Abstract
Purpose
The aim of this systematic review was to evaluate the associations between pre-pregnancy body mass index and gestational weight gain and placental abruption.
Methods
Relevant studies were identified from PubMed, EMBASE, Scopus and CINAHL. Unpublished findings from analyses of linked population-based data sets from Western Australia (2012–2015, n = 114,792) were also included. Studies evaluating pre-pregnancy body mass index and/or gestational weight gain and placental abruption were included. Two independent reviewers evaluated studies for inclusion and quality. Data including odds ratios (ORs) and 95% confidence intervals (CIs) were extracted and analysed by random effects meta-analysis.
Results
21 studies were included, of which 15 were eligible for meta-analyses. The summary ORs for the association of being underweight, overweight and obese, and placental abruption, compared to normal weight women, were 1.4 (95% CI 1.1, 1.7), 0.8 (95% CI 0.8, 0.9) and 0.8 (95% CI 0.7, 0.9), respectively. These findings remained unchanged when each study was eliminated from the analysis and in subgroup analyses. Although data were scarce, women with gestational weight gain below the Institute of Medicine recommendations appeared to be at greater risk of abruption compared with women who had optimal weight gain.
Conclusions
Mothers that are underweight prior to or in early pregnancy are at a moderately increased risk of placental abruption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Placental abruption affects 0.3–1% of pregnancies in high-income countries [2]. It is associated with an increased risk of short- and long-term adverse outcomes, including maternal postpartum haemorrhage, shock and cardiovascular disease as well as an increased risk of perinatal morbidity and mortality [1, 11, 20]. Clinical management involves either careful maternal–fetal surveillance or, in cases where there is evidence of maternal or fetal compromise, immediate delivery of the fetus [38]. A better understanding of the risk factors associated with placental abruption may help to identify at-risk women requiring closer monitoring during pregnancy.
Although the etiology of placental abruption remains unknown, multiple risk factors including smoking and hypertensive disorders of pregnancy (HDP) have been identified [4, 44]. While the rate of smoking during pregnancy has declined or remained stable across many high-income countries, an increasing trend in the prevalence of placental abruption has been reported in some countries [2, 3, 35], suggesting a change in the underlying risk factors or diagnosis. Emerging evidence [40] suggests that pre-pregnancy body mass index (BMI) and gestational weight gain (GWG) may be associated with the development of placental abruption, although the mechanisms are not yet clear.
Pre-pregnancy obesity and excessive GWG are already serious public health challenges as they are increasingly prevalent conditions which are associated with adverse maternal and child outcomes [14, 37]. They are associated with higher risk of HDP [52], which in turn are linked with greater risk of placental abruption [4]. However, there is conflicting evidence on the nature of the association between pre-pregnancy BMI and GWG and placental abruption and few insights into causal processes. Some studies [18, 26, 26, 26] have shown an increased risk of abruption in women with underweight or GWG below the Institute of Medicine (IOM) recommendations [29], another study [30] reported an increased risk for overweight and obese women, while other studies [17, 42] found no association. The increasing prevalence of maternal obesity and conflicting results from limited existing research underscore the need for a systematic review, including meta-analysis, to summarise the link between pre-pregnancy BMI and GWG, and placental abruption. Such evidence can help guide further research in this area and inform clinical practice.
This systematic review aimed to evaluate the associations of pre-pregnancy BMI and GWG, and placental abruption. We further enhanced the meta-analysis by including unpublished findings from analyses of linked population-based data sets in Western Australia (WA).
Methods
Literature review
This review followed the methodology for a systematic review and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [32]. The protocol for this review was registered in PROSPERO (CRD42018115427) and the completed MOOSE checklist is included as a supplementary material.
Search strategy and study selection
PubMed, EMBASE, Scopus and CINAHL databases were searched, using key words tailored to each database, from their inception until November 2018. Results were restricted to English language and human domain. While some databases searched included unpublished studies that form part of the grey literature (e.g., conference abstracts), a specific search of the grey literature was not conducted. In addition, citations and reference lists of relevant studies were manually searched until the end of November 2018. Details of the search terms used are in a supplement file (Appendix S1 in Supplementary material).
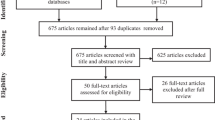
All citations were first imported into an Endnote library and duplicates removed. The remaining records were screened by their titles. All abstracts that passed the title screening were reviewed by two independent reviewers (AAA and HDB). Full-text documents of the eligible abstracts were further examined by the same authors (Fig. 1). At both stages, any disagreements were resolved through face-to-face discussions.
Inclusion and exclusion criteria
Original cohort, case–control or cross-sectional studies that evaluated pre-pregnancy BMI and/or GWG as exposure and placental abruption as an outcome were included while reviews, commentaries, editorials, theses, conference abstracts, or case only (without control) studies were not. Clinically diagnosed partial or complete placental abruption, regardless of whether bleeding was observed, was the sole outcome of interest. As the risk for placental abruption is higher among women bearing twins or higher order multiple pregnancies [44], this review was limited to singleton pregnancies. Consequently, studies which included multiple pregnancies without providing separate findings for singleton pregnancies were excluded.
Quality and risk of bias assessments
The Joanna Briggs Institute (JBI) critical appraisal tools for case–control and cohort studies were used to assess the methodological quality and extent of biases addressed during the design, conduct and analysis of each included study [33]. Risk of bias for each study was assessed following the GRADE approach [23]. Two of the authors (AAA and HDB) performed the independent appraisal.
Data extraction
Data extracted include study details (first author last name, year of publication, period, country, source population and study design), data collection methods/source and sample size, exposure (pre-pregnancy BMI and/or GWG) definition, measurement and timing, outcome (placental abruption) diagnosis and characteristics (e.g., partial or complete), effect estimates [odds ratios (ORs) with 95% confidence intervals (CIs)] as well as adjustment factors. One of the authors (AAA) extracted these data into a standardized excel sheet and another investigator (HDB) verified the results.
The current study (WA-linked data)
Data were obtained from two core population health data sets [25]—the Midwives’ Notification System (MNS) and Hospital Morbidity Data Collection (HMDC). Both are linked routinely by the Data Linkage Branch (DLB) of the WA Government Department of Health. The MNS records the circumstances of all births of 20 weeks or more gestation, with information received from attending midwives since 1980, and was used as a primary data source to establish the cohort. The HMDC comprises inpatient separation records for all public and private hospitals in WA since 1970. While maternal height has always been routinely recorded in the MNS, maternal weight was only collected from 2012. Thus, for this analysis, we included all singleton births of at least 20 weeks of gestation in WA between 2012 and 2015.
The DLB linked these data sets together by probabilistic linkage method [41] using common identifiers including name, address and the birthdate of the baby, and securely transferred the data (with identifying fields removed) to the research team.
Study variables of the current study
Weight and height measured at the first antenatal booking (or self-reported pre-pregnancy weight which was obtained if antenatal booking was after 20 weeks of gestation) were extracted from the MNS data set and were used to estimate the pre-pregnancy BMI [weight (kg)/height (m)2]. Based on their BMI, women were categorised into the World Health Organisation (WHO) BMI classifications [underweight (BMI < 18.5), normal weight (BMI 18.5–24.99), overweight [BMI 25–29.99] and obese (BMI ≥ 30)] [51]. Women were classified as having a placental abruption if placental abruption was listed in ‘complications of pregnancy’ in the MNS or as principal or additional diagnosis of premature separation of the placenta [Australian Modification of the 10th edition of International Classification of Disease (ICD-10-AM) code O45] in HMDC.
Other important variables reported in the MNS were categorised as follows: smoking during pregnancy, essential hypertension, pre-eclampsia (all yes/no), maternal age at birth (<25, 25–29, 30–34, ≥ 35 years), ethnicity (Caucasian/non-Caucasian), parity (0, 1, ≥ 2), first antenatal care visit (≤ 12 weeks of gestation, > 12 weeks of gestation), socioeconomic status (SES) quintiles [1st (most disadvantaged) to 5th (least disadvantaged)]. This area-based SES variable was derived using the Australian Bureau of Statistics Index of Relative Socio Economic Disadvantage, which ranks the relative level of disadvantage of areas using a range of measures including income, educational attainment, employment status, occupational skill and housing [36]. Essential hypertension was derived from medical conditions recorded in the MNS or as a HMDC diagnosis (ICD-10-AM code I10) in any admission prior to the birth, while pre-eclampsia was derived from information on complications of pregnancy recorded in the MNS or as a HMDC diagnosis (ICD-10-AM codes O11 and O14) in any admission during pregnancy.
Statistical analysis of the current study
Logistic regression was used to estimate ORs and their 95% CIs for the associations of pre-pregnancy BMI and placental abruption. Maternal age, ethnicity, parity, time of first antenatal care visit, SES, smoking during pregnancy, essential hypertension and pre-eclampsia were included in the model as confounders/covariates based on previous literature [44].
Meta-analysis
Random effects meta-analysis, which accounts for both within and between-studies variability [22], was used to calculate the aggregated effect estimates of included studies and the current study and forest plots produced. Heterogeneity between studies was evaluated using the I2 statistic [24]. Separate meta-analyses were done for each weight classification (underweight, overweight and obese) and only studies which followed the standard WHO BMI classifications were included in the main meta-analyses.
Subgroup analyses based on study size (< 20 vs. ≥ 20 placental abruption cases in each BMI group), data source (hospital vs. population), adjustment for prominent risk factors for abruption [4] (smoking during pregnancy: yes/no; pre-eclampsia: yes/no), and BMI (measured/extracted from records vs. self-reported) were performed. Sensitivity analyses were performed to assess the source of heterogeneity. Models were run to assess the impacts of the (1) exclusion of each study one at a time and (2) exclusion of studies with unadjusted models only, and (3) including studies which either did not use the WHO BMI classifications for underweight, normal weight, overweight or obese or used a group other than normal weight as a reference. Stata version 15 (StataCorp. 2017, College Station, TX, USA) was used for all analyses.
Results
Current WA study
Data were available for 114,792 singleton births of over 20 weeks gestation between 2012 and 2015 in WA. Of these, 688 (0.6%) births were complicated by placental abruption. The ORs for being underweight, overweight and obese and the abruption risk compared with normal weight women were 1.6 (95% CI 1.1, 2.2), 0.8 (95% CI 0.7, 1.0) and 0.6 (95% CI 0.6, 1.0), respectively (Table S1).
Systematic review
Of 3981 records identified via database searching, 1647 were found to be duplicates (Fig. 1). After title assessment of 2370 records, 59 full-text articles were evaluated and 20 articles [7,8,9,10, 12, 13, 17,18,19, 26,27,28, 30, 39, 40, 42, 43, 47, 49, 50] were included in this review. Reasons for the exclusions are listed in Fig. 1. Fourteen published studies [7, 8, 10, 12, 17,18,19, 27, 28, 30, 40, 42, 43, 47] were included in at least one meta-analysis with eight of these [7, 10, 17, 18, 28, 40, 42, 47] included in the main meta-analyses as well as the current study based on the WA-linked data; while the remaining six [8, 12, 19, 27, 30, 43] were included in the sensitivity analyses. Six studies [9, 13, 26, 39, 49, 50] were only included in qualitative reviews as they did not use the WHO BMI definition or there were limited number of studies to perform meta-analysis of GWG (Table S2).
Characteristics of studies included in the meta-analysis
Table 1 and Table S1 summarise the characteristics of studies included in the meta-analyses. Of the 15 studies, 80% were cohort studies and 20% case–control studies, with 53% being population-based. The sample size of included studies ranged from 144 to 461,729 women. Overall over 7145 women with a placental abruption (at least 773 underweight, 4670 normal weight, 666 overweight and 1036 obese), and 594,773 controls were included in the main meta-analyses. Nine of the studies [7, 10, 17, 18, 28, 40, 42, 47] used the WHO BMI classifications, while six [8, 12, 19, 27, 30, 43] adopted slightly different definitions: such as collapsing underweight and normal weight groups (n = 1), or using other cutoffs to define underweight, normal weight, overweight or obese groups (n = 5). Eight published studies [7, 8, 10, 12, 17, 30, 42, 43] reported BMI calculated from anthropometric measurements obtained mainly at the first antenatal booking or extracted from antenatal records, while the remainder [18, 19, 27, 28, 40, 47] used self-reported pre-pregnancy weight and/or height or did not specify the source.
There was variation in the choice of model confounders/covariates of in-scope studies. While most studies adjusted for maternal age or parity, seven published studies [17,18,19, 27, 28, 40, 42] adjusted for smoking during pregnancy, of which three studies [18, 27, 40] additionally adjusted for pre-existing hypertension and pre-eclampsia, and the other six [17,18,19, 27, 40, 42] further adjusted for SES or education (Table 1). In addition to these factors, the current WA study also adjusted for timing of first antenatal care visit and ethnicity.
Most of the studies included in the meta-analysis were high quality based on the JBI quality assessment scale, with seven of the studies scoring 8 or above (Table 1 and Table S3). The risk of bias using the GRADE approach was low for most studies, with none assessed as having a high risk of bias (Table S4).
Meta-analyses of the association between BMI and placental abruption
The meta-analyses included eight published studies [7, 10, 17, 18, 28, 40, 42, 47] each for the association between being underweight, overweight, and obese and risk of placental abruption as well as the current WA study. While four of these published studies [7, 10, 17, 28] were included in all three meta-analyses, four studies [18, 40, 42, 47] contributed data for only some of the BMI categories (Table 2). There was an elevated risk of placental abruption among underweight women when compared with normal weight women (summary OR = 1.4; 95% CI 1.1, 1.7)—with a moderate degree of heterogeneity (I2 = 55.2%). Conversely, there was a reduced risk among overweight (OR = 0.8, 95% CI 0.8, 0.9; I2 = 0%) and obese (OR = 0.8, 95% CI 0.7, 0.9; I2 = 28.2%) women (Fig. 2).
Similar results to the main analyses were obtained in the sensitivity analyses excluding each study; even the exclusion of the large study by Deutsch et al. [18] (weight 30%) did not substantially change the effect of being underweight (Fig S1). Largely consistent results were also obtained when the analyses were stratified by study size (< 20 vs. > 20 cases), data source (hospital vs. population), whether there was adjustment for smoking during pregnancy or pre-eclampsia and method of weight/height ascertainment (measured, extracted from records or self-reported) as well as in the analyses excluding studies which reported unadjusted findings (Figs S2 to S7). By contrast, the summary ORs for all BMI groups were attenuated, with confidence intervals spanning the null value when studies [8, 12, 19, 27, 30, 43] which used a group other than normal weight as a reference and/or do not use the WHO BMI categories were added to the main analyses (Fig S8).
Qualitative review of BMI studies excluded from meta-analyses
Qualitative reviews were done on four studies in which the BMI categories or reference group had major differences to the other studies (Table S2). Of the three studies that reported findings for women with high BMIs, one US study [9] found a higher risk of placental abruption (n = 11,926) among morbidly obese women (BMI > 35) compared with non-obese women (BMI of 19–27; OR = 1.4, 95% CI 1.3, 2.0, after adjustment for race, parity, substance use and pre-existing medical conditions). By contrast, the other two reported no association. The first of these was a multicentre US study [49] (n = 16,102) which categorised women as being obese (BMI 30–34.9), or morbidly obese (BMI ≥ 35), and used women with BMI < 30 as the reference group; this study may have been underpowered with < 15 women with placental abruption in both the obese categories. The second was a large study (n = 610,969) [13], based on the Swedish Medical Birth Registry, which categorised women into three high-BMI groups (29.1–35, 35.1–40 and > 40) and used women with BMI of 19.8–26 as the reference group.
The fourth study was a US nested case–control study [50] (143 cases and 1257 controls) which reported an increased risk of abruption among underweight women (BMI < 18) compared to women with a pre-pregnancy BMI of 18–30 (OR 2.3, 95% CI 1.3, 4.1). The model was fully adjusted for a range of factors including smoking during pregnancy.
Gestational weight gain and placental abruption
We did not formally evaluate the association between GWG and placental abruption as there were only two relevant studies [26, 39]: a large US state-based cohort of over a million women [39] and a smaller Taiwanese hospital study with 9301 women (Table S2) [26]. However, both had similar findings, that is, women who had GWG below the IOM guidelines (12.5–18 kg for underweight, 11.5–16 kg for normal weight, 7–11.5 kg for overweight and 5–9 kg for obese) [29] were about 70% more likely to have a placental abruption compared with women who had optimal GWG. Only the larger US study [39] found a significantly lower risk in women who gained above the IOM recommendation (OR 0.7, 95% CI 0.7, 0.7), while the estimate from the Taiwanese study [26] was imprecise (OR 0.9, 95% CI 0.6, 1.5).
Discussion
This systematic review and meta-analysis included 7145 pregnancies complicated by placental abruption and 594,773 controls, drawn from a small number of studies with a moderate degree of heterogeneity in effect estimates. Overall, we found that underweight women were at a moderately increased risk of placental abruption relative to those of normal weight. Unexpectedly, we found that overweight or obese women were less likely to have placental abruption. These findings largely remained unchanged in the subgroup and sensitivity analyses. Based on limited studies, women with GWG below the IOM recommended amount of weight appear to be at greater risk of placental abruption compared with women who had optimal GWG.
The strengths of this systematic review and meta-analysis were that included studies had no time period restriction and we implemented independent record evaluation, risk of bias and quality assessments. However, because of English language restriction, some literature may have been missed and the grey literature were not included. The other limitations were the small number of eligible studies and the low number of placental abruption cases in some studies which precluded a detailed examination of the sources of heterogeneity between studies. Despite the high quality of studies included in the meta-analyses, about half did not adjust for potentially salient confounders such as smoking during pregnancy while 40% used self-reported anthropometric measures to calculate the pre-pregnancy BMI, which may have introduced errors and biases. However, similar findings were obtained when we ran subgroup analyses based on these factors. The other limitations were related to various definitions of BMI and an insufficient number of studies for meta-analysis of GWG and placental abruption. Although our funnel plots did not show striking results (data not shown), there is the potential for publication bias.
The finding of the association between underweight and the increased risk of placental abruption reinforces the importance of attaining normal weight prior to (or early in) pregnancy. Although maternal pre-pregnancy overweight and obesity are prominent current public health challenges, underweight has been given less attention. For instance, studies included in this review documented a considerable number of underweight women, with the proportion ranging from 3% in high-income settings to 18% in upper middle-income countries (Table S1). Globally, about 10% of women are underweight, with the burden highly skewed to low- and middle-income countries [5]. Accordingly, given the majority of studies in this systematic review were in high-income settings, our findings may have considerably greater implications in low- and middle-income settings.
The underlying mechanisms linking maternal underweight and placental abruption risk are unknown, although we speculate that important nutrient deficiencies may play a role. Evidence suggests that underweight women are more likely to have micronutrient deficiencies as a result of poor nutritional intake and, consequently, fewer reserves to deal with the additional nutritional demands of pregnancy [16, 45, 46]. In turn, this suboptimal condition may contribute to the poor development of the placenta and lead to a resultant increased risk of abruption [15, 18]. Moreover, underweight women may have adopted different lifestyles, have underlying medical conditions or they might have chosen to be underweight for various reasons [6]. For example, in the current WA study, the proportion of smoking during pregnancy among underweight women (14.7%) was twice that of normal weight women (7.7%). Similarly, a number of published studies [8, 17,18,19, 39, 42] included in this systematic review and meta-analysis found a greater prevalence of smoking during pregnancy in underweight than normal weight women. Despite adjustment for smoking there could be residual confounding. There could also be unmeasured medical conditions and other unhealthy lifestyle factors (such as methamphetamine use linked with loss of appetite and hypertension) associated with underweight, which may partly explain the association of underweight and the increased risk of placental abruption [34].
Previous research indicates that the impact of being underweight on the risk of placental abruption can be mitigated through pre-pregnancy weight and GWG interventions. For example, Salihu et al. [39] found that the risk of placental abruption in underweight women who gained a substantial amount of weight during pregnancy was similar to the risk for normal-weight women, while the placental abruption risk was lower in women who gained weight above the IOM recommendations. Moreover, in contrast to most obstetrics and perinatal outcomes, the risk of placental abruption was lower in overweight and obese women. Nevertheless, placental abruption is relatively rare, albeit severe when it occurs, compared with other obstetric complications. Therefore, these findings need to be interpreted cautiously and considered in the context of the more prevalent poor short- and long-term health consequences of pre-pregnancy obesity and excessive GWG for mothers and their children [21, 31, 48]. Our findings add to the spectrum of existing reasons why a normal body weight before pregnancy and appropriate GWG are important [29, 37].
In summary, the findings of this systematic review and meta-analysis demonstrate that underweight women have an increased risk of placental abruption while overweight or obese women may have lower risk, when compared to normal-weight women. Although data are scarce, women with GWG below the IOM recommendations appear to be at greater risk of placental abruption. Future research should universally adopt the WHO BMI classifications to allow direct comparisons between studies and allow for pooling of findings. Further research is required to improve our understanding about the mechanisms linking pre-pregnancy BMI and placental abruption risk and to evaluate the impact of GWG interventions for women who are underweight prior to pregnancy.
References
Ananth CV, Hansen AV, Williams MA et al (2017) Cardiovascular disease in relation to placental abruption: a population-based cohort study from Denmark. Paediatr Perinat Epidemiol 31:209–218
Ananth CV, Keyes KM, Hamilton A et al (2015) An international contrast of rates of placental abruption: an age-period-cohort analysis. PLoS One 10:e0125246
Ananth CV, Oyelese Y, Yeo L et al (2005) Placental abruption in the United States, 1979 through 2001: temporal trends and potential determinants. Am J Obstet Gynecol 192:191–198
Ananth CV, Smulian JC, Vintzileos AM (1999) Incidence of placental abruption in relation to cigarette smoking and hypertensive disorders during pregnancy: a meta-analysis of observational studies. Obstet Gynecol 93:622–628
Anonymous (2016) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387:1377–1396
Audrain-Mcgovern J, Benowitz NL (2011) Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther 90:164–168
Avci ME, Şanlikan F, Çelik M et al (2015) Effects of maternal obesity on antenatal, perinatal and neonatal outcomes. J Maternal-Fetal Neonatal Med 28:2080–2083
Bhattacharya S, Campbell DM, Liston WA et al (2007) Effect of body mass index on pregnancy outcomes in nulliparous women delivering singleton babies. BMC Public HEALTH 7:168
Bianco AT, Smilen SW, Davis Y et al (1998) Pregnancy outcome and weight gain recommendations for the morbidly obese woman. Obstet Gynecol 91:97–102
Blumenfeld YJ, Baer RJ, Druzin ML et al (2014) Association between maternal characteristics, abnormal serum aneuploidy analytes, and placental abruption. Am J Obstet Gynecol 211:144.e141–149
Boisrame T, Sananes N, Fritz G et al (2014) Placental abruption: risk factors, management and maternal-fetal prognosis. Cohort study over 10 years. Eur J Obstet Gynecol Reprod Biol 179:100–104
Budde MP, De Lange TE, Dekker GA et al (2007) Risk factors for placental abruption in a socio-economically disadvantaged region. J Maternal-fetal Neonatal Med 20:687–693
Cedergren MI (2004) Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol 103:219–224
Cheney K, Farber R, Barratt AL et al (2018) Population attributable fractions of perinatal outcomes for nulliparous women associated with overweight and obesity, 1990–2014. Med J Aust 208:119–125
Christian P (1973S) Micronutrients and reproductive health issues: an international perspective. J Nutr 133:1969S–1973S
Cucó G, Fernández-Ballart J, Sala J et al (2005) Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr 60:364
Denison FC, Norwood P, Bhattacharya S et al (2014) Association between maternal body mass index during pregnancy, short-term morbidity, and increased health service costs: a population-based study. BJOG Int J Obstet Gynaecol 121:72–81
Deutsch AB, Lynch O, Alio AP et al (2010) Increased risk of placental abruption in underweight women. Am J Perinatol 27:235–240
Ding XX, Xu SJ, Hao JH et al (2016) Maternal pre-pregnancy BMI and adverse pregnancy outcomes among Chinese women: Results from the C-ABCS. J Obstet Gynaecol 36:328–332
Downes KL, Shenassa ED, Grantz KL (2017) Neonatal outcomes associated with placental abruption. Am J Epidemiol 186:1319–1328
Goldstein RF, Abell SK, Ranasinha S et al (2017) Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-analysisAssociation of Gestational Weight Gain With Maternal and Infant OutcomesAssociation of Gestational Weight Gain With Maternal and Infant Outcomes. JAMA 317:2207–2225
Harris RJ, Deeks JJ, Altman DG et al (2008) Metan: fixed-and random-effects meta-analysis. The Stata Journal 8:3–28
Higgins JP, Thompson SG, Deeks JJ et al (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Higgins J, Altman D, Sterne J (2008) on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group (editors). Chapter 8: Assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions version 5
Holman CD, Bass AJ, Rouse IL et al (1999) Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Public Health 23:453–459
Hung TH, Chen SF, Hsu JJ et al (2015) Gestational weight gain and risks for adverse perinatal outcomes: a retrospective cohort study based on the 2009 Institute of Medicine guidelines. Taiwan J Obstet Gynecol 54:421–425
Hung TH, Hsieh CC, Hsu JJ et al. (2007) Risk factors for placental abruption in an Asian population. Reprod Sci (Thousand Oaks, Calif.) 14:59–65
Hung TH, Hsieh TT (2016) Pregestational body mass index, gestational weight gain, and risks for adverse pregnancy outcomes among Taiwanese women: a retrospective cohort study. Taiwan J Obstet Gynecol 55:575–581
Institute of Medicine (Us) and National Research Council (Us) Committee to Reexamine Iom Pregnancy Weight Guidelines (2009) Weight gain during pregnancy; Reexamining the Guidelines. In: Rassmussen KM, Yaktine AL, Institute of Medicine, National Research Council (eds)The National Academic Press, Washington DC
Liu X, Du J, Wang G et al (2011) Effect of pre-pregnancy body mass index on adverse pregnancy outcome in north of China. Arch Gynecol Obstet 283:65–70
Marchi J, Berg M, Dencker A et al (2015) Risks associated with obesity in pregnancy, for the mother and baby: a systematic review of reviews. Obes Rev 16:621–638
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535
Moola S, Munn Z, Tufanaru C et al (2017) Chapter 7: Systematic reviews of etiology and risk. Joanna Briggs Institute Reviewer's Manual, The Joanna Briggs Institute
National Institute on Drug Abuse (2014) DrugFacts: Methamphetamine. http://www.assessmentpsychology.com/icbmi.htm
Pariente G, Wiznitzer A, Sergienko R et al (2011) Placental abruption: critical analysis of risk factors and perinatal outcomes. J Maternal-fetal Neonatal Med 24:698–702
Pink B (2011) Socio-economic indexes for areas (SEIFA). Australian Bureau of Statistics, Canberra
Poston L, Caleyachetty R, Cnattingius S et al (2016) Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol 4:1025–1036
Royal College of Obstetricians and Gynaecologists (Rcog) (2011) Antepartum Haemorrhage: Green top Guideline No. 63. Royal College of Obstetrics & Gynaecology, London
Salihu HM, Diamond E, August EM et al (2013) Maternal pregnancy weight gain and the risk of placental abruption. Nutr Rev 71(Suppl 1):S9–17
Salihu HM, Lynch O, Alio AP et al (2009) Extreme obesity and risk of placental abruption. Hum Reprod (Oxford, England) 24:438–444
Sayers A, Ben-Shlomo Y, Blom AW et al (2016) Probabilistic record linkage. Int J Epidemiol 45:954–964
Scott-Pillai R, Spence D, Cardwell C et al (2013) The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004–2011. BJOG Int J Obstet Gynaecol 120:932–939
Sebire NJ, Jolly M, Harris J et al (2001) Maternal obesity and pregnancy outcome: a study of 287 213 pregnancies in London. Int J Obes 25:1175
Tikkanen M (2011) Placental abruption: epidemiology, risk factors and consequences. Acta Obstet Gynecol Scand 90:140–149
Torheim LE, Ferguson EL, Penrose K et al (2058s) Women in resource-poor settings are at risk of inadequate intakes of multiple micronutrients. J Nutr 140:2051s–2058s
Truong YN, Yee LM, Caughey AB et al (2015) Weight gain in pregnancy: does the Institute of Medicine have it right? Am J Obstet Gynecol 212:362.e361–368
Vinturache A, Moledina N, Mcdonald S et al (2014) Pre-pregnancy Body Mass Index (BMI) and delivery outcomes in a Canadian population. BMC Pregnancy Childbirth 14:422
Voerman E, Santos S, Patro Golab B et al (2019) Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med 16:e1002744
Weiss JL, Malone FD, Emig D et al (2004) Obesity, obstetric complications and cesarean delivery rate—a population-based screening study. Am J Obstet Gynecol 190:1091–1097
Williams MA, Lieberman E, Mittendorf R et al (1991) Risk factors for abruptio placentae. Am J Epidemiol 134:965–972
World Health Organization (2006) Global database on body mass index. http://www.assessmentpsychology.com/icbmi.htm
Zhou A, Xiong C, Hu R et al (2015) Pre-pregnancy BMI, gestational weight gain, and the risk of hypertensive disorders of pregnancy: a cohort study in Wuhan, China. PLoS One 10:e0136291
Acknowledgements
We would like to acknowledge the Data Linkage Branch (Western Australian Government Department of Health), the Midwives’ Notification System and the Hospital Morbidity Data Collection for providing data for this project.
Funding
This research was supported by funding from an Australian National Health and Medical Research Council (NHMRC) Project Grant (APP1127265) which funded AAA, CCJS, FJL and HDB. BMF is also funded by an NHRMC Project Grant (APP1098844). The funding bodies had no part in either the study design, conduct, analysis or interpretation of this study nor the decision to submit this study for publication.
Author information
Authors and Affiliations
Contributions
AAA, HDB, CCJS and FJL designed and conceptualised the study. AAA performed the database searches, data extraction, evaluation and analyses and drafted the manuscript. HDB participated in data extraction, evaluation and analyses. HDB, CCJS, BMF, FJL and SWW critically revised the manuscript. All authors reviewed and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
For the review part, ethics approval was not required. All procedures performed in studies involving human participants were in accordance with the ethical standards of the WA Aboriginal Health Ethics Committee (project 797) and the WA Department of Health Human Research Ethics Committee (project 2016/51) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Adane, A.A., Shepherd, C.C.J., Lim, F.J. et al. The impact of pre-pregnancy body mass index and gestational weight gain on placental abruption risk: a systematic review and meta-analysis. Arch Gynecol Obstet 300, 1201–1210 (2019). https://doi.org/10.1007/s00404-019-05320-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05320-8