Abstract
Objective
To evaluate the clinical and pathological features of endometrial cancer (EC) following breast cancer and to assess the effect of the breast cancer hormone receptor status on subsequent EC.
Materials
A retrospective study based on SEER data of EC patients with a history of breast cancer.
Results
A total of 2142 cases met the inclusion criteria. Compared to that of the general population, the incidence of EC following estrogen receptor-positive (ER+) breast cancer and hormone receptor-negative (HR−) breast cancer increased by approximately 16-fold and 15-fold, respectively. Histologically, the proportions of type II EC following ER+ breast cancer, HR− breast cancer and primary EC were 39.6%, 39.4% and 31.2%, respectively (P < 0.001). The proportions of G3 ECs were 26.9%, 28.2% and 19.8%, respectively (P < 0.001). The proportion of patients who died from miscellaneous malignant tumors among EC patients following breast cancer was significantly higher than the proportion of patients among primary ECs. The overall survival rate was worse for EC patients with a history of breast cancer (P < 0.001). There were no significant differences between patients with EC following ER+ breast cancer and those with EC following HR− breast cancer with regard to stage, lymphatic metastasis, outcome or cause of death.
Conclusions
Compared to the general population, the incidence of EC in patients with breast cancer was increased markedly. Patients with EC following ER+ or HR− breast cancer shared the same clinicopathological features and prognoses. All patients need close monitoring regardless of breast cancer hormone receptor status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer in women, accounting for 25% of cancers in female patients worldwide [1]. More than 70% of breast cancer patients are diagnosed with estrogen receptor-positive (ER+) disease [2]. Since the early 1980s, endocrine therapy, including estrogen receptor inhibitors and aromatase inhibitors (AIs), has been globally used for hormone receptor (HR)-positive breast cancer patients [3,4,5]. Tamoxifen (TAM) can significantly reduce breast cancer recurrence and the risk of contralateral breast cancer but has some side effects [6, 7]. The most significant and deleterious effect appears to be a proliferative effect on the endometrium, which can result in endometrial cancer (EC). Proportion of type II cancer with poor prognosis increases in patients with EC, occuring after breast cancer compared to primary EC [8]. Doctors generally equate EC that occurs after breast cancer with the side effects of hormone therapy. It has been widely accepted that the endometrium should be closely monitored during treatment with TAM [9].
However, 10% of breast cancer patients are diagnosed with hormone receptor-negative (HR−) disease [2]. Among these patients, endocrine therapy is not recommended, and hormone dependence, which is the pathogenic basis of both endometrial and breast cancer, is absent. The characteristics of patients with EC after HR− breast cancer remain unclear. There is no study evaluating the effect of hormone receptor status in breast cancer on subsequent EC. The purpose of this study is to provide data for the prevention and treatment of EC after breast cancer from two perspectives. The first is an exploration of the clinical and pathological characteristics of EC in patients with the history of breast cancer compared with those of primary EC (with/without the history of breast cancer). The second is an evaluation of whether hormone receptor status in breast cancer matters in terms of the prognosis of subsequent EC.
Materials and methods
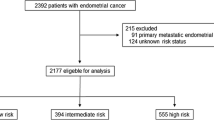
With permission from the Surveillance, Epidemiology, and End Results (SEER) program of the United States National Cancer Institute, clinicopathological, treatment and survival information of women diagnosed with EC or breast cancer during the period from January 1, 2004, to December 31, 2015, was collected. Patients were selected in tabular format in the “Case Listing” option of the SEER* Stat software. Eligibility criteria included the following: (1) a primary diagnosis of breast cancer from 2004 to 2015, (2) estrogen receptor-positive (ER+) status (regardless of progesterone receptor status) or hormone receptor-negative (HR−) status, including estrogen receptor-negative and progesterone receptor-negative status, (3) EC that was diagnosed after breast cancer during the same period, and (4) confirmation of all diagnoses by positive histology.
A total of 2142 patients met the inclusion criteria, and another 105,418 cases with one primary diagnosis of EC alone were extracted as controls. The recorded data included age at diagnosis, histology, grade, stage, lymphatic metastasis, surgery, time interval, cause of death (COD) and overall survival (OS) month. Patients were classified into three age groups: less than 50 years, 50–60 years, and greater than 60 years. Endometrioid adenocarcinoma was classified as type I cancer, and type II EC includes serous adenocarcinoma, clear cell adenocarcinoma, and Mullerian mixed tumors, etc. The differentiation of tumor was reported using a four-grade system: grade 1 (well differentiated), grade 2 (moderately differentiated), grade 3 (poorly differentiated) and undifferentiated. Staging was recorded from stage I to IV. Lymph node metastasis was recorded in two categories: yes or no. Patients with unknown or non-applicable lymph node metastasis status were excluded when calculating P values. Furthermore, survival was calculated as the number of months from cancer diagnosis to death, and each patient's cause-specific death was recorded.
Clinical and pathological characteristics were compared using Pearson's Chi-squared and Fisher's exact tests. The Kaplan–Meier and log-rank tests were used to estimate survival and compare differences between groups, respectively. P values less than 0.05 were considered to indicate statistical significance.
Result
The SEER data included more than 542,000 ER+ and 118,000 HR− breast cancer patients from 2004 to 2015, of which 2142 patients were diagnosed with EC afterwards. A total of 1792 patients had ER+ cancer, and 350 patients had HR− cancer. Overall morbidity of EC was 0.32% in the breast cancer population, 0.33% in the ER+ group and 0.30% in the HR− group. The clinicopathological features of the patients are shown in Table 1. The average age at diagnosis of patients with a history of breast cancer and of patients with primary cancers was 66 and 58 years, respectively. The EC patients with ER+ breast cancer were older than those with HR− breast cancer (diagnosed at over 60 years of age: 70.9% vs. 63.7%, P = 0.006). Histologically, patients with EC following breast cancer were characterized as having more type II ECs (39.5% vs. 31.2%, P < 0.001) and grade 3 ECs (28.7% vs. 19.8%, P < 0.001). These characteristics existed for both ER+ and HR− patients, and there were no significant differences between the two groups. When comparing patients with EC following breast cancer with those diagnosed with primary EC alone, there were no significant differences in the distributions of stage, pelvic metastasis or para-aortic metastasis. The above indicators were also not significantly different between the ER+ and HR− cases.
The overall survival rate of EC following breast cancer was worse than that of primary EC, while there was no difference in the survival rate between the patients with EC following ER+ and HR− cancer (Fig. 1). Regarding proportional COD, the rates of death from miscellaneous cancer (MC) in patients with primary EC and those with EC following breast cancer were 2.5% and 11.7%, respectively. The rates of death from EC of the two groups were 28.8% and 23.2%, respectively. The rates of death from diabetes were 2.0% and 1.4%, respectively. The rates of death from cardiovascular and cerebrovascular disease were 12.8% and 11.0%, respectively. Differences of death from MCs and ECs were significant between the EC patients with a history of breast cancer and those with primary ECs. There was no difference in the rate of other COD between the two groups. Between the ER+ and HR− groups, there was no difference in the rate of COD.
Most patients with EC (70.7%) were diagnosed within 5 years after the diagnosis of breast cancer. This high proportion was more pronounced among patients with ER+ breast cancer (72.2% vs. 62.6%, P < 0.001). The risk of EC in ER+ breast cancer patients decreased gradually with increasing time interval, while a small peak reappeared 6–7 years after the diagnosis of HR− breast cancer (Fig. 2).
Discussion
EC with a history of breast cancer is a specific condition. We found that compared to the general population, the incidence of EC in patients with previous breast cancer increased. In the general population, the incidence of EC in the United States is 0.019% [10]. In our research, based on data from the SEER database, the incidence of EC following ER+ and HR− breast cancers is 0.33% and 0.30%, which is approximately 16 times and 15 times higher, respectively.
Hormone therapy is globally used in patients with HR+ breast cancer. TAM is a representative drug and is widely used, especially in premenopausal patients [11]. A meta-analysis based on four RCTs shows that extended adjuvant TAM is associated with an increase in EC [12]. However, our data show that in patients with HR− breast cancers who do not use TAM, the incidence of EC is still as high, which indicates that EC occurs after breast cancer seems to be mainly derived from intrinsic abnormalities. Genetic carcinogenesis is most likely a factor.
Recent cancer genome studies have led to the identification of scores of cancer genes. There are multiple proven pathogenic genes whose alterations increase susceptibility to breast cancer, including BRCA-1, BRCA-2, P53, HER-2, and PTEN [13,14,15]. In BRCA-1 mutation carriers, the security of genomic safeguard combined with estrogen surveillance is endangered, resulting in accumulated mutations both in mammary and endometrial tissues [16]. Women carrying breast cancer susceptibility genes also preferentially develop EC [17]. PTEN is the most common mutation in type I EC. In type II EC, the most common gene mutations include P53, HER-2 and P16 [18]. It is documented that BRCA-1 expression levels were downregulated in response to transcriptional repression by p53 [19, 20]. Synergistic downregulation of BRCA-1 and p53 accelerates tumor occurrence. Several studies have highlighted the association between breast cancer and high‐risk EC subtypes. A multicenter prospective cohort study including 1083 women with a deleterious BRCA-1 or BRCA-2 mutation demonstrated that BRCA-1+ women are at increased risk of serous/serous-like EC [21]. A study by Liang et al. suggested that women with a prior diagnosis of breast cancer who subsequently developed EC were more likely to have type II cancer, and this effect was independent of TAM exposure [22]. These studies have revealed that predisposing genetic factors may be common to cancers, which also explains the high incidence of type II and high-grade cancers in our study.
In our study, the prognosis and COD between the three groups show several notable features. The first, patients with EC following breast cancer have a worse prognosis than patients with primary EC, and the results of COD show that its real reason is not due to the EC specific mortality. Approximately 20% of the patients died of breast cancer in the group of patients with subsequent EC, which we speculated may be responsible for the poor overall survival. The second, the proportion of women dying of MC among patients with EC following breast cancer is five times higher than that of patients with primary EC, although the overall number of cases is small. MC are interpreted as other types of malignant tumors other than breast and endometrial cancer. We speculate that this is probably attributable to pathogenic gene mutations as discussed, although we do not know the genetic background or mutation characteristics of these cancers. The co-occurrence of endometrial and breast cancer is a high risk factor for miscellaneous cancers. The third, there has no significant difference between patients with EC following ER+ breast cancer and those patients with EC following HR− breast cancer in terms of clinicopathological features and prognoses. This deserves our attention and consideration. Many studies have determined that TAM is closely related to the occurrence of type II and high-grade EC [23]. Doctors are always very anxious about using it, which limits its clinical application to a certain extent. Although in this study, TAM detailed medication information is not available, hormone receptor status can be as a proxy for hormone therapy. There are no significant differences regarding the survival and COD of EC patients in the non-TAM population represented by HR− patients compared with ER+ patients. Some studies have also shown that although the proportion of patients with high-risk EC with a history of breast cancer is increasing, the increase has nothing to do with hormone therapy [24, 25]. Therefore, it can be concluded that TAM may have no adverse effects on the prognosis of EC following ER+ breast cancer. The effect of TAM on the EC requires further study. Finally, what needs to be pointed out is that cardiovascular and cerebrovascular diseases are still an important cause of death in EC patients with a history of breast cancer, although it is fewer in patients with primary EC. It is well known that type I EC is considered to be a metabolic syndrome with high-risk factors, including hypertension, obesity, and diabetes which is closely related to cardiovascular and cerebrovascular accidents. Metabolic syndrome also has an association with breast cancer which should be considered during the follow-up of EC patients with a history of breast cancer [26].
Surveillance is an effective way to prevent disease from progressing into an advanced stage. There were no differences in lymph node metastasis, advanced stage or cancer-specific survival between the patients with EC following breast cancer and those diagnosed with primary EC alone, although the proportions of G3 and type II cancer were significantly higher in the former group. This difference is probably related to clinical monitoring in breast cancer patients. Based on our results, we have the following suggestions for the surveillance of patients with EC following breast cancer. (1) Patients with breast cancer should be alert to the occurrence of EC from the date of diagnosis regardless of hormone receptor status and whether TAM is used. The risk of EC decreases with increasing interval time, and endometrial monitoring should last for at least 5 years. However, vigilance is recommended as there is still a small peak of EC in HR− breast cancer patients 5 years after diagnosis. Endometrial monitoring methods include ultrasound and hysteroscopy. Ultrasonographic abnormalities (including in the uterine body and endometrium) and abnormal uterine bleeding should be further examined by pathology, especially for postmenopausal patients. Endometrial biopsy guided by hysteroscopy should be proposed to women with ultrasonographic abnormalities and/or with uterine bleeding. (2) Other systemic tumors should also be emphasized in the follow-up of patients with EC following breast cancer. MC is an important cause of death among these patients. Early detection and intervention is critical to management. (3) Cardiovascular and cerebrovascular accidents remain an important problem for patients with EC following breast cancer. It is necessary to strengthen multidisciplinary treatment including internal medicine to control metabolic diseases and reduce the risk of death.
Since the exact hormone therapy plan in ER+ breast cancer was unavailable, our research is limited. TAM and AIs are the most commonly used drugs, but their pathogenic effects on EC are different. Therefore, the influencing factors are manifold in EC following ER+ breast cancer. However, until 2015, AI was recommended as the first choice for initial endocrine therapy for postmenopausal women with HR+ early breast cancer by National Comprehensive Cancer Network (NCCN) and European Society for Medical Oncology (ESMO) [27,28,29,30]. Our cases range from 2004 to 2015 in which TAM is still generally recommended and accepted for clinical practice. Theoretically, most of the HR+ patients were exposed to TAM in our research. Therefore, we compared the ER+ cases as a whole with HR− cases and primary EC cases, and our data should not have been biased with respect to the incidence of high-risk EC following breast cancer and its prognosis.
In conclusion, there were higher incidences of EC in patients both with ER+ and HR− breast cancer than in the general population. These EC patients with a history of breast cancer were characterized by higher grade, more type II cancer and poorer overall survival. The clinicopathological features of the patients with EC following ER+ breast cancer were comparable to those of the patients with EC following HR− breast cancer. Additionally, there were no significant differences between the two groups with regard to outcomes. All patients need close monitoring regardless of breast cancer hormone receptor status.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 Cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Ghoncheh Mahshid, Pournamdar Zahra, Salehiniya Hamid (2016) Incidence and mortality and epidemiology of breast cancer in the world. Asian Pac J Cancer Prev 17(S3):43–46
Early Breast Cancer Trialists Collaborative Group (1988) Effects of adjuvant tamoxifen and of cytotoxic therapy on mortality in early breast cancer. An overview of 61 randomized trials among 28,896 women. N Engl J Med 319(26):1681–1692
Fisher B, Costantino J, Redmond C, Poisson R, Bowman D, Couture J et al (1989) A randomized clinical trial evaluating tamoxifen in the treatment of patients with node-negative breast cancer who have estrogen receptor positive tumors. N Engl J Med 320(8):479–484
Winer EP, Hudis C, Burstein HJ, Wolff AC, Pritchard KI, Ingle JN et al (2005) American society of clinical oncology technology assessment on the use of aromatase inhibitors as adjuvant therapy for postmenopausal women with hormone receptor-positive breast cancer: status report 2004. J Clin Oncol 23(3):619–629
Nagykálnai T, Landherr L, Mészáros E (2011) Aromatase inhibitors and arthralgia. Magy Onkol 55(1):32–39
Moscetti L, Agnese Fabbri M, Sperduti I, Fabrizio N, Frittelli P, Massari A et al (2015) Adjuvant aromatase inhibitor therapy in early breast cancer: what factors lead patients to discontinue treatment? Tumori 101(5):469–473
Rieck GC, Freites ON, Williams S (2005) Is tamoxifen associated with high-risk endometrial carcinomas? A retrospective case series of 196 women with endometrial cancer. J Obstet Gynaecol 25(1):39–41
Neri F, Maggino T (2009) Surveillance of endometrial pathologies, especially for endometrial cancer, of breast cancer patients under tamoxifen treatment. Eur J Gynaecol Oncol 30(4):357–360
Lortet-Tieulent J, Ferlay J, Bray F, Jemal A (2018) International patterns and trends in endometrial cancer incidence, 1978–2013. J Natl Cancer Inst 110(4):354–361
Francis PA, Pagani O, Fleming GF, Walley BA, Colleoni M, Láng I et al (2018) Tailoring adjuvant endocrine therapy for premenopausal breast cancer. N Engl J Med 379(2):122–137
Fleming CA, Heneghan HM, O'Brien D, McCartan DP, McDermott EW, Prichard RS et al (2018) Meta-analysis of the cumulative risk of endometrial malignancy and systematic review of endometrial surveillance in extended tamoxifen therapy. Br J Surg 105(9):1098–1106
Romagnolo AP, Romagnolo DF, Selmin OI (2015) BRCA1 as target for breast cancer prevention and therapy. Anticancer Agents Med Chem 15(1):4–14
Bellazzo A, Sicari D, Valentino E, Del Sal G, Collavin L (2018) Complexes formed by mutant p53 and their roles in breast cancer. Breast Cancer (Dove Med Press) 10:101–112
Ngeow J, Sesock K, Eng C (2017) Breast cancer risk and clinical implications for germline PTEN mutation carriers. Breast Cancer Res Treat 165(1):1–8
Suba Z (2015) DNA stabilization by the upregulation of estrogen signaling in BRCA gene mutation carriers. Drug Des Devel Ther 9:2663–2675
MacLachlan TK, Takimoto R, El-Deiry WS (2002) BRCA1 directs a selective p53-dependent transcriptional response towards growth arrest and DNA repair targets. Mol Cell Biol 22:4280–4292
Bulsa M, Urasińska E (2017) Triple negative endometrial cancer. Ginekol Pol 88(4):212–214
Jeffy BD, Hockings JK, Kemp MQ, Morgan SS, Hager JA, Beliakoff J et al (2005) An estrogen receptor-alpha/p300 complex activates the BRCA-1 promoter at an AP-1 site that binds Jun/Fos transcription factors: repressive effects of p53 on BRCA-1 transcription. Neoplasia 7(9):873–882
Arizti P, Fang L, Park I, Yin Y, Solomon E, Ouchi T, Aaronson SA, Lee SW (2000) Tumor suppressor p53 is required to modulate BRCA1 expression. Mol Cell Biol 20:7450–7459
Shu CA, Pike MC, Jotwani AR, Friebel TM, Soslow RA, Levine DA et al (2016) Uterine cancer after risk-reducing salpingo-oophorectomy without hysterectomy in women with BRCA mutations. JAMA Oncol 2(11):1434–1440
Liang SX, Pearl M, Liang S, Xiang L, Jia L, Yang B et al (2011) Personal history of breast cancer as a significant risk factor for endometrial serous carcinoma in women aged 55 years old or younger. Int J Cancer 128(4):763–770
Bland AE, Calingaert B, Secord AA, Lee PS, Valea FA, Berchuck A et al (2009) Relationship between tamoxifen use and high risk endometrial cancer histologic types. Gynecol Oncol 112(1):150–154
Slomovitz BM, Sun CC, Ramirez PT, Bodurka DC, Diaz P, Lu KH (2004) Does tamoxifen use affect prognosis in breast cancer patients who develop endometrial cancer? Obstet Gynecol 104:255–260
Le Donne M, Alibrandi A, Ciancimino L, Azzerboni A, Chiofalo B, Triolo O (2013) Endometrial pathology in breast cancer patients: Effect of different treatments on ultrasonographic, hysteroscopic and histological findings. Oncol Lett 5(4):1305–1310
O'Neill S, O'Driscoll L (2015) Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev 16(1):1–12
Cuzick J, Sestak I, Baum M et al (2010) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol 11:1135–1141
Regan MM, Neven P, Giobbie-Hurder A et al (2011) Assessment of letrozole and tamoxifen alone and in sequence for postmenopausal women with steroid hormone receptor-positive breast cancer: the BIG 1–98 randomised clinical trial at 81 years median follow-up. Lancet Oncol 12:1101–1108
Senkus E, Kyriakides S, Ohno S et al (2015) Primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 26:8–30
National Comprehensive Cancer Network (NCCN) (2015) Clinical Practice Guidelines in Oncology. Breast Cancer, Version 3. [DB/OL]. http://www.nccn.org
Funding
Thanks for the fund support provided by Beijing High-level Health Personnel Training Program (2015-3-090).
Author information
Authors and Affiliations
Contributions
Haili Qian: Data collection. Hua Duan: Data analysis. Jianbin Guo: Manuscript writing. Fei Ma: Providing guidance for revision. Xiujuan Cui: Data analysis. Ying Zhang: project development, Manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guo, J., Zhang, Y., Qian, H. et al. The clinical characteristics and prognosis of endometrial carcinomas that occur after breast cancer: does hormone receptor status of breast cancer matter?. Arch Gynecol Obstet 300, 1399–1404 (2019). https://doi.org/10.1007/s00404-019-05318-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05318-2