Abstract
Purpose
To investigate the occurrence and development state of embryo vacuoles between the 8-cell and morula stages, and to explore how vacuoles affected the development of embryos.
Methods
A retrospective study of a cohort of 422 patients undergoing conventional in vitro fertilization or intracytoplasmic sperm injection. With the help of time-lapse imaging, the development processes and outcomes of good quality embryos with or without vacuoles were analyzed.
Results
Vacuole positive embryos had significantly lower blastulation rate and good quality blastulation rate than vacuole negative embryos, p < 0.05. Compared to vacuole negative embryos, the number of best and good quality blastocysts was significantly reduced, while the number of fair and discarded ones was significantly increased, p < 0.05. The average starting time of vacuolization was 73.7 ± 9.3 h after insemination. The proportion of blastomeres affected by vacuoles was associated with embryonic developmental potential.
Conclusions
Vacuolization on Day 3 and Day 4 was frequently observed and was detrimental to embryo development. The proportion of blastomeres affected by vacuoles may be an indicator of embryo developmental potential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vacuolization is a frequently occurring anomaly during embryo development at any stage. It is known that vacuoles are membrane-bound cytoplasmic inclusions filled with liquid, virtually identical to the liquids found in perivitelline space [1]. Vacuoles have been observed by light [2], electron, and confocal microscopy [3].
Ebner et al. [4] identified three types of vacuoles: those already present at oocyte collection, which may rapidly develop during maturation; those artificially created by an embryologist (ICSI); and those accompanied with developmental arrest. All the three types of vacuoles could be observed in cultured embryos. However, most studies have focused on vacuoles at the oocyte stage, as vacuolization was one of the oocyte morphological abnormalities. Studies have explored whether there was an association between vacuoles, fertilization rate, and developmental competence [4,5,6,7,8]. To our knowledge, few authors have investigated vacuoles accompanied with developmental arrest at the cleavage stage. However, by watching time-lapse videos, we found that vacuolization at the 8-cell to morula stage was more frequent and of greater significance.
The time-lapse monitoring system was widely used in IVF labs for embryo culture and observation. Many publications used the time-lapse monitoring system to predict the developmental potential and ploidy of embryos [9,10,11,12,13,14,15]. We believed that time-lapse technology could help us better understand vacuolization.
The aim of this study was to clarify the occurrence and development state of vacuoles at the 8-cell to morula stage using the time-lapse monitoring system. We also intended to determine which feature of vacuolization could be an indicator of embryo developmental potential.
Materials and methods
Patients
This study included 422 patients with at least one good quality embryo on Day 3 who underwent IVF/ICSI treatment at Center for Reproductive Medicine, Shandong University, from December 2015 to December 2016. All the embryos were cultured in a time-lapse incubator (EmbryoScope, Unisense, Denmark) from Day 0 (insemination day) to Day 6. Of the 422 patients, 119 had at least one good quality embryo showing vacuolization at the 8-cell stage or later.
Oocyte retrieval, embryo culture and embryo transfer
Oocyte retrieval was undertaken by transvaginal ultrasound-guided follicular aspiration 36 h after hCG administration. The cumulus–oocyte complexes (COCs) were kept in culture for 4 h at 37.0 °C and 6.0% carbon dioxide until insemination.
For in vitro fertilization (IVF), COCs were put in contact with spermatozoa for 5 h. Then we observed the polar body of zygotes after removal of granule cells via gentle pipetting. The zygotes were then placed in the time-lapse incubator. For intracytoplasmic sperm injection (ICSI), oocyte denudation was performed in hyaluronidase (80 IU/mL, Irvine Scientific, Santa Ana, CA, USA) via gentle pipetting. Only the metaphase II oocytes were injected. Following insemination, embryos were placed in the time-lapse incubator and cultured in 6% carbon dioxide and 5% oxygen concentrations until Day 5 (D5) or 6 (D6). Sequential culture media (G1 and G2) from Vitrolife (Scandinavian IVF Science, Sweden) was used for embryo culture. The EmbryoScope was programmed to acquire images of each embryo every 15 min through seven different focal planes.
Embryo transfer was conducted on D3 or D5 according to embryo quality and the clinical condition of patients. Following our laboratory guidelines, only vacuole negative, good quality embryos were transferred on D3. The transferred embryos were excluded from the experimental data as they had no further development outcomes. The blastocysts were evaluated and transferred on Day 5 over 4 BC grade in accordance with Garden and Lane’s criteria [16]. Blastocyst quality rather than D3 embryo scoring was used as the evaluation criteria before blastocyst transfer. For frozen embryo transfer (FET) cycles, the vitrified blastocysts were thawed on the morning of the transfer day and cultured for 4–5 h at 37 °C and 6% CO2 before transfer. Only the expanded blastocysts were transferred.
Evaluation of time-lapse imaging and vacuolization
An expert embryologist analyzed the development processes of all the embryos with the help of Embryo Viewer (Unisense, Denmark). Embryos that contained 7–16 cells at 68 ± 1 h post insemination and indicated < 10% fragmentation rate were considered as good quality embryos [17]. In this study, embryos with or without vacuoles were both considered as good quality embryos once they met the above conditions.
Three morphological parameters—inner cell mass (ICM), trophectoderm (TE), and blastocoele expansion and hatching (EH)—were used to evaluate blastocyst quality. Blastocysts were divided into four groups according to the blastocyst scoring system proposed by Gardner and Schoolcraft [18]:
-
Best: EH(4–6), ICM(A) + TE(A)
-
Good: EH(4–6), ICM(A) + TE(B), ICM(B) + TE(A), ICM(B) + TE(B)
-
Fair: EH(4–6), ICM(A) + TE(C), ICM(B) + TE(C)
-
Discarded: EH(3–6), ICM(C) + TE(B), ICM(C) + TE(C); EH(1–2), ICM, and TE without grades; embryos failed to form a blastocoele, or not compacted
Vacuolization was defined as spontaneous vacuole appearance in good quality embryos at the 8-cell stage or later. Embryos with vacuoles before the 8-cell stage were excluded. With the help of time-lapse videos, we could see the occurrence and development state of vacuoles and how they affected the development of embryos. The starting time of vacuolization in each embryo was recorded. The number of blastomeres with or without vacuoles were counted before embryo compacting.
Statistical analysis
Significance of data was assessed by SPSS Statistics 17 software (IBM Inc., New York, NY, USA) using the Student’s t test and the Chi-square test. Differences were considered significant when p values < 0.05.
Results
Of the 422 patients with at least 1 good quality embryo, 119 (28.2%) were found to have vacuoles in the good quality embryos. There was no relationship between vacuolization and parental variables, as shown in Table 1. Embryonic vacuole positive and negative patients were characterized by similar age, basal level of FSH, number of oocytes retrieved, and sperm concentrations. Furthermore, there were no differences in fertilization rates between the two groups.
There were 673 good quality embryos collected from the 119 patients, and 287 of those embryos were vacuole positive. Vacuole positive good quality embryos had a lower blastulation rate and good quality blastulation rate than vacuole negative good quality embryos, p < 0.05, as shown in Table 2.
Out of 170 vacuole positive good quality blastocysts, 8 D5 blastocysts and 37 frozen blastocysts were transferred. Out of the transferred blastocysts, a total of 25 blastocysts (55.6%) were implanted. In contrast, out of 274 vacuole negative good quality blastocyst, 13 D5 blastocysts and 62 frozen blastocysts were transferred, and a total of 40 blastocysts (53.3%) were implanted. However, there was no significant difference between them, as seen in Table 2. Vacuole positive blastocysts seemed to be more likely to result in miscarriage, but the difference was not significant.
Vacuolization reduced blastocyst quality. The number of best and good quality blastocysts was reduced significantly, p < 0.05. Alternatively, the number of fair and discarded blastocysts was increased significantly, p < 0.05, as demonstrated in Table 3.
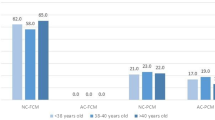
The average starting time of vacuolization was 73.7 ± 9.3 h after insemination. Starting time was not related to embryo quality, as demonstrated in Table 4. The proportion of blastomeres affected by vacuoles was associated with the developmental potential of embryos, as shown in Table 4 and Fig. 1. The more blastomeres affected by vacuoles, the worse the embryo’s development outcome.
Time-lapse images of vacuoles affecting embryo development. From left to right: cleavage stage, morula stage, and blastocyst stage. The vacuoles in each image is pointed out by an arrow. a The proportion of blastomeres affected by vacuoles was low, embryo developed into good quality blastocyst. b The proportion of blastomeres affected by vacuoles was higher, embryo developed into blastocyst of poor quality. c The proportion of blastomeres affected by vacuoles was high, embryo developed into blastocyst to be discarded
Discussion
In this study, we observed using time-lapse imaging that vacuoles affected embryo development competence to a great extent. Among 422 patients with at least 1 good quality embryo, 119 patients (28.2%) were found to suffer from vacuolization in good quality embryos. Ebner et al. [4] showed that 36.6% of their patients had at least one embryo showing at least one vacuole during preimplantation development. The reason their percentage was higher than ours may be that we had different research objects. Ebner et al. [4] investigated vacuolization at every stage of embryo development, including D0, D1, D2–4, and D5, while we only researched embryos at the 8-cell to morula stage. In their study, vacuolization was low at cell stage 2–8, but increased significantly at the compaction stage. That was in accordance with our opinion about vacuolization at the 8-cell to morula stage.
To further explore the adverse effect of vacuolization on embryo development, we thoroughly studied the 119 vacuole positive patients. Among them, there were a total of 673 good quality embryos on D3 (embryos transferred on D3 were excluded), 287 of which were vacuole positive (42.6%). We analyzed the developmental outcomes of the 673 embryos and recorded the scores of the blastocysts. Vacuole positive embryos had a lower blastulation rate and quality of blastulation than vacuole negative embryos. The vacuole positive and negative embryos were all from the same cohort of patients, thus reducing the effect of biases.
In accordance with our laboratory guidelines, we do not transfer vacuole positive cleavage embryos on D3. However, once embryos became blastocysts, the restriction was cancelled. Blastocyst quality was the major factor to be considered regarding transfer. We recorded the implantation rate for a total of 120 blastocysts with or without vacuoles (45 with vacuoles and 75 without vacuoles). Those blastocysts were transferred on D5 or FET. The result showed that the two kinds of blastocysts had a similar implantation rate, but vacuole positive blastocysts tended to have a higher miscarriage rate (16.0% vs 7.5%). One possible explanation was that more blastocysts of low quality and less blastocysts of top quality were transferred in the vacuole positive group than in the vacuole negative group (data not shown), as vacuolization had reduced blastocyst quality. Majumdar et al. [19] found that the euploidy rate was significantly higher for blastocysts with good morphology as compared to those with poor morphology. It has previously been found that embryonic aneuploidy may be responsible for miscarriage [20, 21]. In line with this finding, vacuolization did not reduce the implantation rate of blastocysts, but increased the miscarriage rate. However, the relatively small number of investigated blastocysts may cause the decline in reliability of the data. Thus, further investigation is required.
Since vacuolization had some adverse effects on embryos, we explored how embryo’s development was affected by vacuolization. The embryo development and vacuolization are dynamic, continuous, and complex processes. Counting the number and measuring the size of vacuoles at the special time point was a difficult work that did not necessarily contributed the prediction accuracy of the embryonic potential. We believed that embryos with many vacuoles detected in one blastomere tended to serve as a better outcome indicator than embryos with fewer vacuoles scattered over several blastomeres.
Using time-lapse video, we accurately recorded the beginning times of vacuolization. The present study demonstrated that the average starting time of vacuolization was 73.7 ± 9.3 h after insemination. Suggestively, it indicates that we could miss detection of vacuoles in some embryos when using the inverted microscope. If vacuoles were missed, embryo scorings made 68 ± 1 h after insemination were most likely, also wrongly estimated as high developmental potential. Besides, there was no significant difference found among the four groups of vacuole positive embryos. Thus, the starting time of vacuolization should not be a decisive indicator of embryo developmental potential.
In the present study, we found that the proportion of blastomeres affected by vacuoles and the number of blastomeres participating in compacting were associated with the embryonic potential. As demonstrated in Fig. 1, the more blastomeres were affected by vacuoles, the worse was the developmental embryo outcome. The quality of blastocyst depends on the quality of morula, it was demonstrated that Day 4 morula in classes I–III developed into optimal blastocysts only in 57.4, 50, and 35.6% of the total, respectively [22]. And the quality of morula was determined by the number of blastomeres undergoing the compaction process [22, 23]. Vacuoles might affect the positioning of spindles, cell nucleus and some other cellular structures, thus preventing normal cell division [4, 7, 24]. Such an affected blastomere could not undergo compaction process and will eventually degenerate. Besides this problem, the degenerated blastomeres if located between the intact ones could prevent the formation of correct connection among blastomeres. This may also result in a lack of compaction [25]. Without one or two blastomeres, the embryo can still develop into an intact blastocyst. However, if an embryo had many vacuoles in different blastomeres, the embryo may not be able to develop a functional blastocyst. Even though such an embryo develops into a blastocyst, its score will be low.
There are some limitations found in this study. First, we could not determine the cause of vacuolization and predict the type of embryos that would suffer from vacuolization. Further research is needed to address those problems. Second, the number of embryos transferred was relatively small and the miscarriage rate in two groups may not be persuasive enough. Third, counting the number of blastomeres with or without vacuoles before compacting may be not accurate enough. However, we believed that it still reflects the association between vacuolization and embryo developmental potential.
In conclusion, vacuolization process in embryos at 8-cell stage to morula was quite commonly observed and resulted in detrimental effects on embryo development. We thought that the proportion of blastomeres affected by vacuoles may serve as an indicator of embryo developmental potential. We believe that these data helps better understanding of the vacuolization role in embryo scoring and estimation of embryonic developmental potential on D3 and D4.
References
Van Blerkom J (1990) Occurrence and developmental consequences of aberrant cellular organization in meiotically mature human oocytes after exogenous ovarian hyperstimulation. J Electron Microsc Tech 16(4):324–346. https://doi.org/10.1002/jemt.1060160405
Hardy K, Warner A, Winston RM, Becker DL (1996) Expression of intercellular junctions during preimplantation development of the human embryo. Mol Hum Reprod 2(8):621–632
Hardy K (1999) Apoptosis in the human embryo. Rev Reprod 4(3):125–134
Ebner T, Moser M, Sommergruber M, Gaiswinkler U, Shebl O, Jesacher K, Tews G (2005) Occurrence and developmental consequences of vacuoles throughout preimplantation development. Fertil Steril 83(6):1635–1640. https://doi.org/10.1016/j.fertnstert.2005.02.009
De Sutter P, Dozortsev D, Qian C, Dhont M (1996) Oocyte morphology does not correlate with fertilization rate and embryo quality after intracytoplasmic sperm injection. Hum Reprod 11(3):595–597
Alikani M, Palermo G, Adler A, Bertoli M, Blake M, Cohen J (1995) Intracytoplasmic sperm injection in dysmorphic human oocytes. Zygote 3(4):283–288
Ten J, Mendiola J, Vioque J, de Juan J, Bernabeu R (2007) Donor oocyte dysmorphisms and their influence on fertilization and embryo quality. Reprod Biomed Online 14(1):40–48
Yu EJ, Ahn H, Lee JM, Jee BC, Kim SH (2015) Fertilization and embryo quality of mature oocytes with specific morphological abnormalities. Clin Exp Reprod Med 42(4):156–162. https://doi.org/10.5653/cerm.2015.42.4.156
Meseguer M, Herrero J, Tejera A, Hilligsoe KM, Ramsing NB, Remohi J (2011) The use of morphokinetics as a predictor of embryo implantation. Hum Reprod 26(10):2658–2671. https://doi.org/10.1093/humrep/der256
Kirkegaard K, Kesmodel US, Hindkjaer JJ, Ingerslev HJ (2013) Time-lapse parameters as predictors of blastocyst development and pregnancy outcome in embryos from good prognosis patients: a prospective cohort study. Hum Reprod 28(10):2643–2651. https://doi.org/10.1093/humrep/det300
Desai N, Ploskonka S, Goodman LR, Austin C, Goldberg J, Falcone T (2014) Analysis of embryo morphokinetics, multinucleation and cleavage anomalies using continuous time-lapse monitoring in blastocyst transfer cycles. Reprod Biol Endocrinol 12:54. https://doi.org/10.1186/1477-7827-12-54
Basile N, Nogales Mdel C, Bronet F, Florensa M, Riqueiros M, Rodrigo L, Garcia-Velasco J, Meseguer M (2014) Increasing the probability of selecting chromosomally normal embryos by time-lapse morphokinetics analysis. Fertil Steril 101(3):699–704. https://doi.org/10.1016/j.fertnstert.2013.12.005
Campbell A, Fishel S, Bowman N, Duffy S, Sedler M, Hickman CF (2013) Modelling a risk classification of aneuploidy in human embryos using non-invasive morphokinetics. Reprod Biomed Online 26(5):477–485. https://doi.org/10.1016/j.rbmo.2013.02.006
Minasi MG, Colasante A, Riccio T, Ruberti A, Casciani V, Scarselli F, Spinella F, Fiorentino F, Varricchio MT, Greco E (2016) Correlation between aneuploidy, standard morphology evaluation and morphokinetic development in 1730 biopsied blastocysts: a consecutive case series study. Hum Reprod 31(10):2245–2254. https://doi.org/10.1093/humrep/dew183
Del Carmen Nogales M, Bronet F, Basile N, Martinez EM, Linan A, Rodrigo L, Meseguer M (2017) Type of chromosome abnormality affects embryo morphology dynamics. Fertil Steril 107(1):229–235. https://doi.org/10.1016/j.fertnstert.2016.09.019
Gardner DK, Lane M (1997) Culture and selection of viable blastocysts: a feasible proposition for human IVF? Human Reprod Update 3(4):367–382
Alpha Scientists In Reproductive M (2012) The Alpha consensus meeting on cryopreservation key performance indicators and benchmarks: proceedings of an expert meeting. Reprod Biomed Online 25(2):146–167. https://doi.org/10.1016/j.rbmo.2012.05.006
Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB (2000) Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril 73(6):1155–1158
Majumdar G, Majumdar A, Verma IC, Upadhyaya KC (2017) Relationship between morphology, euploidy and implantation potential of cleavage and blastocyst stage embryos. J Hum Reprod Sci 10(1):49–57. https://doi.org/10.4103/0974-1208.204013
Fragouli E, Wells D (2011) Aneuploidy in the human blastocyst. Cytogenet Genome Res 133(2–4):149–159. https://doi.org/10.1159/000323500
Angell RR, Aitken RJ, van Look PF, Lumsden MA, Templeton AA (1983) Chromosome abnormalities in human embryos after in vitro fertilization. Nature 303(5915):336–338
Ivec M, Kovacic B, Vlaisavljevic V (2011) Prediction of human blastocyst development from morulas with delayed and/or incomplete compaction. Fertil Steril 96(6):1473–1478. https://doi.org/10.1016/j.fertnstert.2011.09.015
Tao J, Tamis R, Fink K, Williams B, Nelson-White T, Craig R (2002) The neglected morula/compact stage embryo transfer. Hum Reprod 17(6):1513–1518
Wallbutton S, Kasraie J (2010) Vacuolated oocytes: fertilization and embryonic arrest following intra-cytoplasmic sperm injection in a patient exhibiting persistent oocyte macro vacuolization–case report. J Assist Reprod Genet 27(4):183–188. https://doi.org/10.1007/s10815-010-9399-2
Alikani M, Cohen J, Tomkin G, Garrisi GJ, Mack C, Scott RT (1999) Human embryo fragmentation in vitro and its implications for pregnancy and implantation. Fertil Steril 71(5):836–842
Funding
This study was funded by The National Key Research and Development Program of China (2017YFC1001000) and The Shanghai Commission of Science and Technology (17DZ2271100).
Author information
Authors and Affiliations
Contributions
ZJY: data management/analysis, manuscript writing/editing. ZWX: data management/analysis, manuscript writing/editing. LH: data collection, manuscript editing. ZHB: data collection, manuscript editing. LM: manuscript editing. MSY: manuscript editing. WKL: project development, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of the Center for Reproductive Medicine, Shandong University.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Zhang, J., Zhong, W., Liu, H. et al. Using time-lapse technology to explore vacuolization in embryos on Day 3 and Day 4. Arch Gynecol Obstet 299, 857–862 (2019). https://doi.org/10.1007/s00404-018-5008-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-5008-x