retained placenta either manually or instrumentally. The reported incidence of persistent RPOC after vaginal deliveries in women who underwent postpartum MROP is reportedly in the range of 7.2–12.2% [8, 9]. Endometritis, late PPH, intrauterine adhesions and infertility are possible sequels of RPOC. In terms of these potential sequels, a matter of debate is whether the routine diagnosis and treatment of RPOC are essential in women who underwent MROP, or whether these should be limited to patients with bleeding symptoms. Our study aimed to compare rates of persistent RPOC between these two patient groups.
Materials and methods
The study was approved by the Institutional Review Board of Barzilai University Medical Center (Protocol number 0052-19-BRZ). The records of 31,066 vaginal deliveries between January 2010 and September 2018 were reviewed. Women who underwent singleton vaginal deliveries beyond 24 weeks of gestation with MROP due to retained placenta were included in the study. Exclusion criteria included cesarean deliveries, multiple gestations. We compared rates of persistent RPOC over 2 distinct time periods. Before September 2016, women who underwent MROP were not routinely evaluated for persistent RPOC. Rather, only those with prolonged or late postpartum vaginal bleeding were referred for hysteroscopic evaluation. In September 2016, we changed our departmental protocol such that all patients with MROP, regardless of bleeding symptoms, were scheduled to undergo routine ultrasonographic evaluation 6 weeks after delivery. The two groups were not concurrently observed; rather, the routine evaluation group (group B) was observed after Group A. Group A comprised vaginal deliveries with MROP from January 2010 until August 2016, during which women were referred to hysteroscopic evaluation upon prolonged postpartum vaginal bleeding. Prolonged postpartum uterine bleeding was defined as the continuation of bleeding or bloody discharge for more than 6 weeks in the postpartum period. Group B comprised vaginal deliveries with MROP from September 2016 until September 2018, during which all patients with MROP, regardless of bleeding symptoms, were scheduled to undergo routine ultrasonographic evaluation 6 weeks after delivery. Two physicians and two sonography technicians were responsible for sonographic examinations in our institution. Abnormal sonographic findings included: thick irregular endometrium > 15 mm, hyperechogenic mass, and hypoechogenic intrauterine mass with blood flow on Doppler scan. Patients with abnormal ultrasonographic findings were referred for hysteroscopic evaluation.
All hysteroscopic procedures were performed in our center. All patients initially underwent diagnostic hysteroscopy in an office hysteroscopy setting. Diagnostic hysteroscopy was performed using a rigid 2.8-mm hysteroscope. Patients with findings of RPOC were scheduled for operative hysteroscopy. Operative hysteroscopy procedures were performed in the operating room under general anesthesia or sedation. All hysteroscopies were performed by one of the 2 specialists experienced in hysteroscopy. Histologic diagnosis of RPOC was defined as the presence of trophoblastic tissue.
Accrued data included demographics, gestational age of delivery, time interval between delivery, and hysteroscopic, ultrasonographic, hysteroscopic, and histological findings. We compared the rates of RPOC confirmed by hysteroscopy and histology between patients treated during the two time periods.
The sample size calculation was based on the prevalence of RPOC after MROP in previous studies, as 7.2–12.2% [8, 9]. Based on the lower rate (7.2%), we assumed a 15% increase in the rate of RPOC in patients who underwent routine evaluations (Group B). With an Alfa of 0.05 and a power of 0.80, the sample size was determined as 83 patients for each group. Continuous variables were compared using the Student’s t test. For the categorical variables, Chi-square test was performed. A p value of less than 0.05 was considered significant.
Results
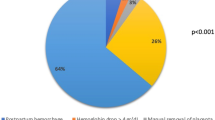
Figure 1 shows the study flow diagram. Altogether, 599 women underwent MROP after vaginal delivery during the entire study period (2010–2018). Prior to the change in protocol, 465 women underwent symptom-based postpartum evaluation (Group A). After the change in protocol, 134 women underwent routine postpartum evaluation (Group B).
Patient characteristics are shown in Table 1. Statistically significant differences were not observed between the groups in baseline characteristics: maternal age, gestational week at delivery, or the proportion of women who were breastfeeding. In Group A, 55 (12%) women underwent hysteroscopy due to the diagnosis of suspected RPOC. In Group B, all women underwent routine 6-week postpartum ultrasound evaluations, either in our department (n = 117) or in public health services (n = 17). Fifty (37%) women in Group B underwent hysteroscopy due to ultrasonographic signs of RPOC. The rates of RPOC diagnosed both by hysteroscopy (23% vs. 10%, p < 0.001) and histology (21% vs 7%, p < 0.001) were higher in Group B. The interval between delivery and hysteroscopy was significantly longer in Group A than in Group B (86 ± 40 vs. 66 ± 13 days, p = 0.03). In both groups, there was one uterine perforation during hysteroscopy that was managed conservatively.
Discussion
The main finding of this study is that a change in departmental protocol, which entailed scheduling of routine ultrasonography for all women with MROP, yielded a threefold increase in the rate of persistent RPOC confirmed by histology (21% vs. 7%, p < 0.05).
Our report of a 12% rate of persistent RPOC requiring surgical treatment in women with symptom-based evaluation concurs with previously reported rates of 7–12% [8, 9]. Weissbach et al. [8] evaluated the predictive value of immediate postpartum ultrasound in 399 women who underwent MROP after vaginal delivery. In their retrospective study, the rates of late postpartum intervention (both medical and surgical) due to RPOC were 7.2% and 7.9% in patients with and without immediate postpartum ultrasound, respectively. A recently published prospective comparative study of women with (n = 293) and without (n = 293) MROP after vaginal delivery reported a 12% rate of RPOC requiring surgical intervention (operative hysteroscopy or suction curettage) within 12 weeks postpartum in patients with MROP [9]. Notably, the response rates to the telephone questionnaire used in that research were 86.7% and 78.5% for the study and control groups, respectively. Additionally, the histologic results of surgical interventions were available in only 11 cases.
For women who underwent routine sonographic evaluation 6 weeks after delivery, we report rates of RPOC by hysteroscopy and histology as 23% (n = 31) and 21% (n = 28), respectively. This compares with a 33% rate of RPOC in hysteroscopic evaluations at 3–4 months after delivery among 100 women with retained placenta who underwent curettage within 24 h of delivery due to failed MROP [6]. In that study, the need for curettage due to failed MROP could indicate an adherent placenta, which may explain the higher rate of RPOC even 3–4 months after delivery.
Hysteroscopy is a widely used invasive procedure for the diagnosis and treatment of RPOC. This technique enables direct visualization of the uterine cavity and prevents damages to unaffected endometrium. RPOC resolves spontaneously after 6 weeks expectant management in up to 90% of women, according to previous reports [10, 11]. In our series, the intervals between delivery and hysteroscopy were 86 ± 40 and 66 ± 13 days in Groups A and B, respectively. This interval could be enough time to allow spontaneous resolution.
In our series, the rate of RPOC confirmed by histology was threefold higher in women who underwent routine evaluation following MROP (21% vs. 7%). However, these results should be interpreted cautiously. Notably, in Group B, 116 (87%) of the women with routine postpartum evaluation were without abnormal bleeding. The diagnosis and treatment of RPOC in asymptomatic patients are controversial. It is currently unclear if early diagnosis of postpartum RPOC may prevent possible sequels like infertility or intrauterine adhesions. Previously reported studies do not show consistent results in this regard [12,13,14].
Serial US examinations could be a choice in the expectant management of RPOC. Because of lacking well-designed prospective randomized trials [11], there is no standard of care in cases with RPOC. Furthermore, in terms of possible sequels, as previously mentioned, the possible malpractice and legal issues could also be a reason for surgical intervention rather than expectant management.
In the current cohort, cases with RPOC that were diagnosed by hysteroscopy, 73% (33/45) and 90% (28/31) of them were confirmed by histology, in Group A and Group B, respectively (Table 1). This discrepancy between hysteroscopy and histology was also reported previously. The study by Vitner et al. [15] also found a low positive predictive value (74%) of hysteroscopy in the diagnosis of RPOC.
However, our study has some limitations inherent to its retrospective design that should be acknowledged. Nevertheless, baseline characteristics were similar between the groups, and other than the change in protocol, no other change is known to have occurred between the study periods that would be expected to affect the outcomes. Furthermore, information bias is a pervasive issue in retrospective studies, and variable that may affect the rate of persistent RPOC such as the prevalence of placenta increta was not consistently available.
Our results could be considered in the management of women with MROP after vaginal delivery. We assume that further studies with a larger patient cohort, ideally in a randomized control setting, will be required to evaluate this subject. In terms of a possible sequel of retained placenta, further studies should be conducted to evaluate whether the routine postpartum evaluation of women after MROP may improve subsequent fertility outcomes.
References
Deneux-Tharaux C, Macfarlane A, Winter C, Zhang WH et al (2009) Policies for manual removal of placenta at vaginal delivery: variations in timing within Europe. BJOG 116:119–124
Weeks AD (2008) The retained placenta. Best Pract Res Clin Obstet Gynaecol 22:1103–1117
Cheung WM, Hawkes A, Ibish S, Weeks AD (2011) The retained placenta: historical and geographical rate variations. J Obstet Gynaecol 31:37–42
Combs CA, Laros RK (1991) Prolonged third stage of labor: morbidity and risk factors. Obstet Gynecol 77:863–867
Weeks AD (2003) Placental influences on the rate of labour progression: a pilot study. Eur J Obstet Gynecol Reprod Biol 106:158–159
Hrazdirova L, Svabik K, Zizka Z, Germanova A, Kuzel D (2012) Should hysteroscopy be provided for patients who have undergone instrumental intrauterine intervention after delivery? Acta Obstet Gynecol Scand 91:514–517
Rosenstein MG, Vargas JE, Drey EA (2014) Ultrasound-guided instrumental removal of the retained placenta after vaginal delivery. Am J Obstet Gynecol 211(180):e1–e3
Weissbach T, Haikin-Herzberger E, Bacci-Hugger K, Shechter-Maor G, Fejgin M, Biron-Shental T (2015) Immediate postpartum ultrasound evaluation for suspected retained placental tissue in patients undergoing manual removal of placenta. Eur J Obstet Gynecol Reprod Biol 192:37–40
Anteby M, Many A, Ashwal E, Yogev Y, Shinar S (2019) Risk factors and complications of manual placental removal after vaginal delivery: How common are additional invasive procedures? J Matern Fetal Neonatal Med 32:384–388
Sotiriadis A, Makrydimas G, Papatheodorou S, Ioannidis JP (2005) Expectant, medical, or surgical management of first-trimester miscarriage: a meta-analysis. Obstet Gynecol 105:1104–1113
Nanda K, Peloggia A, Grimes D, Lopez L, Nanda G (2006) Expectant care versus surgical treatment for miscarriage. Cochrane Database Syst Rev 2:CD003518
Barel O, Krakov A, Pansky M, Vaknin Z, Halperin R, Smorgick N (2015) Intrauterine adhesions after hysteroscopic treatment for retained products of conception: what are the risk factors? Fertil Steril 103:775–779
Hooker AB, Muller LT, Paternotte E, Thurkow AL (2015) Immediate and long-term complications of delayed surgical management in the postpartum period: a retrospective analysis. J Matern Fetal Neonatal Med 28(16):1884–1889
Melcer Y, Smorgick N, Schneider D, Pansky M, Halperin R, Ben-Ami I (2016) Infertility Following retained products of conception: Does the timing of surgical ıntervention matter? Isr Med Assoc J 18:605–608
Vitner D, Filmer S, Goldstein I, Khatib N, Weiner Z (2013) A comparison between ultrasonography and hysteroscopy in the diagnosis of uterine pathology. Eur J Obstet Gynecol Reprod Biol 171(1):143–145
Author information
Authors and Affiliations
Contributions
AN: manuscript writing–editing, data analyzing; NE: data collection, data analyzing; EI: data collection; EZ: data analyzing; SS: data analyzing; VK: data analyzing; EYA: manuscript editing, supervsior; OG: Supervisor, project administration, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
The study was designed as a retrospective study. All data was collected anonymously. The Ethical board waived informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Namazov, A., Elkabetz, N., Ivshin, E. et al. Routine ultrasonographic and hysteroscopic evaluations of women undergoing postpartum manual removal of placenta: a retrospective cohort study. Arch Gynecol Obstet 301, 715–719 (2020). https://doi.org/10.1007/s00404-020-05433-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05433-5